Insomnia is very common during childhood (30% of children under 5), and causes a serious cognitive and emotional consequence in learning, as well as significant medical comorbidity. It also affects the quality of life, not only of the child, but also of the whole family. Paediatrician training in its diagnosis and treatment is usually poor. For this reason a consensus document is presented on the management of insomnia in children and adolescents. This has been developed by members of the Spanish Paediatrics Association, the Spanish Sleep Society, the Spanish Society of Paediatric Outpatient and Primary Care, the Spanish Adolescent Medicine Society, the Spanish Child and Adolescent Society, and the Spanish Paediatric Neurology Society. This group suggests that diagnosis must be clinical and complementary tests will only be required in doubtful cases or when a differential diagnosis is needed. Likewise, treatment should be mainly based on cognitive-behavioural therapy and the modification of sleeping habits. Using medicines and other substances to make the sleep easier is currently quite common, even although there are no clinical guidelines to support this.
El insomnio es una patología muy frecuente en edad pediátrica (30% en niños menores de 5 años) que ocasiona una grave repercusión cognitiva y emocional en el aprendizaje junto con una importante comorbilidad médica y afectación de la calidad de vida del niño y la familia. La formación de los pediatras en el diagnóstico y el tratamiento del mismo suele ser deficitaria. Por todo ello, se presenta el documento de consenso sobre el manejo del insomnio en la infancia y la adolescencia elaborado por representantes de la Asociación Española de Pediatría, la Sociedad Española de Sueño, la Sociedad Española de Pediatría Extrahospitalaria y de Atención Primaria, la Sociedad Española de Medicina de la Adolescencia, la Sociedad Española de Psiquiatría Infantil y la Sociedad Española de Neurología Pediátrica. Este grupo recomienda que el diagnóstico debe ser clínico y solo en los casos dudosos o en que sea necesario un diagnóstico diferencial serán necesarias pruebas complementarias. Asimismo el tratamiento se debe basar principalmente en terapias cognitivo-conductuales y en una modificación de los hábitos de sueño. El uso de medicamentos y sustancias para facilitar el sueño es elevado, aunque no existen guías clínicas que lo apoyen.
Sleep is a developmental and active process that starts before birth as a result of a shifting and dynamic interaction of biological, psychological and social factors; its evolution depends on the balance between these three domains.1
Insomnia affects 30% of children aged 6 months to 5 years. In Spain, 27% of children aged 5 to 7 years resist going to sleep, 11% exhibit a prolonged sleep onset latency, 6% experience frequent awakenings, and 17% have difficulty waking up in the morning.2 As for adolescents, 38.5% report a perceived poor quality of sleep, and 23.1% a sleep onset latency of more than 30min.3 Sleep problems have an impact on children and their environment and lead to an increase in health care utilisation, with children with problems making a mean of 8.84 sick visits a year compared to 6.34 in children without.4
Health care professionals have insufficient training on sleep. Various scientific associations present this consensus as a contribution towards its improvement.
Consensus methodologyMethod modified nominal group technique in which in-person meetings were replaced using online means.
Systematic reviews of primary, secondary and tertiary sources (backward search starting from references in the literature). The search period ended in May 2015.
Language limits: English and Spanish.
The participating scientific associations appointed the members of the consensus group, who signed a statement regarding their conflicts of interest.
The group was divided in subgroups: Aetiology-definition; Clinical Manifestations-Diagnosis; and Treatment. Each subgroup elaborated their conclusions, which were later distributed to the entire group for discussion and approval. A writing team (G. Pin, V. Soto) produced the final manuscript, which was revised and approved by the rest of the group. The work was conducted online. Neither the consensus project nor the authors have received any funding.
Object of the consensus: chronic insomnia in children with normal development. The authors consider that most cases of insomnia can be managed in primary care (PC).
Concept and classification- a.
Concepts:
- 1.
The mother-infant dyad is a “complex adaptive system”: a dynamic network of systems that acting in a parallel yet interconnected and mutually complementary; one cannot be understood without reference to the other.5 Maternal stress during the third trimester of gestation facilitates placental permeability to corticosteroids, which influences:
- –
An increase in foetal corticosteroid levels.
