To quantitatively assess the learning capacity of school children aged between 8-12 years in basic life support (theory and practice) after a feasible school training programme.
Material and methodsQuasi-experimental study with a convenience sample of 567 pupils in 3rd and 5th year of Primary Education, and first year of Compulsory Secondary Education, from 3 public schools in Galicia. They received 2h (one theoretical and another practical) of basic life support training by their Physical Education teachers, as part of the school program. The children were evaluated by a theoretical test and a practical skill test that measured the quality of chest compressions, and assessed the performance of the basic life support sequence.
ResultsThe level of knowledge increased with respect to the baseline, and was higher in the higher grades (P < .001). The complete basic life support sequence was carried out by 16.5% of pupils in the 3rd year of Primary Education, 54.4% of pupils in the 5th year of Primary Education, and 28.5% of pupils in the 1st year of Secondary Education (P = .030). The following compression quality parameters improved significantly with age: continuity of compressions (P < .001), percentage of compressions performed at correct depth (P = .002), and median depth (P < .001), while the percentage of compressions with correct decompression decreased significantly (P < .001).
ConclusionsAlthough their anthropometric characteristics may not allow them to achieve the ideal quality of this manoeuvre, a 2h theoretical and practical training programme, taught by Physical Education teachers, helps to improve the ability of children younger than 13 years old to recognise the emergency, start the chain of survival, and initiate chest compressions.
Valorar cuantitativamente la capacidad de aprendizaje en soporte vital básico (teórica y práctica) de escolares de 8-12 años con un programa de formación adaptado a las escuelas.
Material y métodosEstudio cuasiexperimental con una muestra de conveniencia de 567 alumnos de 3° y 5° de Educación Primaria y 1° de Educación Secundaria Obligatoria, de 3 colegios concertados de Galicia, que recibieron 2 h (una teórica y otra práctica) de formación en soporte vital básico por parte de sus profesores de Educación Física integrada en el programa escolar. Los niños fueron evaluados mediante un test teórico y una prueba práctica que midió la calidad de las compresiones torácicas y valoró la secuencia de soporte vital básico.
ResultadosEl nivel de conocimientos aumentó respecto al basal y fue mayor en los alumnos de cursos superiores (p < 0,001). La secuencia completa de soporte vital básico fue realizada por el 16,5% de los escolares de 3° de Educación Primaria, el 54,4% de los de 5° de Educación Primaria y el 28,5% de los de 1° de Educación Secundaria Obligatoria (p = 0,030). Los siguientes parámetros de calidad de las compresiones mejoraron de forma significativa con la edad: continuidad de las compresiones (p < 0,001), porcentaje de compresiones realizadas con una profundidad correcta (p = 0,002) y mediana de profundidad (p < 0,001), mientras que el porcentaje de compresiones con descompresión correcta descendió significativamente (p < 0,001).
ConclusionesUn programa formativo teórico-práctico de 2 h, impartido por los profesores de Educación Física, contribuye a mejorar la capacidad de los niños menores de 13 años para reconocer la emergencia, poner en marcha la cadena de supervivencia e iniciar las compresiones torácicas, aunque posiblemente sus características antropométricas no les permitan alcanzar la calidad ideal establecida para esta maniobra.
Out-of-hospital cardiac arrest (OHCA) is witnessed by relatives, friends or other people in 70% of cases. In most instances, bystander cardiopulmonary resuscitation (CPR) attempts take place in the home, but CPR is only attempted before the arrival of medical emergency teams in less than 20% of cases,1 when early CPR is a key determinant of survival and neurologic outcome.2 The main strategy to increase the frequency of bystander CPR is training in basic life support (BLS), and in this regard, school-based training of students may be one of the most effective approaches.1,3
In Spain, there have been several official initiatives and projects to provide BLS training in the school setting,4–6 but there is no evidence yet on its actual impact on bystander initiation of BLS and victim survival. On the other hand, several studies in recent years have analysed the methodology of BLS training in children, with educational strategies varying significantly in terms of the duration of training, the methods used, the instructors and the minimum age for training.7
The Kids Save Lives initiative promoted by the European Resuscitation Council (ERC) with the support of the World Health Organization recommends 2 hours of school-based CPR training a year starting from age 12 years.3 However, it may not be necessary to wait until this age to start teaching first aid and BLS skills to children, as children as young as 6 years of age can learn the chain of survival8 and even how to use a semi-automatic defibrillator.9 In addition, while children under 12 years may not be able to deliver quality chest compressions (possibly on account of anthropometric factors),10 they are capable of delivering vigorous compressions and learn theoretical concepts.
