The Practices in Emergency and Rescue medication For Epilepsy managed with Community administered Therapy (PERFECT™) Initiative was set up in 2011 to gain a better understanding of how prolonged convulsive seizures are managed, and rescue medication is administered, in out-of-hospital settings across Europe. This paper explores the initial research findings for Spain.
Material and methodsA review was made of existing clinical guidelines, guidance to schools, and relevant policy and legal frameworks, as well as a survey of 20 healthcare professionals who treat children with prolonged convulsive seizures in Spain.
ResultsExisting clinical guidelines pertain mainly to the hospital setting, and contain very little information on how prolonged seizures should be managed outside of the hospital. Guidance for schools is unclear as to whether teachers are allowed to administer rescue medication to children, and there is no legal obligation for school staff to administer medication to children under their care. As a result of such uncertainty, whether or not children who experience prolonged seizures receive their rescue medication during school hours depends mostly on the resources and training available in each school.
ConclusionsThere is a need for more explicit guidance covering educational and healthcare settings, clearer information to parents and schools, and more systematic training to be made available to caregivers. This is to ensure that all children at risk of a prolonged convulsive seizure receive rescue medication in a timely manner, regardless of where their seizure occurs.
La Iniciativa Practices in Emergency and Rescue medication For Epilepsy managed with Community administered Therapy (PERFECT™) se inició en 2011 con el objetivo de conocer mejor cómo se tratan las crisis convulsivas prolongadas y cómo se administra la medicación de rescate en la comunidad en Europa. Este artículo analiza sus resultados iniciales en España.
Material y métodosRevisión de las guías clínicas, guías para colegios y marco legal relevante sobre el tratamiento de las crisis convulsivas prolongadas y una encuesta a 20 profesionales sanitarios que tratan a niños con crisis convulsivas prolongadas en España.
ResultadosLas guías clínicas existentes abordan principalmente el ámbito hospitalario y contienen poca información sobre cómo deben tratarse las crisis convulsivas prolongadas en la comunidad. Las recomendaciones para los colegios no son claras respecto a si los profesores, que no tienen la obligación legal de administrar la medicación de rescate a los niños que tienen a su cargo, pueden o deben administrarla. Esta incertidumbre determina que la administración de medicación de rescate al niño con una crisis convulsiva prolongada durante el horario escolar dependa los recursos y de la formación disponibles en cada colegio.
ConclusionesEs necesario contar con guías explícitas que aborden los ámbitos educativo y sanitario, información más clara para padres y colegios, y formación más sistemática a disposición de los cuidadores. Ello facilitará que todos los niños con riesgo de presentar crisis convulsivas prolongadas reciban el tratamiento de rescate apropiado, independientemente del lugar en el que ocurra la crisis.
Epilepsy affects approximately 360,000 people in Spain, with an annual incidence of 62.6 cases per 100,000 children.1,2 Among the population with active epilepsy, 25% are children, and although most have brief, self-limited epileptic seizures, there is a subgroup with a predisposition to prolonged convulsive seizures, defined as those that last for more than 5min. In these children seizures are less likely to stop spontaneously unless emergency treatment is administered promptly.3 Delays in administering it are associated with a higher risk of evolving into convulsive status epilepticus. This complication occurs in 10–20% of children with epilepsy at some point in their illness and can require admission to the intensive care unit and lead to the development of neurocognitive sequelae.4–7 It is therefore essential to ensure that children with prolonged convulsive seizures receive rescue medication as quickly as possible, regardless of where their seizure occurs.
Most seizures occur in the community, and therefore administration of rescue medication will depend on the presence of a trained caregiver with access to the drug. Rescue medication is administered in the home by parents, while in special education schools there is commonly a nurse present who assumes this responsibility. On the other hand, in ordinary schools parents have to delegate this responsibility to teaching staff with no specific healthcare training for this purpose.
Benzodiazepines are the first-line emergency treatment and their route of administration will depend on the setting in which the child is treated. The intravenous route is the most effective and is the route of choice in the hospital setting, but in the community the transmucosal route commonly has to be used.6 Rectal diazepam is effective in stopping prolonged convulsive seizures and is the most widely used transmucosal benzodiazepine in Spain. However, the perception exists that appropriate application of emergency treatment in the community is limited in practice by a lack of information on how, when and by whom it has to be administered.