- –
A delayed development of diurnal cortisol rhythms.
- –
Hyperarousal with activation of the hypothalamic-pituitary-adrenal axis in stressful situations.6
- –
- 2.
Sleeping through the night: It requires three elements7:
- i.
A period of uninterrupted sleep.
- ii.
Sleep schedule that coincides with that of the rest of the family.
- iii.
Ability to go back to sleep independently following nighttime awakenings.
- i.
- 3.
Paediatric insomnia: the second edition of the International Classification of Sleep Disorders (ICSD-2) of the American Academy of Sleep Medicine defined it as a “repeated difficulty with sleep initiation, duration, consolidation, or quality that occurs despite age appropriate time and opportunity for sleep, which results in some form of daytime functional impairment for the child and/or family.”
A sleep onset latency of more than 30min and/or wake times lasting longer than 20min can lead to clinically significant distress or impairment in social, familial, academic or other important areas of functioning.
- 1.
- b.
Classification: the Diagnostic and Statistical Manual (DSM-5) of the American Psychiatric Association includes insomnia as a single category; however, the International Classification of Sleep Disorders, Third Edition (ICSD-3) includes8:
- 1.
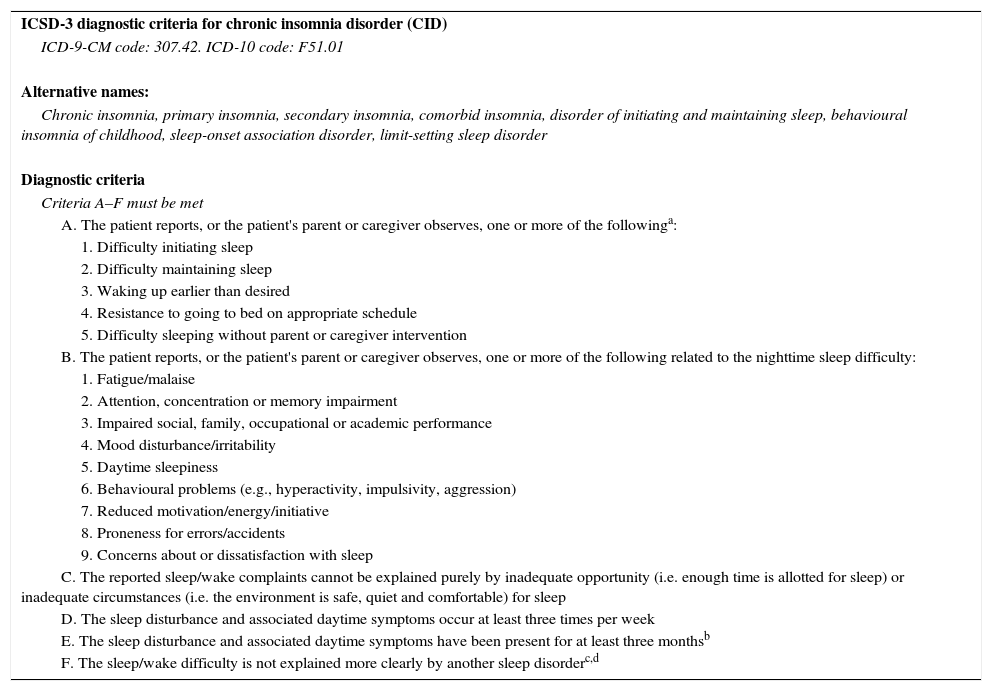
Chronic insomnia disorder (CID) (Table 1).
Table 1.Diagnostic criteria for chronic insomnia disorder.
