The pollution of the planet also reaches the breastfeeding ecosystem, one of the most intimate and inviolable that links us as an animal species to the rest of mammals. Nursing mothers may be concerned about whether the quality of their milk will be adequate for their baby and whether environmental pollutants through work, diet, and storing may adversely affect their child. Breast milk is a source of exposure to environmental pollutants, and at the same time it counteracts much of the effects of these exposures. An approach based on the principles of reality and precaution of environmental health to avoid, reduce or eliminate the production and use of harmful chemicals during pregnancy and lactation would improve the human and planetary health for the offspring.
La contaminación del planeta alcanza también al ecosistema de la lactancia, uno de los más íntimos e inviolables que nos liga como especie animal al resto de los mamíferos. Las madres lactantes pueden estar preocupadas sobre si la calidad de su leche será la adecuada para su bebé y si los contaminantes medioambientales, a través del trabajo, la dieta y el envasado, pueden afectar a su hijo desfavorablemente. La leche materna es fuente de exposición a contaminantes medioambientales, y al mismo tiempo contrabalancea muchos de los efectos de estas exposiciones. Un enfoque basado en los principios de realidad y precaución de la salud medioambiental para evitar, reducir o eliminar la producción y el uso de sustancias químicas nocivas durante el embarazo y la lactancia aseguran a la descendencia una mejor salud humana y del planeta.
Human milk is a natural, unique and essential food in the first years of life. We live in a polluted world. Chemical pollution has penetrated every ecosystem in the planet. Environmental pollutants (EPs) can be found in every biological matrix, including human milk. The best way to protect mothers and babies from the risks associated with chemical pollution is to reduce or eliminate production and use of noxious chemical substances, especially during pregnancy and lactation.1–4 In terms of food safety, human milk is the healthiest and least polluted food of the planet, and all children have a right to healthy nutrition free of noxious substances. The scientific literature has evinced the following key aspects2: (a) the deleterious effects of chemical EPs, including drugs, in child health are associated more strongly with prenatal exposure than with exposure through breastmilk; (b) human milk contains protective factors that counteract the effects of exposure to EPs during gestation; (c) tobacco and other environmental pollutants are associated with a shorter duration of breastfeeding (BF) and (d) diet, habits, lifestyles and occupational exposure are the main sources of exposure to EPs. In this article, we discuss the main anthropogenic EPs that may enter the HM ecosystem through occupational exposure, diet and packaging, with an emphasis on recommendations as to how to reduce or eliminate exposure.
Human milk is a natural, unique and essential food in the first years of life. We live in a polluted world. Chemical pollution has penetrated every ecosystem in the planet. Environmental pollutants (EPs) can be found in every biological matrix, including human milk. The best way to protect mothers and babies from the risks associated with chemical pollution is to reduce or eliminate production and use of noxious chemical substances, especially during pregnancy and lactation.1–4 In terms of food safety, human milk is the healthiest and least polluted food of the planet, and all children have a right to healthy nutrition free of noxious substances. The scientific literature has evinced the following key aspects2: (a) the deleterious effects of chemical EPs, including drugs, in child health are associated more strongly with prenatal exposure than with exposure through breastmilk; (b) human milk contains protective factors that counteract the effects of exposure to EPs during gestation; (c) tobacco and other environmental pollutants are associated with a shorter duration of breastfeeding (BF) and (d) diet, habits, lifestyles and occupational exposure are the main sources of exposure to EPs. In this article, we discuss the main anthropogenic EPs that may enter the HM ecosystem through occupational exposure, diet and packaging, with an emphasis on recommendations as to how to reduce or eliminate exposure.
Particular vulnerability to environmental pollutantsAn EP is a factor, agent, substance, compound or combination of the above that alters the composition and equilibrium of human habitats, with the following effects on human health: (a) increased risk of developing mild, moderate and severe diseases; (b) an increase in early mortality or (c) a significant decrease in quality of life. Including drugs, most EPs found in HM are anthropogenic.
There are numerous mechanisms associated with vulnerability5–8:
Infant-dependentAnatomical and physiological immaturity of the infant: all organic systems go through various maturation phases during infancy and childhood, both anatomical (rapid cellular growth with hyperplasia—increase in the number of cells—and hypertrophy—increase in cellular size) and physiological (deficiencies in all physiological systems, especially in immunity and detoxification). Preterm infants are more vulnerable due to their decrease capacity to metabolize and excrete toxic substances.