There is little published data on how prolonged convulsive seizures are treated in schools or other areas of the community in Spain and the situation is believed to vary according to the resources and staff available in each school.8 The PERFECT™ initiative (standing for Practices in Emergency and Rescue medication For Epilepsy managed with Community administered Therapy) began in 2011 with the intention of finding out how prolonged convulsive seizures are treated in the community in various European countries and identifying points where there was room for improvement. In the following pages we present some of its results in Spain and establish recommendations for improving care of children with prolonged convulsive seizures in the community, with special emphasis on the school setting.
MethodsThe PERFECT™ initiative includes 3 phases carried out in 6 European countries (France, Italy, Germany, Spain, Sweden and the United Kingdom). Phase 1 consisted of a review of the clinical and non-clinical guidelines regulating the treatment of prolonged convulsive seizures. Phase 2 comprised a qualitative survey addressed to healthcare professionals on their perception of care of children with prolonged convulsive seizures in the community. Phase 3 will consist of a survey of children and caregivers on their experience with prolonged convulsive seizures in the community. The results of Phase 1 have been published at European level, those of Phase 2 are in press and those of Phase 3 will be published at the beginning of 2014.8 This article presents the results of Phases 1 and 2 in Spain.
For the review of clinical guidelines and non-clinical guidance (Phase 1), searches were carried out in Spanish and English in the medical literature indexed in PubMed, as well as websites of professional associations and patients’ organisations, for relevant clinical guidelines and care protocols. The legal framework governing treatment of prolonged convulsive seizures in educational institutions was also reviewed.
The survey of healthcare professionals (Phase 2) was conducted between March and April 2012 and consisted of a 45-min telephone survey in Spanish. The respondents were 15 neuropaediatricians and 5 paediatricians from Spanish public and private hospitals, the intention being to provide a representative sample of specialists involved in treating children with prolonged convulsive seizures in Spain. The participants were selected using a method of freely searching in various Spanish hospitals. They had to be physicians who devoted more than 10% of their time to the care of children with epilepsy, including at least 5 children per month requiring emergency treatment for prolonged convulsive seizures. A market research company, Insight Research Group, conducted the survey. All the results were obtained anonymously.
The committee of experts of the PERFECT™ initiative, composed of leading European epileptologists, played a part in identifying significant sources of information in participating countries and in consultations with local patients’ organisations and professional associations, as well as in developing the questionnaire for healthcare professionals.8
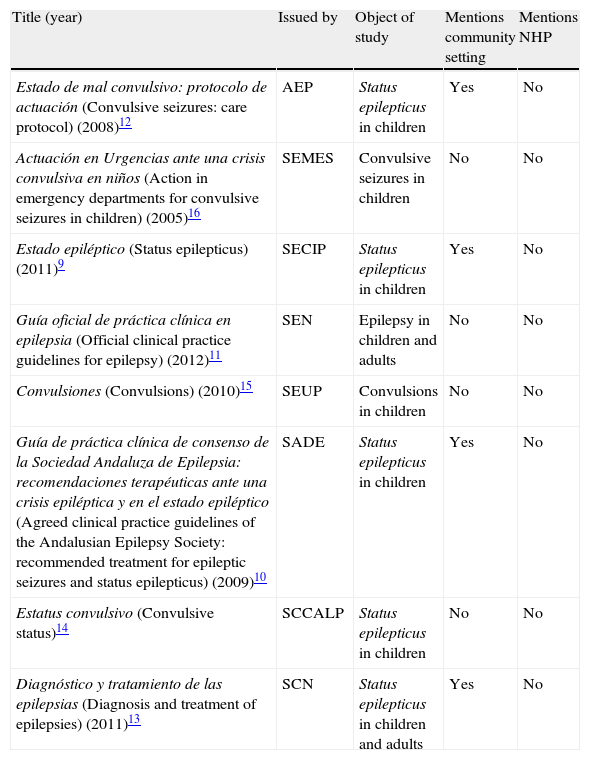
ResultsClinical guidelinesThe existing Spanish clinical guidelines on the treatment of prolonged convulsive seizures contain very little information on how such seizures should be treated in the community (Table 1). The guidelines of the AEP (Spanish Association of Paediatrics) and of other national and regional scientific societies recommend administration of rectal diazepam but do not mention anything about parents, teachers or other caregivers having to receive specific training to administer it or having to follow a protocol specified in advance. Other guidelines confine themselves to establishing recommendations for the hospital setting without even mentioning treatment in the community.9–16
Recent clinical guidelines on the treatment of prolonged convulsive seizures in children.