The Adestrando Nenos e Xóvenes a Salvar Vidas project (Teaching children and youth to save lives, ANXOS) addresses the main practical uncertainties that have emerged in relation to school-based BLS training of children and youth. In this context, the aim of our study was to assess the acquisition of BLS theoretical knowledge and skills in students aged less than 13 years through a brief training delivered by their physical education instructors.
Material and methodsSampleWe conducted a quasiexperimental study in which we invited to participate a convenience sample of 658 students in 3 charter schools in Galicia. The study was approved by the Ethics Committee of the School of Education and Sport Sciences of the Universidad de Vigo.
The inclusion criteria were age 8 to 12 years, absence of physical or mental illness and written informed consent of parents and verbal assent of the minor. We excluded participants for who the anthropometric data were not documented or with incomplete data.
Study designThe ANXOS project started by setting up meetings to inform school administrators and parents, explaining the objectives and design of the study, and requesting the necessary authorizations and consent.
The next step was to train physical education instructors,11 who were to be responsible for training students. In a second phase (corresponding to the study presented here), students filled out an ad hoc questionnaire to assess their knowledge a week before undergoing a training structured in 2 sessions that took place in the times allotted to the 2 weekly physical education classes, each of which had a duration of 50 minutes. The first session was devoted to theoretical contents taught with materials adapted to the age of the students; the second session was devoted to practical training with adult-size manikins that provided instant visual feedback on the quality of chest compressions. There was 1 manikin per 5 students and 1 instructor per 25 students. Each student practiced delivering chest compressions on the manikin for a minimum of 6 minutes.
The practical session was organised around 3 stations: 1) the BLS sequence; 2) practice of BLS skills on an adult torso CPR training manikin (without feedback), and 3) practice of BLS skills on the manikin with real-time audio guidance and visual feedback.
After the training sessions, the theoretical knowledge and practical skills of the students were assessed again. Theoretical knowledge was assessed with the same questionnaire used for the baseline assessment at the beginning of the study. We evaluated practical skills through the simulation of a case of OHCA, assessing the ability to follow the steps of the BLS sequence and the quality of chest compressions delivered over 2 minutes.
VariablesWe collected data on the following variables: 1) sociodemographic and anthropometric characteristics (school year, age, weight, height, body mass index); 2) theoretical knowledge, assessed with a questionnaire; 3) BLS sequence: securing the scene, checking for a response, opening the airway, look-listen-feel assessment of breathing, alerting medical emergency services and initiation of chest compressions; 4) CPR quality: time to initiation of compressions (in seconds), chest compression fraction, percentage of compressions with hands in the right position, mean depth of compressions (in mm), percentage of compressions that reached the recommended depth (50-60 mm), percentage of compressions with correct decompression, mean rate of compressions (compressions/minute) and percentage of compressions delivered at the correct rate (100-120/minute).
Assessment toolsKnowledge questionnaireWe designed an ad hoc questionnaire to assess knowledge through 5 items with three answer choices of which only one was correct. The possible score ranged from 0 to 5 points (Appendix B, supplemental file 1).
Basic life support sequenceWe assessed the BLS sequence by means of an ad hoc evaluation form that included every step in the sequence and documented the time elapsed from the start of the simulation to initiation of chest compressions (Appendix B, supplemental file 2).
Quality of CPRTo measure the quality of the compression, we used the Laerdal Resusci Anne manikin with SkillReporter (version 12.0.0.2, wireless for PC), setting the parameters according to the 2015 ERC guidelines: chest compression depth of 50-60 mm; compression rate of 100-120 compressions/minute. As a quality criterion, we used a widely accepted arbitrary threshold of 70%.12
Statistical analysisIn the analysis of quantitative data, we assessed the normality of the distribution by means of the Kolgomorov-Smirnov test. We summarised quantitative variables using central tendency and dispersion measures (mean/median and standard deviation [SD]/interquartile range [IQR]) and qualitative variables as absolute and relative frequency distributions. We used the Pearson correlation coefficient to analyse the linear association between anthropometric variables and CPR quality variables. The association between categorical variables was assessed by means of the chi square test. We compared means with the Student t test or Mann-Whitney U test as applicable, and multiple means by analysis of variance (ANOVA) with the Bonferroni correction (homogeneity of variance met) or the Games-Howell correction (homogeneity of variance not met). The data were processed and analysed with the statistical software SPSS version 24.0. We defined statistical significance as a p-value less than 0.05.