Increased intestinal absorption in infants: the bulk of the absorption of EPs takes place in the stomach and small intestine. Infants aged less than 6–8 months have a prolonged gastric emptying time lasting up to 6–8 h and a prolonged intestinal transit time, resulting in an increased absorption potential. Children absorb 50% of the lead they ingest, while adults only absorb approximately 10%. Newborn mammals absorb 12% of administered cadmium, while adults of the same species absorb up to 100 times less. Newborns have a higher gastric pH, which can increase or decrease the absorption of certain EPs.
Maternal factors and/or factors related to the characteristics of environmental pollutantsInhibition of milk production or reduction in the milk supply: mainly caused by hormonally active agents, such as dichlorodiphenyltrichloroethane (DDT)/dichlorodiphenyldichloroethylene (DDE) or prolactin inhibitors (ergoline derivatives, oestrogens, anticholinergic drugs, prostaglandins, H1-antihistamines etc.).
High bioavailability in human milk: the bioavailability depends on the route of administration, dose, number of doses and interval between doses.
Higher milk/plasma ratio: the relative concentration of a chemical in milk and plasma is known as the milk-to-plasma (M/P) ratio. The higher the ratio (>1), the greater the concentration of the substance in breastmilk. A ratio of less than 0.25 is indicative of safety in BF. Most drugs used in clinical practice have a M/P ratio that is much smaller than 1, while almost all persistent organic pollutants, such as polychlorobiphenyls or DDT, have M/P ratios near 1 or greater than 1 (Table 1). Pollutants pass to HM more easily if they have the following characteristics:
- •
Low plasma protein binding.
- •
Low molecular weight: pollutants of more than 700–800 Da enter milk in negligible amounts.
- •
High lipophilicity.
- •
Basic pH: readier entry to milk, since the latter has a pH of 7, more acidic compared to plasma, which has a pH of 7.4.
Persistence in milk: depends on the peak or maximum concentration and the half-life of the substance.
Bioaccumulation and biomagnification: when chemical EPs can accumulate, the associated risk increases, as their concentration increases in each trophic level up the food chain, which has humans at the top, so that HM is an indicator of the state of the environment. In this sense, maternal age, parity and lifestyle habits affect the levels of many EPs in breastmilk.
May be active at low doses and have a cocktail effect: the dose-response relationship is not linear, and lower exposure does not always entail a lesser effect, as some endocrine disruptors exhibit higher biological effects at lower doses. Some EPs may act together with an additive or synergistic interaction, possibly enhancing the effect of the exposure to the substances when combined.
Occupational exposure and chemical risk during breastfeedingA growing number of breastfeeding mothers are asking about the potential risks to their children’s health of exposure to occupational pollutants through breast milk. Breastfeeding counterbalances many of the effects of exposure to EPs. Avoiding exposure in mothers reduces the concentration of pollutants in HM and in the offspring. There is evidence of an inverse correlation between exposure to numerous anthropogenic EPs and the duration of BF.9 The thresholds of toxicological concern established for HM are not based on data obtained in vulnerable subsets of the population. Typically, the threshold for safety in pregnancy and breastfeeding is estimated applying uncertainty factors of 10-fold and 100-fold. The scarcity of toxicological data in lactation and pregnancy, the physiological vulnerability of infants to EPs, the uniformity of the diet based on HM and the processes of bioaccumulation and biomagnification are specific factors that must be taken into account in assessing the occupational environmental risk of lactating women.2,9–14 The deficient to non-existent training of occupational health specialists in environmental health and the vulnerability of foetuses and children increases the risk experienced by infants. In this regard, the basic scientific principle used to address chemical risk in the context of breastfeeding is prudence. In case of uncertainty, given the dearth of evidence, the ideal scientific approach to err on the side of caution will protect the health of children. Underestimating risk in paediatric clinical practice contributes to overexposing children to EPs. Children are not small adults. On the contrary, we know that the tissues of embryos and young infants are much more vulnerable to the toxic effects of endocrine disrupters, carcinogens or mutagens. During medical visits, midwives and paediatricians should find out the occupations of parents and explore any potential occupational exposure or concern in relation to BF.