| Title (year) | Issued by | Object of study | Mentions community setting | Mentions NHP |
| Estado de mal convulsivo: protocolo de actuación (Convulsive seizures: care protocol) (2008)12 | AEP | Status epilepticus in children | Yes | No |
| Actuación en Urgencias ante una crisis convulsiva en niños (Action in emergency departments for convulsive seizures in children) (2005)16 | SEMES | Convulsive seizures in children | No | No |
| Estado epiléptico (Status epilepticus) (2011)9 | SECIP | Status epilepticus in children | Yes | No |
| Guía oficial de práctica clínica en epilepsia (Official clinical practice guidelines for epilepsy) (2012)11 | SEN | Epilepsy in children and adults | No | No |
| Convulsiones (Convulsions) (2010)15 | SEUP | Convulsions in children | No | No |
| Guía de práctica clínica de consenso de la Sociedad Andaluza de Epilepsia: recomendaciones terapéuticas ante una crisis epiléptica y en el estado epiléptico (Agreed clinical practice guidelines of the Andalusian Epilepsy Society: recommended treatment for epileptic seizures and status epilepticus) (2009)10 | SADE | Status epilepticus in children | Yes | No |
| Estatus convulsivo (Convulsive status)14 | SCCALP | Status epilepticus in children | No | No |
| Diagnóstico y tratamiento de las epilepsias (Diagnosis and treatment of epilepsies) (2011)13 | SCN | Status epilepticus in children and adults | Yes | No |
AEP: Asociación Española de Pediatría (Spanish Association of Paediatrics); NHP: non-healthcare professionals; SADE: Sociedad Andaluza de Epilepsia (Andalusian Epilepsy Society); SCCALP: Sociedad de Pediatría de Asturias, Cantabria, Castilla y León (Paediatrics Association of Asturias, Cantabria and Castilla y León); SCN: Societat Catalana de Neurologia (Catalan Neurology Society); SECIP: Sociedad Española de Cuidados Intensivos Pediátricos (Spanish Paediatric Intensive Care Society); SEMES: Sociedad Española de Medicina de Emergencias (Spanish Emergency Medicine Society); SEN: Sociedad Española de Neurología (Spanish Neurology Society); SEUP: Sociedad Española de Urgencias Pediátricas (Spanish Paediatric Emergencies Society).
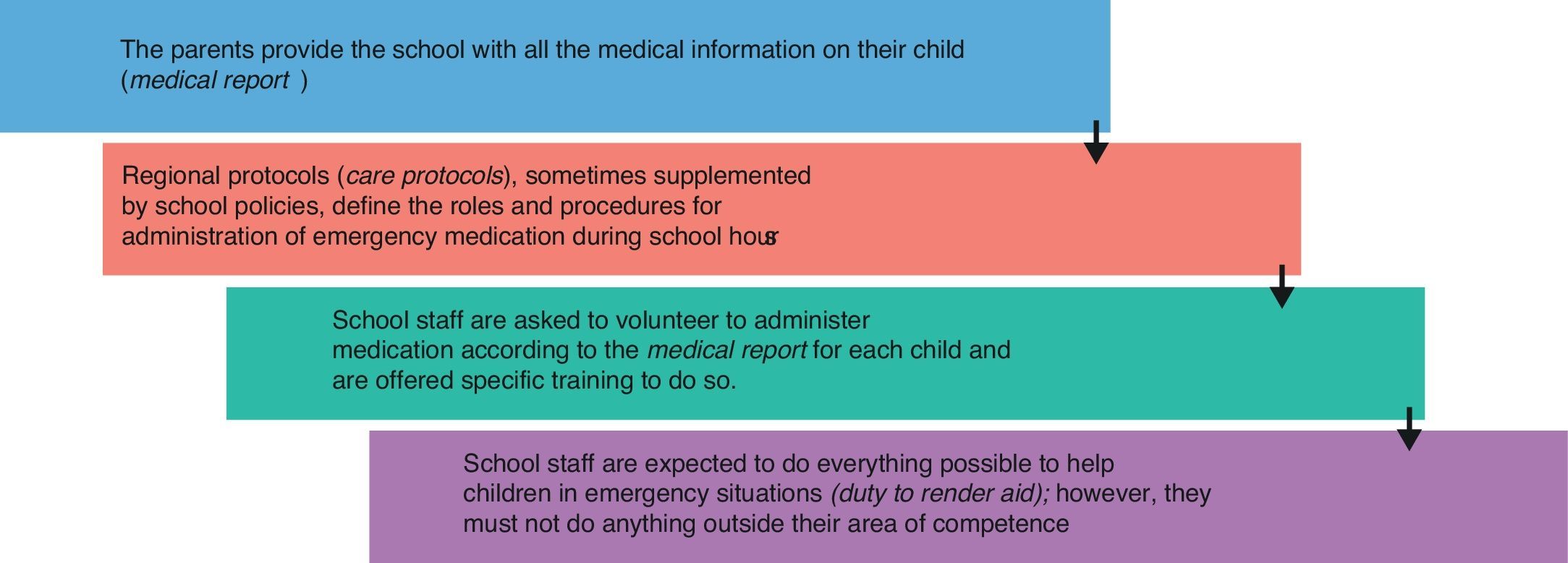
In Spain, responsibility for education and health is devolved to the autonomous communities and references to emergency treatment differ from one autonomous community to another and are spread over documents that regulate different areas (e.g. treatment of chronic illnesses in schools, management of emergency situations). Existing care protocols in some autonomous communities are conceived to serve as a framework of understanding among the various parties involved in treating children in the community and many of these protocols describe the chain of care for children who require administration of medication in school.17–19 The guidelines are of a general nature and applicable to many illnesses and the section devoted to prolonged convulsive seizures is very brief or non-existent. Although they differ in certain respects, the general process recommended in the care