ICSD-3 diagnostic criteria for chronic insomnia disorder (CID) ICD-9-CM code: 307.42. ICD-10 code: F51.01 Alternative names: Chronic insomnia, primary insomnia, secondary insomnia, comorbid insomnia, disorder of initiating and maintaining sleep, behavioural insomnia of childhood, sleep-onset association disorder, limit-setting sleep disorder Diagnostic criteria Criteria A–F must be met A. The patient reports, or the patient's parent or caregiver observes, one or more of the followinga: 1. Difficulty initiating sleep 2. Difficulty maintaining sleep 3. Waking up earlier than desired 4. Resistance to going to bed on appropriate schedule 5. Difficulty sleeping without parent or caregiver intervention B. The patient reports, or the patient's parent or caregiver observes, one or more of the following related to the nighttime sleep difficulty: 1. Fatigue/malaise 2. Attention, concentration or memory impairment 3. Impaired social, family, occupational or academic performance 4. Mood disturbance/irritability 5. Daytime sleepiness 6. Behavioural problems (e.g., hyperactivity, impulsivity, aggression) 7. Reduced motivation/energy/initiative 8. Proneness for errors/accidents 9. Concerns about or dissatisfaction with sleep C. The reported sleep/wake complaints cannot be explained purely by inadequate opportunity (i.e. enough time is allotted for sleep) or inadequate circumstances (i.e. the environment is safe, quiet and comfortable) for sleep D. The sleep disturbance and associated daytime symptoms occur at least three times per week E. The sleep disturbance and associated daytime symptoms have been present for at least three monthsb F. The sleep/wake difficulty is not explained more clearly by another sleep disorderc,d Notes:
aDifficulties initiating or maintaining sleep or waking up early can occur in all age groups. Resistance to going to bed at an appropriate time and difficulty falling asleep without the intervention of a parent or caregiver is most common in children and elderly individuals that require monitoring by a caregiver due to significant functional impairment (e.g., seniors suffering from dementia).
bSome patients with chronic insomnia may experience recurrent episodes of sleep/wake problems lasting several weeks and for many years, yet not meet the criterion of three months’ duration for each isolated episode. Nevertheless, these patients should be given a diagnosis of CID, given the intermittent difficulties in sleep that persist through time.
cSome patients that use hypnotics regularly may sleep well and not meet the criteria of insomnia disorder while they are taking them. However, in the absence of these medications these same patients may meet the diagnostic criteria. This diagnosis applies to these patients if they experience significant concern about their inability to sleep without pharmacological treatment.
dSeveral comorbidities, such as chronic pain disorders or gastroesophageal reflux disorder (GERD) may cause the sleep/wake complaints presented here. When these comorbidities are the only cause of the sleep disturbance, a separate diagnosis of insomnia is not warranted. However, in many patients these are chronic conditions and are not the only source of sleep problems. Their clinical manifestations must be assessed. If there is evidence that the symptoms are not caused by the medical problem alone and they require independent treatment, the diagnosis of CID should be made.
- 2.
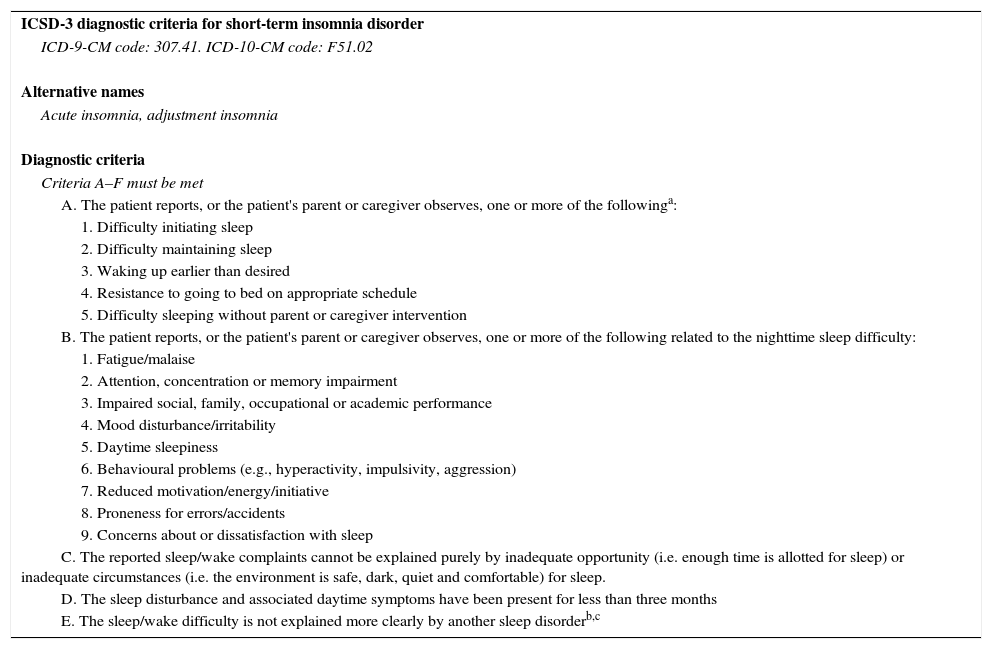
Short-term insomnia disorder (Table 2).