There are specific tools for this purpose that help screen for most EPs that can be encountered in the work setting or the home during BF, such as the “green sheet for pregnancy and breastfeeding”.15
Small doses in these stages of development can have significant and long-lasting effects. We think it is appropriate to consult with nurses, midwives or paediatricians specialised in environmental health if mothers have questions regarding the impact on the offspring of exposures during pregnancy or lactation. Whenever needed, the environmental history-taking can be supplemented with tests to measure the levels of biologic markers of exposure and/or effect.
Table 2 provides some examples of occupations associated with an increased chemical risk during pregnancy that require avoidance of exposure to pollutants from the moment of planning the pregnancy through the end of breastfeeding.16–18 In pregnant and BF women, it is important that the occupational environmental health history be complemented with an environmental risk assessment of the infant performed by a paediatrician specialised in environmental health. Table 3 provides some recommendations for breastfeeding mothers and paediatricians.
Occupations that carry chemical risk in the context of breastfeeding.
| Chemical industry, crude oil derivatives and plastics | Benzene, volatile organic compounds, heavy metals, chrome pigments, crude oil derivatives and plastics, isopropyl alcohol, dyes, bis(chloromethyl) ether, aromatic amines, etc. |
| Agriculture/farming/gardening | Pesticides, herbicides, arsenic derivatives |
| Automotive industry | Solvents, cadmium, polybromides, etc. |
| Glass production | Cadmium, arsenic, etc. |
| Milling and woodworking | Dust, formaldehyde, solvents |
| Construction | Asbestos, PAH |
| Rubber industry | Benzene and aromatic amines |
| Metal industries | Tin manufacturing (PAH, tar) |
| Copper (arsenic) and lead casting | |
| Chrome manufacturing and plating (chromium vi) | |
| Steel and iron manufacturing | |
| Nickel refining (nickel compounds) | |
| Chemical pickling (acid rain with sulfuric acid) | |
| Cadmium refining and manufacturing, production of Ni–Cd batteries, cadmium pigment manufacturing, galvanized cadmium coatings, zinc casting, PVC compounding (cadmium and compounds) | |
| Manufacturing of beryllium and related products y (beryllium and derivatives) | |
| Paint | Solvents, gums, volatile organic compounds, lead, cadmium, etc. |
| Footwear/fur/leather | Solvents, gums, glues (volatile organic compounds), heavy metals, mercury, dyes (benzylanilines, 2-naphthylamine, 4-aminobiphenyl), benzene |
| Plumbing | Metals, solvents, etc. |
| Oil refinery/gas stations/gas | PAH, aliphatic compounds, solvents, benzene, heavy metals, benzopyrenes, aromatic amines, etc. |
| Transportation | Diesel particles, PAH |
| Health care | Nitro compounds, antineoplastics, ethylene oxide, volatile organic compounds (formaldehyde), etc. |
| Hairstyling and/or cosmetology | Dyes and anilines, aromatic nitro compounds, etc. |
| Mining | Heavy metals, uranium, etc. |
| Printing | Volatile organic compounds, cadmium, dyes, etc. |
| Cleaning | Solvents, dry-cleaning agents (trichloroethylene etc.) |
| Other exposure to hazardous substances | Assess risk of other occupations on a case-by-case basis |
PAH, polycyclic aromatic hydrocarbon.
General recommendations for paediatrics clinics regarding working breastfeeding women.
| Precautions | Exercise extreme caution using protective measures (use gloves, gowns and any other necessary elements) |
| Review the datasheets of the chemical substances (request them from prevention services or insurance companies) | |
| If you work with aerosols | Example: hairstylist; improve ventilation and measures to guarantee indoor air quality |
| Protect your home and family | Do not take clothing contaminated with traces of chemicals home |
| Clothing or footwear contaminated in the work setting can be a significant source of parental exposure at home that may interfere with BF. Remember to get changed at work or quickly change after getting home. Wash work clothes separately from the rest of the laundry of your household9 | |
| Talk to your doctor | If you have a chemical safety hazard job, report it from the moment you start planning a pregnancy or get a positive pregnancy test: the department of health of your employer, family physician and paediatrician. As about the actual risks and how to reduce or eliminate them. |
| The infant is the main subject of the risk assessment | An adequate and individualised risk assessment considers the child the main subject of the evaluation. You may need to consult with an environmental paediatrics specialist for guidance |
| Manifestations are frequently subclinical or very mild | It is important to ask about subtle or mild symptoms that improve on weekends and suspect an association with occupational exposure. The presence of these symptoms may be a red flag of significant chemical hazards |
| Collaborate with the employer | If your job entails significant chemical safety hazards, help your employer find alternatives. Frequently, a proactive search identifies alternatives that can be applied to everyday activity by moving the worker to an alternative location or assigning her different tasks during BF |
| Consistency | Avoid other potential exposures. The main chemical hazards for actively employed breastfeeding women are tobacco, alcohol and other drugs |
| It is always the best option | The benefits of BF counteract the effects of exposure to many EPs, so it is important to promote it |
BF, breastfeeding; EP, environmental pollutant.