protocols is shown in Fig. 1. There is a national precedent for the care protocols in the form of a report issued by the Legal Services of the Department of Education of the Junta de Andalucía (Andalusian regional government) in 1997; however, it does not seem to have had much influence in practice.20 The basic principles set out in the report are included in the care protocols: schools must adapt to ensure that the medical needs of pupils during school hours are met and teachers are not legally obliged to administer any medicine to children and must not do so if it requires skills beyond those expected of them as educators.
Procedure for administration of rescue medication to children during school hours, according to the recommendations of the care protocols.17–20.
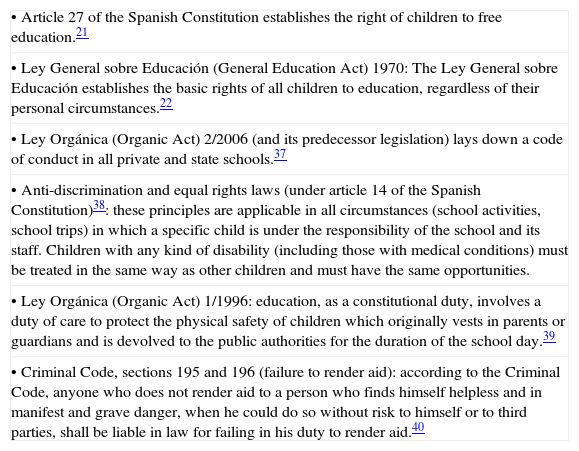
Another point investigated in Phase 1 was the legal framework for the administration of medication in schools (Table 2). The right of all children to free education regardless of their state of health is enshrined in the Spanish Constitution (article 27), as well as the right to non-discrimination in terms of admission to schools and participation in all school activities (article 14).21,22
Legal framework for the rights of children requiring rescue medication in schools.
| • Article 27 of the Spanish Constitution establishes the right of children to free education.21 |
| • Ley General sobre Educación (General Education Act) 1970: The Ley General sobre Educación establishes the basic rights of all children to education, regardless of their personal circumstances.22 |
| • Ley Orgánica (Organic Act) 2/2006 (and its predecessor legislation) lays down a code of conduct in all private and state schools.37 |
| • Anti-discrimination and equal rights laws (under article 14 of the Spanish Constitution)38: these principles are applicable in all circumstances (school activities, school trips) in which a specific child is under the responsibility of the school and its staff. Children with any kind of disability (including those with medical conditions) must be treated in the same way as other children and must have the same opportunities. |
| • Ley Orgánica (Organic Act) 1/1996: education, as a constitutional duty, involves a duty of care to protect the physical safety of children which originally vests in parents or guardians and is devolved to the public authorities for the duration of the school day.39 |
| • Criminal Code, sections 195 and 196 (failure to render aid): according to the Criminal Code, anyone who does not render aid to a person who finds himself helpless and in manifest and grave danger, when he could do so without risk to himself or to third parties, shall be liable in law for failing in his duty to render aid.40 |
Education legislation also protects the right to health in the school setting. Teachers must look after children and according to the Criminal Code they could be legally liable for failure to render aid if they did not intervene to assist a pupil in a life-threatening situation.