ResultsThe initial sample consisted of 658 students, of who we excluded 42 (6.4%) due to incomplete data and 49 (7.4%) due to lack of signed informed consent at the start of the study, so the final sample included 567 students (48.0% female). The distribution by school year was: 32.1% in year 3 of primary education (PE), 31.6% in year 5 of PE, and 36.3% in year 1 of compulsory secondary education (known in Spain as ESO).
Theoretical knowledgeThe percentage of students that answered at least 4 questions (out of 5) increased from the pre- to the post-training test in every year: year 3 of PE (2.3% vs 25.6%; P < .001), year 5 of PE (1.1% vs 46.2%; P < .001) and year 1 of the ESO (23.3% vs 77.0%; P < .001).
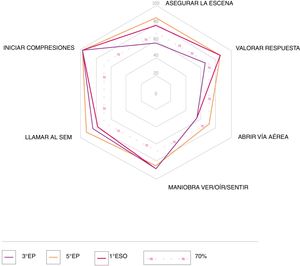
Basic life support sequenceFig. 1 and supplemental file 3 in Appendix B present the data concerning the performance of the BLS sequence after the training. At least 50% of the students were able to perform all the steps in the BLS sequence in each school year. The steps the students performed less frequently (< 70%) were “securing the scene” and “checking for a response” (students in year 3 of PE) and “opening the airway” (students in year 3 of EP and year 1 of ESO). More than 80% of students performed the “look-listen-feel assessment of breathing”, “alerting medical emergency services” and “initiation of chest compressions” steps.
When we analysed the percentage of students that performed the full sequence by school year, we found that a higher proportion of students in year 5 of PE could perform the full sequence compared to year 3 of PE or year 1 of ESO (year 3 of PE: 16.5%; year 5 of PE: 54.4%; year 1 of ESO: 28.5%; P = .030). In the subset of students that performed the full sequence, we did not find significant differences based on school year in the seconds elapsed from the start of the simulation to initiation of chest compressions (year 3 of PE: median, 52.2 [IQR, 43.3-58.7]; year 5 of PE: median, 47 [IQR, 42.5-55.3]; year 1 of ESO: median, 40.7 [IQR 40.3-56.4]; P = .577).
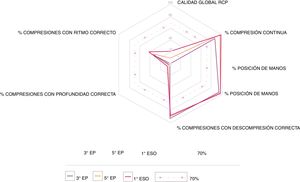
Quality of CPRFig. 2 presents the results on the parameters used to assess the overall quality of CPR by school year, with additional results presented in supplemental file 4 in Appendix B.
The chest compression fraction, mean depth of compressions and percentage of compressions with correct depth increased with the school year (P < .001). We also found significant linear associations between with CPR quality parameters and anthropometric variables (Table 1).
Linear relationship between cardiopulmonary resuscitation variables and anthropometric variables.
| Weight | Height | BMI | |
|---|---|---|---|
| r | r | r | |
| P | P | P | |
| Overall quality of resuscitation | 0.572 | 0.518 | 0.405 |
| < .001 | < .001 | < .001 | |
| Mean depth of compressions | 0.636 | 0.618 | 0.450 |
| < .001 | < .001 | < .001 | |
| Percentage of compressions with adequate recoil | −0.237 | −0.167 | −0.228 |
| < .001 | < .001 | < .001 | |
| Percentage of compressions with adequate depth | 0.470 | 0.398 | 0.334 |
| < .001 | < .001 | < .001 | |
| Percentage of compressions at adequate rate | 0.111 | 0.129 | – |
| 0.008 | 0.002 | – |
BMI, body mass index.
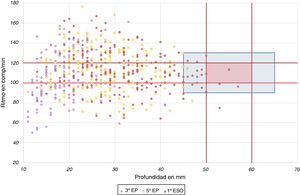
Fig. 3 presents the results regarding the depth of compressions (mm) and mean rate of compressions (per minute). It shows a target area, marked in red, that includes the recommended values,13 and a blue area defined by arbitrary deviation thresholds of ± 10 compressions per minute and ±5 mm of depth. When it came to depth, the target of 50 mm was only achieved by 3.4% of participants in year 1 of ESO (P = .002) compared to none in years 3 and 5 of PE. As for the compression rate, 31.9% of students in year 3 of PE, 33.0% in year 5 of PE and 45.1% in year 1 of ESO maintained an adequate rate of compressions (P = .003).
Only 2 students (0.98%) in year 1 of ESO delivered CPR at a depth of 50-60 mm and rate of 100-120 compressions/minute. However, 19 students of year 1 of ESO (9.27%), 4 (2.23%) in year 5 of PE (although none in year 3 of PE) managed to position themselves in the wider arbitrarily defined blue area.