One of the main risks of BF women who are actively employed is termination of employment, frequently unwarranted. Expanding maternity leave to 2 years would be the most cost-effective strategy to ensure healthier breastfeeding and care of young children.
Dietary recommendationsDiet is the main source of exposure to many EPs in lactating women. Increased consumption of fresh foods, especially vegetables, and decreased consumption of animal fats contribute to lowering the toxic load. Many lipophilic EPs are found in high concentrations in animal fats and processed/ultra-processed foods.2 Consumption of a variety of plant-based foods (fruits, vegetables, greens, legumes, grains), which are the cornerstone of the Mediterranean diet, is recommended. It is particularly important to avoid processed and ultra-processed foods. The benefits of reducing intake of animal-based and processed foods is apparent in every age group, as many chemical toxins are stored in the body, especially in fatty tissue, where they may remain for decades and interfere with hormone signalling at very low doses.
The European Parliament recognizes that consumption of ecological or organic foods may be particularly beneficial for health during pregnancy and breastfeeding.19 Organic foods are those produced through natural processes without use of deleterious chemical substances. Human milk is the nutritional ecosystem that links mankind to all other mammals and is the quintessential sustainable and organic food. Supplying all other foods throughout life through an organic approach guaranteeing a sustainable carbon footprint requires effort on our part to establish a diet richer in organic plant-based foods and free of pesticides in our region. All diets rich in animal-based and ultra-processed foods are unhealthy and carry a higher risk of diseases associated with global development, while diets based on fresh or minimally processed plant-based foods are healthy and have protective effects.20Table 4 lists the chemicals authorised in industrial and ecological farming.19 There is a growing body of evidence on the effects of exposure to pesticides and other toxins from very low doses on neurodevelopment, especially during gestation and in the first years of life. Occupational and at-home exposure during gestation, infancy and childhood are also associated with an increased risk of certain cancers, such as lymphomas and leukaemias, endocrine disruption and neurodevelopmental disorders.16–18
Approved active substances that may be found in the foods consumed by the public.
| In the European Union | For industrial agriculture | For organic agriculture |
|---|---|---|
| Number of approved substances | 389 | 35 |
| Acutely toxic | 102 | 3 |
| Suspected human carcinogenicity | 28 | 0 |
| Germ cell mutagenicity | 2 | 0 |
| Reproductive toxicity (1B + 2) | 29 | 0 |
| Candidates for substitution | 87 | 1 |
Source: European Parliamentary Research Service.19
Increased consumption of ecological foods significantly decreases exposure to pesticides and other chemicals. In children that follow an organic diet, urinary excretion of organophosphorus compounds is up to 9 times smaller.21 The breastmilk of women and other mammals with an organic diet has higher levels of omega-3 fatty acids and other antioxidants, data that support the potential benefits of BF.22 Consumption of organic foods during pregnancy, breastfeeding and early childhood is associated with a decreased risk of allergies and eczema. Cohort studies in the Nordic countries have found that a diet based on organic foods during pregnancy is associated with a 21% decrease in the risk of preeclampsia and a lower risk of urinary tract defects in the offspring.23,24 Other observational studies have found an association between a diet based on organic products and improved outcomes in fertility and a decreased frequency of obesity, metabolic syndrome, allergic eczema, cancer overall and Hodgkin lymphoma in particular.25
