Leucoencephalopathy with brain stem and spinal cord involvement and lactate elevation is a rare disease that affects the white matter of the brain of which fewer than a hundred cases have been described. The onset of symptoms usually occurs during childhood or adolescence and is characterised by slowly progressing cerebellar ataxia, spasticity and dysfunction of the dorsal column of the spinal cord. Its diagnosis is based on the abnormalities found in magnetic resonance imaging (MRI) and spectroscopy. It follows a pattern of autosomal recessive inheritance and caused by mutations in the DARS2 gene.
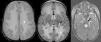
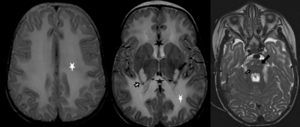
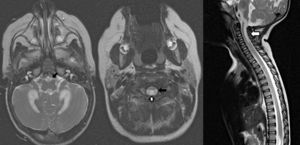
We present the cases of two female twins aged 14 months, born preterm at 32 weeks’ gestation to consanguineous parents, and referred for evaluation due to failure to thrive. They were followed up in the clinic, exhibiting mild psychomotor delay at age 9 months. At 14 months they were admitted for evaluation of severe malnutrition. The neurological assessment revealed psychomotor regression with absence of sitting and turning, irregular eye focusing and tracking, and little interest in objects. A metabolic and nutritional screening was performed, revealing a mild elevation of lactate in blood. The findings of brain and spinal cord MRI were compatible with severe, uniform diffuse involvement of the periventricular, centrum semiovale, and cerebellar peduncle white matter. There was involvement of the posterior and anterior regions of the corpus callosum, the corticospinal tracts from the posterior limb of the internal capsule through the brain stem to the lateral corticospinal tracts in the spinal cord and of the ascending tracts from the dorsal columns of the cervical spinal cord and medial lemniscus of the brain stem to the thalamus and corona radiata (Figs. 1 and 2). We performed a magnetic resonance spectroscopic imaging (MRSI) scan that revealed a decreased N-acetyl aspartate/creatine ratio and lactate elevation. The disease progressed slowly in both twins, with gradual neurological deterioration and recurrent respiratory infections leading to their death at age 2 years.
Transversal T2-weighted images showing extensive involvement of the periventricular, deep and cerebellar white matter (white asterisks). Involvement of the corpus callosum (black asterisks) and the corticospinal tract, from the posterior limb of the internal capsule and pyramidal tracts in the brainstem (black arrows). Abnormal signal intensity in the thalamus and medial lemniscus in the brainstem (white arrows). Trigeminal nerve trajectory involvement (white arrow head).
Transversal T2-weighted images of the medulla oblongata and spinal cord, and sagittal T2-weighted image of the cervical spine. Involvement of the pyramidal tract in the medulla oblongata and lateral corticospinal tracts of the spinal cord (black arrows). Involvement of dorsal columns of the spinal cord (white arrows).
The leucoencephalopathies comprehend a heterogeneous group of diseases that primarily affect the white matter of the brain. In 2003, van der Knaap et al. were the first to describe a novel entity, LBS-L (Leukoencephalopathy with Brainstem and Spinal cord involvement and increased Lactate), which exhibited a pattern of autosomal recessive inheritance.1
In most of the described cases, the symptoms start between early childhood and adolescence, and progress gradually. The main clinical features are slowly progressing cerebellar ataxia, tremors, muscle weakness and spasticity most prominent in the lower limbs, with mild or absent cognitive deficits.1–3 The disease progresses slowly, leading to walking disability and wheelchair dependency over the years. The phenotypic spectrum of the disease is very broad, ranging from oligosymptomatic cases, usually with onset in adulthood, to cases of early onset and rapid and fatal progression.4
Magnetic resonance imaging shows abnormal signal intensity at the level of the periventricular and deep white matter, selective involvement of cerebellar connections, and involvement of the entire length of the pyramidal and ascending tracts to the spinal cord and the intraparenchymal trajectories of the trigeminal nerve.5 The MRSI usually detects lactate elevation. These MRI abnormalities, along with the abnormal elevation of lactate in white matter found by MRSI, are considered characteristic of the disease.1–4The diagnosis is confirmed by genetic testing. LBS-L is an autosomal recessive disease caused by mutations in the DARS2 gene in chromosome 1, which encodes mitochondrial aspartyl-tRNA synthetase.6 We did not perform genetic testing in our patients, as the clinical manifestations, neuroimaging findings and elevated lactate in spectroscopy were so characteristic of the disease that we deemed them sufficient to make the diagnosis. However, genetic confirmation is important not only for advancing our knowledge of the disease, but also for its potential in prenatal diagnosis. The general prognosis is better than that of most hereditary leucoencephalopathies, with the exception of cases with childhood onset. At present, there is no effective treatment for the disease. Supportive measures are all that is available: early stimulation, physical therapy, rehabilitation, anticonvulsant therapy if required, and nutrition therapy.
In conclusion, we are presenting the cases of two female twins with an early diagnosis of leukoencephalopathy with brain stem and spinal cord involvement and elevated lactate, a rare metabolic disease that has been recently defined, who experienced rapid disease progression. We want to emphasise the usefulness of brain and spinal cord MRI, which revealed differential features consistent with LBS-L in both of the cases presented here, as they provide specific findings to guide the diagnosis of this disease.
Please cite this article as: Navarro Vázquez I, Maestre Martínez L, Lozano Setién E, Menor Serrano F. Leucoencefalopatía con afectación de troncoencéfalo y médula espinal y elevación de lactato: presentación de 2 nuevos casos. An Pediatr (Barc). 2016;84:291–293.