Table 2.ICSD-3 diagnostic criteria for short-term insomnia disorder.
ICSD-3 diagnostic criteria for short-term insomnia disorder ICD-9-CM code: 307.41. ICD-10-CM code: F51.02 Alternative names Acute insomnia, adjustment insomnia Diagnostic criteria Criteria A–F must be met A. The patient reports, or the patient's parent or caregiver observes, one or more of the followinga: 1. Difficulty initiating sleep 2. Difficulty maintaining sleep 3. Waking up earlier than desired 4. Resistance to going to bed on appropriate schedule 5. Difficulty sleeping without parent or caregiver intervention B. The patient reports, or the patient's parent or caregiver observes, one or more of the following related to the nighttime sleep difficulty: 1. Fatigue/malaise 2. Attention, concentration or memory impairment 3. Impaired social, family, occupational or academic performance 4. Mood disturbance/irritability 5. Daytime sleepiness 6. Behavioural problems (e.g., hyperactivity, impulsivity, aggression) 7. Reduced motivation/energy/initiative 8. Proneness for errors/accidents 9. Concerns about or dissatisfaction with sleep C. The reported sleep/wake complaints cannot be explained purely by inadequate opportunity (i.e. enough time is allotted for sleep) or inadequate circumstances (i.e. the environment is safe, dark, quiet and comfortable) for sleep. D. The sleep disturbance and associated daytime symptoms have been present for less than three months E. The sleep/wake difficulty is not explained more clearly by another sleep disorderb,c Notes:
aDifficulties initiating or maintaining sleep or waking up early can occur in all age groups. Resistance to going to bed at an appropriate time and difficulty falling asleep without the intervention of a parent or caregiver is most common in children and elderly individuals that require monitoring by a caregiver due to significant functional impairment (e.g., seniors suffering from dementia).
bPatients with short-term insomnia disorder may complaint of sleep/wake difficulties occurring less than three times a week on average, yet may experience clinically significant anxiety regarding their symptoms warranting clinical attention.
cMany processes such as grieving, acute pain or other stressors are often associated with sleep deprivation. When these conditions are the sole cause of difficulty sleeping, a separate diagnosis of insomnia does not apply. The main factor in the diagnosis of short-term or adjustment insomnia is the degree to which the sleep disturbance impacts the individual and/or warrants independent clinical attention.
- 3.
Other insomnia disorders. Rare cases that do not meet the criteria for short-term insomnia disorder with symptoms significant enough to require medical attention.
- 1.
- c.
Conditioning factors: various factors play a role in insomnia:
- 1.
Circadian factor: melatonin and light. Initiation of melatonin secretion at night under dim light conditions (dim-light-melatonin-onset [DLMO]) precedes sleep onset by approximately 2h.
Children that are forced to go to sleep at a time that is too close to or too far from their DLMO exhibit longer sleep onset latencies and greater resistance to go to bed.9
- 2.
Homeostatic factor: late naps. The more hours of wakefulness that precede bedtime, the easier it is to fall asleep.
- 3.
Environmental factor: light, noise and temperature. Exposure to light during the night, combined with reduced exposure in the morning, favours insomnia. The percentage decrease in melatonin secretion in the presence of light before bedtime reaches 88% in children.10
- 4.