DiscussionOur study shows that following a brief and simple training, delivered during school hours by the physical education instructors of the schools, enabled students in years 3 and 5 of PE and year 1 of ESO (ages 8-12 years) to activate the chain of survival and initiate basic life support, although the quality of CPR was insufficient.
Similar to previous studies, we found that students in the sample were able to assimilate knowledge on first aid and BLS.14–16 In fact, the results of a small study in Italy showed that students could even have greater capacity for knowledge acquisition and retention for this type of content compared to adults,17 which would further justify teaching BLS to schoolchildren without waiting for them to reach adolescence or adulthood.
When we assessed the performance of the BLS sequence, more than half of the children performed each of the steps, a proportion that exceeded 70% in the oldest group. Although most were not able to perform the full sequence with every step in the right order, it is fair to say that they exhibited good knowledge acquisition, as reported in previous studies.14,18 It must be taken into account that carrying out each step consecutively in adherence with current guidelines is no simple task even for adults.19
Another factor at play in the delivery of basic CPR was the physical characteristics of the students, in an age range that is strongly associated with anthropometric growth. Achieving the recommended depth of compression has proven a nearly impossible goal for children under 13 years.10,20 This is not the case of other compression quality parameters that are not as dependent on height and weight, such as the chest compression fraction, correct hand positioning or full chest recoil (which happens to be easier for weaker and younger children), for which we observed proportions greater than 85%, as did previous studies.10,14,18
The percentage of compressions followed by adequate decompression decreased with increasing student age. One of the possible explanations is that younger children allow adequate thoracic decompression to occur due to anthropometric factors, as it is more challenging for them to stop the recoil of the manikin’s chest. The association between the depth of compression, chest recoil and compression rate has already been demonstrated in the context of out-of-hospital CPR.21 When it comes to the compression rate, the factors at play are not only the anthropometric characteristics of rescuers or their ability to assimilate knowledge, but also the level of psychomotor development, which determines the ability to move at a given pace, in this case, at a rate of 100-120 compressions per minute. This explains why, despite the fact that the mean rate of compressions was in the recommended target range in every group, a higher proportion of older children achieved an adequate chest compression fraction. These differences between groups in favour of older students have already been observed in previous studies.10,14,22
The Kids Save Lives statement, issued by the ERC and endorsed by the World Health Organization, has the objective of increasing survival after OHCA and promotes 10 principles, the first of which is that “kids can save lives”.1 In consequence, the school is considered the ideal setting for training with the aim of having a significant impact on the response to OHCA. In several European countries, BLS training in schools is mandatory and integrated in the academic curriculum23; in Spain, Royal Decrees 126/201424 and 1105/2014,25 which establish the primary and secondary education curricula, respectively, include training on first aid, but do not specify the contents to be taught, so that teaching of BLS and CPR is not mandatory as it is in some neighbouring countries.
The inclusion of contents related to first aid in general or BLS in particular requires adequate knowledge of this material by schoolteachers. In a study conducted in Galicia, 70.6% of surveyed teachers reported having been trained on first aid, but the vast majority answered questions about BLS incorrectly.26 Recently, the ERC has issued a position statement on the subject,27 proposing that once they have been trained, teachers can be as competent as health care professionals in teaching BLS contents. In addition, training by schoolteachers would substantially cut costs compared to having to send health care professionals to each school. Therefore, inclusion of first aid-related subjects in the educational curricula of university courses for the training of early childhood educators and primary education teachers should be considered.26,28
There are limitations to our study. The conditions of the simulation hinder the extrapolation of results to potential real-world victims. On one hand, the psychological variables that affect a real-life situation cannot be introduced in this type of simulated scenarios, and on the other, simulations are conducted on manikins, which, while being a valid and reliable instrument, do not exactly reproduce the conditions of real-world CPR, in which compression parameters are also influenced by the physical characteristics of the victim.
We used only one training method, without a control group, and the assessment was conducted immediately after completion of the training, so that it does not reflect the retention of acquired knowledge and skills in the medium and long terms.
ConclusionA 2hour theoretical/practical workshop during school hours and taught by physical education instructors contributes to students learning how to identify an emergency, initiate the chain of survival and initiate basic CPR with chest compressions. The quality of compressions in terms of depth and rhythm proved insufficient. Training on BLS skills should be delivered in every school in Spain, as recommended by the World Health Organization and the ERC.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez-Isasi S, Abelairas-Gómez C, Pichel-López M, Barcala-Furelos R, Varela-Casal C, Vázquez-Santamariña D, et al. Aprendiendo a reanimar en la escuela. Estudio en escolares de 8-12 años. An Pediatr (Barc). 2022;96:17–24.