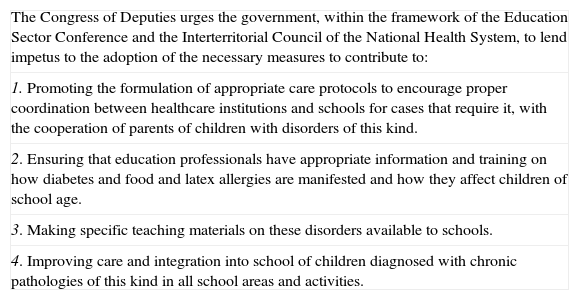
The legislation does not specifically refer to children with epilepsy and its interpretation depends on each individual case. On the other hand, there is an important precedent in diabetes. In 2010 a non-binding parliamentary resolution was passed urging the Spanish government to improve the integration of children with diabetes into schools.23 Although the principles contained in that resolution could be applicable to children with epilepsy or other chronic illnesses there is no sign of it being applied more widely (Table 3).
2010 non-binding parliamentary resolution to improve the care of children with diabetes and food and latex allergies in school settings.23
| The Congress of Deputies urges the government, within the framework of the Education Sector Conference and the Interterritorial Council of the National Health System, to lend impetus to the adoption of the necessary measures to contribute to: |
| 1. Promoting the formulation of appropriate care protocols to encourage proper coordination between healthcare institutions and schools for cases that require it, with the cooperation of parents of children with disorders of this kind. |
| 2. Ensuring that education professionals have appropriate information and training on how diabetes and food and latex allergies are manifested and how they affect children of school age. |
| 3. Making specific teaching materials on these disorders available to schools. |
| 4. Improving care and integration into school of children diagnosed with chronic pathologies of this kind in all school areas and activities. |
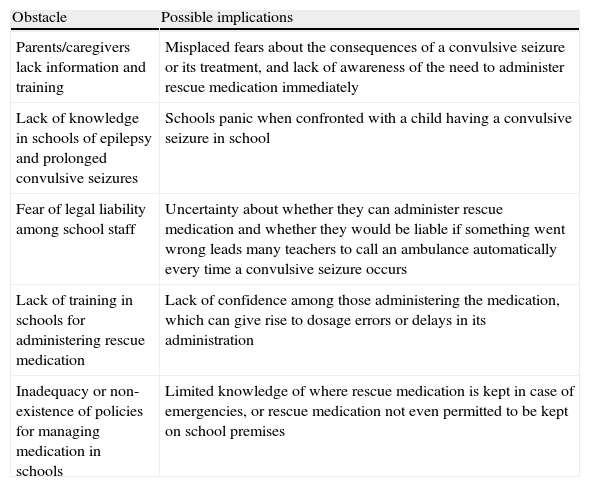
The physicians interviewed during Phase 2 were not very aware of how convulsive seizures are treated in community settings, especially in schools. They recognised the importance of training school staff to be able to administer rescue medication to children when they need it, but they indicated that they did not have time to interact with schools directly and rarely took part in that training, leaving the task to parents. They had the impression that when confronted with a child suffering a prolonged convulsive seizure most teachers panicked, a reaction fed by a lack of information on epileptic seizures, a lack of information on how to treat them, uncertainty about their rights and obligations, and fear of legal liability in the event of complications (Table 4). They estimated that between 20% and 100% of schools called an ambulance every time a child had a prolonged convulsive seizure during school hours.