Consumption of large marine predators (red tuna, grouper, swordfish, shark, whale, louvar or pike) should be avoided by pregnant women, infants and children aged 1–10 years, restricting intake to a maximum of 120 g per month in children aged 10–14 years. These marine predators accumulate large amounts of mercury that is toxic to the developing brain. Fish is still a very healthy food the consumption of which is recommended. Fish and shellfish contain high-quality protein and other essential nutrients, are low on saturated fats and contain omega-3 fatty acids. Given the broad variety that is commercially available, women and young children in particular should include low-mercury fish or shellfish in their diet due to their considerable nutritional value (dorado, hake, sardine, anchovy, sole etc.).26,27
The composition of HM is fairly stable and the maternal diet only affects some of its nutrients. The fat content of HM changes with diet. The carbohydrate, protein, calcium and iron content does not change much even if the mother eats small amounts of them in her diet. While BF, it is important to avoid a diet that contributes fewer than 1800 calories per day. Maternal weight loss is associated with increased levels of persistent EPs, although the risk-benefit ratio of BF does not change when weight loss does not exceed approximately 0.5 kg/week.28
Storage of human milk and other foods in plastic-free containersA few years ago, the use of plastics containing bisphenol A or phthalates in products meant for packaging or storage of children’s food was banned, including baby bottles and nipples. Table 5 summarises some of the available evidence on the effects of some endocrine disruptors associated with plastic or hygiene products on animal and human health.29 The bisphenol A content is greater in artificial formula compared to human milk.30 This could explain why infants fed HM maintain better values in markers of future fertility.31
Health effects associated with early exposure to plastics and personal hygiene products.
| Laboratory animals | Humans | |
|---|---|---|
| Phthalates | Testicular toxicity | Decreased anogenital distance (marker of androgenization) |
| Abnormalities in male reproductive organs (cryptorchidism, hypospadias y testicular tumours) | Postnatal exposure causes a decrease in free testosterone and changes in humoral immunity | |
| Low birth weight | Associated with rhinitis, eczema, wheezing | |
| Liver tumours | Morphological and cytogenetic abnormalities in sperm | |
| BPA | Decreased fertility | Increased risk of diabetes/metabolic syndrome |
| Neurotoxicity. Stimulates oestrogen receptors in the brain. Prenatal exposure associated with hyperactivity and learning difficulties | Childhood obesity | |
| In pups, early puberty and increased incidence of breast cancer and prostate enlargement | Associated with cardiovascular and liver diseases | |
| Increase in adipocytes | ||
| PBDE | Changes in thyroid function | Decreased intellectual quotient and intellectual disability |
| Neurotoxicity | Associated with cryptorchidism and testicular cancer | |
| PCB | Decreased spermatogenesis | Decreased penile length, delayed sexual maturation, decreased fertility, testicular cancer, hypotonia |
| Delayed puberty | ||
| Behavioural changes (females) | ||
| Parabens (preservatives) | Abnormalities in reproductive system: reproductive organ atrophy, oligospermia, decreased anogenital distance, abnormal anormal breast development | Prenatal exposure and birth weight |
BPA, bisphenols A; PBDE, polybrominated diphenyl ethers; PCB, polychlorobiphenyls.
Lipophilicity and heat increase the leaching of substances into plastic polymers. The 5 plastic polymers used most widely to make containers are polyethylene (PE), polypropylene (PP), polyethylene terephthalate, polystyrene and polyvinyl chloride.32–34
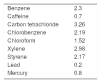
Polypropylene is the plastic used most frequently in the manufacture of containers and packaging for infant food. There is research and evidence of chemicals having leached into PP infant bottles and infant food packaging, including alkanes (in more than 65%) and benzene derivatives (17%), and some plasticizers, esters, antioxidants and other substances have been detected regularly.33 As for the presence of phthalates, traces of diethyl phthalate, diisobutyl phthalate, dibutyl phthalate and bis(2-ethylhexyl) phthalate have been detected in some packaging.