Main obstacles to optimum emergency treatment in the community according to the healthcare professionals surveyed.
| Obstacle | Possible implications |
| Parents/caregivers lack information and training | Misplaced fears about the consequences of a convulsive seizure or its treatment, and lack of awareness of the need to administer rescue medication immediately |
| Lack of knowledge in schools of epilepsy and prolonged convulsive seizures | Schools panic when confronted with a child having a convulsive seizure in school |
| Fear of legal liability among school staff | Uncertainty about whether they can administer rescue medication and whether they would be liable if something went wrong leads many teachers to call an ambulance automatically every time a convulsive seizure occurs |
| Lack of training in schools for administering rescue medication | Lack of confidence among those administering the medication, which can give rise to dosage errors or delays in its administration |
| Inadequacy or non-existence of policies for managing medication in schools | Limited knowledge of where rescue medication is kept in case of emergencies, or rescue medication not even permitted to be kept on school premises |
One of the main difficulties in implementing the existing guidelines is that they contain contradictions as to whether carers without specific training in administering emergency treatment should assume this responsibility in schools. The 1997 report by the Legal Services of the Department of Education of the Junta de Andalucía (Andalusian regional government) and many of the various autonomous communities’ care protocols indicate that teachers can only administer medication if this does not require specific training. Other guidelines indicate that teachers can administer medicines provided they comply with the child's medical report and provided the family and competent school authority sign a clear protocol describing the procedure to be followed.17 One point on which the various guidelines do agree is that any injectable medication must only be administered by a healthcare professional.
Some teachers’ associations have suggested that asking teachers to administer rescue medication is unwise and that teachers should not be expected to assume responsibilities outside what is required of them as educators.24
DiscussionThe review of guidelines and legal framework, as well as the survey of healthcare professionals, in Phases 1 and 2 of the PERFECT™ initiative highlight important limitations in the care of children with prolonged convulsive seizures in community settings in Spain. These results will need to be compared with those to be obtained directly from families in Phase 3 of the study, but they already indicate a need to introduce improvements at various points in the chain of care for these children.
The clinical guidelines do not offer practical guidance on the need for training or the conditions for authorising caregivers to administer rescue medication. Recommendations to schools as to whether teachers can administer rescue medication to children are ambiguous and contradictory. On the one hand, the law protects the right to health of children with epilepsy during school hours; on the other, there is no legal obligation for teaching staff to administer medication to children under their care. The result of this contradiction is often that rescue medication is not administered and an ambulance is called when a child has a prolonged convulsive seizure in school. This leads to delay in administering treatment and a consequent risk of morbidity, and it contributes to stigmatising the children affected and limiting their social integration.6,25
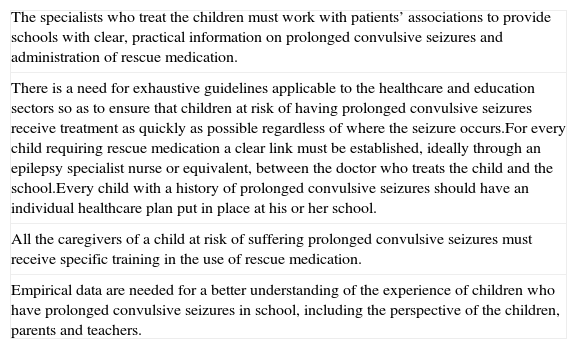
Many of these problems are common to other countries, and Table 5 lists some of the recommendations of the committee of experts of the PERFECT initiative for improving the care of children with prolonged convulsive seizures.8 More exhaustive guidelines are needed covering both healthcare and educational areas. As well as specifying the indicated treatment, these guidelines ought to make explicit recommendations on the role of teachers and caregivers in schools. A special role should also be introduced to facilitate interaction between the two areas, as happens in the United Kingdom and Sweden, where epilepsy specialist nurses play this role; unfortunately, that is not the case in Spain, and the person who assumes this function varies from child to child.
Recommendations for improving care of children with prolonged convulsive seizures in schools.
| The specialists who treat the children must work with patients’ associations to provide schools with clear, practical information on prolonged convulsive seizures and administration of rescue medication. |
| There is a need for exhaustive guidelines applicable to the healthcare and education sectors so as to ensure that children at risk of having prolonged convulsive seizures receive treatment as quickly as possible regardless of where the seizure occurs.For every child requiring rescue medication a clear link must be established, ideally through an epilepsy specialist nurse or equivalent, between the doctor who treats the child and the school.Every child with a history of prolonged convulsive seizures should have an individual healthcare plan put in place at his or her school. |
| All the caregivers of a child at risk of suffering prolonged convulsive seizures must receive specific training in the use of rescue medication. |
| Empirical data are needed for a better understanding of the experience of children who have prolonged convulsive seizures in school, including the perspective of the children, parents and teachers. |
The need to administer rescue medication rapidly in order to avoid progression to status epilepticus and its complications must be brought to the attention of everyone involved in the chain of care for children with epilepsy, from the specialists who prescribe the rescue medication to all the settings in which children at risk may experience a prolonged convulsive seizure. Having clear recommendations may make it easier for parents to convey their needs to schools and schools to be provided with the appropriate resources. This information must be an integral part of an overall effort to promote understanding of epilepsy in general. For example, the campaign entitled Conocer la epilepsia nos hace iguales (Knowing about epilepsy makes us equal), which was launched in 2011 and has reached over 25,000 children in 2000 schools all over Spain, has contributed to fostering awareness of epilepsy in schools and has provided guidance on what to do in the event of a convulsive seizure occurring in school. However, the campaign does not make specific reference to prolonged convulsive seizures or to their treatment.26
Paediatricians have an obligation to identify children at risk of suffering a prolonged seizure and to instruct their parents in the administration of emergency medication. Providing parents with rescue medication reduces their fears for the safety of their children, and administering treatment at home, as well as limiting the morbidity of prolonged seizures, may reduce ambulance calls, emergency department visits, and hospital admissions, with the resulting decrease in costs.27,28 Even in patients for whom the treatment does not stop the seizure, its administration seems to make seizures easier to control subsequently in the hospital setting.6 However, some paediatricians are reluctant to prescribe rescue medication for children at risk of suffering prolonged convulsive seizures for fear of respiratory depression which is a side effect of treatment. Respiratory depression associated with the administration of transmucosal benzodiazepines occurs in 5% of cases, whatever the route of administration, but increases significantly after administration of more than 2 doses of benzodiazepines.6,7,29 This must be weighed against the consequences of progression to status epilepticus and the risk of respiratory depression directly attributable to the seizure. In the benchmark study by Alldredge et al.,30 the incidence of respiratory depression in adults suffering a prolonged convulsive seizure was greater in those who received a placebo than in those treated with lorazepam or diazepam intravenously. However, the prescription of emergency treatment cannot be indiscriminate and must be limited to children with an objective risk of prolonged convulsive seizures. A history of prolonged seizures is the main risk factor, and the United Kingdom NICE guidelines limit the prescription of rescue medication to children who have had a previous episode.31
An important consideration is that the only transmucosal benzodiazepine marketed in Spain so far has been rectal diazepam, which presents obvious problems of social acceptance when it is to be administered in the community by non-healthcare staff. Rectal administration and the need to undress the child make many teachers uncomfortable and represent an additional limitation to achieving appropriate emergency treatment in schools. Perhaps the reluctance of schools to administer rescue medication may be partly solved by the availability of benzodiazepines that are easy to administer and socially acceptable, such as buccal or intranasal midazolam, which are preferred by patients and their caregivers.32,33 Buccal midazolam, which has recently been approved for use in Spain for the treatment of prolonged convulsive seizures in children between the ages of 3 months and 18 years, has been shown in some studies to be more efficacious and cost-effective than rectal diazepam.29,34,35 Indeed, the Cochrane guidelines on the treatment of convulsive status epilepticus in children conclude that buccal midazolam is the treatment of choice for children in whom venous access is not possible, and in the United Kingdom, for example, buccal midazolam is now more frequently prescribed than rectal diazepam. 32,36
In conclusion, we need guidelines containing explicit information for parents and schools about the indicated emergency treatment; the ambiguities over administration of treatment in schools must be resolved and caregivers must be trained so that children with prolonged convulsive seizures receive appropriate emergency treatment. Achieving this requires collaboration between the healthcare and education systems, and the existing care protocols are a first step towards that objective. Extending the principles of the non-binding parliamentary resolution on integration of children with diabetes into schools to children with epilepsy requiring rescue medication would represent an important step forward for this vulnerable group of children.
Conflicts of interestM. Raspall-Chaure, A. Martínez-Bermejo, R. Sánchez-Carpintero and S. Wait have received fees from ViroPharma as consultants in the past.
Please cite this article as: Raspall-Chaure M, Martínez-Bermejo A, Pantoja-Martínez J, Paredes-Carmona F, Sánchez-Carpintero R, Wait S. Manejo de la crisis convulsiva prolongada en la comunidad: resultados del estudio PERFECT en España. An Pediatr (Barc). 2014;81:99–106.