There is a growing body of evidence from studies that prove the lixiviation of chemicals, and plastics can be considered persistent pollutants. This is because most of them are not biodegradable. Polyethylene terephthalate and PP are the plastics used most commonly in paediatrics, can be considerable nonbiodegradable and are frequently used for single-use disposable products.35 Usually, their degradation consists in their fragmentation into smaller polymers. In this way, they end up polluting different ecosystems, this degradation/fragmentation process is the source of microplastics pollution. Microplastics pose one of the greatest threats to the health of seas and oceans worldwide. At present, the recycling rate for plastics by consumers worldwide ranges from 1% to 10%.36
The use of glass, stainless steel or ceramic to store, heat or pasteurise HM reduces exposure to chemical pollutants in the milk, thus contributing to human health and the health of the planet. It also promotes social innovation and the development of biotechnology by businesses (Table 6). In the Region of Murcia, the regional human milk bank located at the Hospital Clínico Universitario Virgen de la Arrixaca has set the standard of using glassware in every process.
Advantages and disadvantages of using glass versus plastic containers to store human milk.
| Advantages | Disadvantages | |
|---|---|---|
| Glass containers and bottles | Sustainable material | Heavier |
| Can break | ||
| Reusable/recyclable | ||
| Free of chemicals | ||
| Compatible with breast pumps | ||
| Long-lasting | ||
| Does not alter the taste of the contents | ||
| Does not absorb odours | ||
| Allows full sterilization | ||
| Easy to clean | ||
| Promotes local industry and innovation | ||
| Low carbon footprint | ||
| Protects the health of the planet | ||
| Plastic containers and bottles | Lighter | Chemical components that are released with heat and prolonged use |
| Hard to break | Porous material that harbours bacteria and is harder to clean | |
| Cannot be fully disinfected | ||
| Heat releases the toxic substances | ||
| The material can change with freezing | ||
| It absorbs and transmits odours | ||
| Less durable; wears out | ||
| Lipids and vitamins adhere to the walls | ||
| High carbon footprint | ||
| Promotes the culture of garbage |
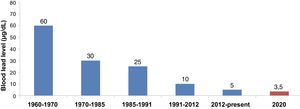
Communities that live on contaminated soil may be exposed to high lead levels and other pollutants in the air, in pit lakes holding waste from mining or metallurgy and on the ground, in non-residential settings.37 Lead is a neurotoxin for which there is no known level in blood that does not have an effect. Fig. 1 provides an example of the decreasing trend in the levels considered safe as the body of evidence grew.35 At present, the Committee on Environmental Health of the AEP is studying the possibility of proposing lowering the action level by 3–3.5 μg/dL based on emerging evidence on the nephrotoxicity and impact on development of lead exposure.38–40 Performance of a blood lead test is recommended in individuals residing in areas with contaminated soil, especially during childhood, pregnancy and lactation. The AEP does not recommend measurement of lead levels in breastmilk for the purpose of clinical decision-making. The studies in the literature have found higher levels of lead in artificial formula compared to human milk.41 Establishment of BF must be promoted while monitoring infants born to mothers with levels of 3.5 μg/dL or greater. In case of clinical toxicity in mothers (levels >40 μg/dL), we recommend discarding the milk until the levels decrease. Consult with a paediatrician with experience in environmental health.
Closing reflectionsIn the Anthropocene era, breastmilk technically is neither a drug nor a health care product and it is also not subject to the legislation on chemical food safety applied to artificial substitutes. And while it continues to be the healthiest, safest and least contaminated food for children on earth in terms of food safety, it is still a fragile ecosystem that requires environmental protection. In a fragmented and increasingly polluted world, it is urgent that we take into account the presence of EPs in HM and develop strategies for standardising and monitoring EP levels to protect the ecology of HM. Determination and a new ecological awareness will be needed in paediatricians of the 21st century to guarantee the preservation of this extremely necessary and delicate ecosystem for future generations.
All children have the right to healthy nutrition free of anthropogenic EPs. As paediatricians, we have the moral authority and scientific acumen to demand that governments prioritise clean food and a clean environment, including the HM ecosystem, which would require encouraging and supporting collective interventions aimed at promoting BF, reducing chemical pollution, enacting regulations such as the Registration, Evaluation, Authorization and Restriction of chemical substances and mixtures to prevent contamination and take advantage of donor human milk banks to develop standards and monitoring guidelines to preserve the ecological niche of HM.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Ortega-García JA, Aguilar-Ros E, Ares-Segura S, Agüera-Arenas JJ, Pernas-Barahona A, Sáenz de Pipaón M, et al. Exposiciones laborales, dieta y envasado: recomendaciones para reducir los contaminantes medioambientales en la lactancia materna. An Pediatr (Barc). 2021;94:261–261.