Educational factor: healthy lifestyle habits. Evidence on bedtime routines has shown a dose-dependent direct association between sleep habits and perceived sleep problems.11
- 5.
Neuroendocrine factor: cortisol.
Sleep deprivation is associated with elevated cortisol levels in the evening.12
- 1.
Dissatisfaction with sleep quantity or quality, expressed in terms of bedtime resistance, frequent awakenings and/or difficulty falling asleep without help.
The clinical impact results from sleep deprivation and includes nocturnal as well as diurnal disturbances:
- a.
Nocturnal: sleep onset latency of more than 20 to 30min, wake time after sleep onset of more than 60min, or nighttime awakenings (requiring caregiver intervention).
- b.
Diurnal: somnolence, attention and memory impairments, mood changes, behavioural problems and poor academic performance.13 It can impact cardiovascular, immune and metabolic systems, including obesity and growth disorders.14 It affects the quality of life of the family.
In many instances, insomnia results from inappropriate associations or inadequate limit-setting8:
- –
Insomnia due to inappropriate sleep onset associations. Results from a dependency on stimulation with specific objects or specific changes to initiate sleep or to fall back asleep after awakening. Falling asleep is associated with some form of stimulation (rocking chair, TV watching), object (bottle) or environment (lit room, parental presence in the room, or falling asleep in the parental bed). Absence of the stimulus leads to difficulties and restoration of the stimulus facilitates sleep.
- –
Clinical manifestations: frequent nighttime awakenings, nighttime fears or anxiety about sleeping alone. It is considered a disorder if: (1) the associations are problematic and very demanding; (2) sleep onset is significantly delayed or sleep is interrupted in the absence of the associated conditions, and (3) frequently requires the intervention of parents or caregivers.
- –
Limit-setting insomnia. Refusal to go to bed reinforced by inappropriate or inconsistent limit setting. It can lead to nighttime awakenings depending on the response of parents or caregivers during the night.
- –
Insomnia due to poor sleep hygiene. The child or the parents/caregivers engage in behaviours incompatible with quality sleep and normal wakefulness during the day, such as late daytime naps, irregular schedules, use of stimulant substances, arousing or disturbing mental, emotional or physical activities close to bedtime, inadequate sleep environment (noise, light stimulation, TV, computer, etc.).15
- –
Psychophysiological insomnia. Older children and adolescents may have sleep disturbances resulting from hyperarousal and/or associations with past experiences.
Clinical manifestations: excessive preoccupation with sleep, fear of sleeping or of being unable to fall asleep, fear of elements close to the bedroom, memories of past negative experiences… These individuals sleep better outside their normal environment.
DiagnosisThe diagnosis is essentially clinical, based on the information provided by the parents/caregivers and the child.14
- 1.
History-taking. Must explore potential organic causes and psychomotor development, with observation of the behaviour of the child and the family. Include assessment of16,17:
- –
Onset of sleep disorder, attempted solutions and their outcomes.
- –
24hour sleep pattern. Timing and amounts of sleep, place of sleep, number of awakenings, and interventions.
- –
Environmental component: light exposure during day and night, television, electronic device screens, physical activity, noise, temperature.
- –
Educational component. Presence or absence of bedtime routines, schedules, type of parental responses.
- –
Impact of the sleep disorder on the child and on the family structure.
- –
Family history and context: maternal stress in the last trimester of pregnancy. Type of delivery and infant feeding. Organisation of family structure. Attachment style. Family sleep patterns. Parental expectations. Cultural factors.
- –
- 2.
Full clinical evaluation. Indispensable.
- 3.
Sleep log/diary. Graphic representation of the sleep-wake cycle over 15 days. Keeping a log of unscheduled sleep is recommended for the purpose of calculating the DLMO.18,19
- 4.
Scales and questionnaires. Various questionnaires can be used for a general assessment of sleep. None of them are validated in Spanish or for use in Spanish children and adolescents.14
- –
Brief Infant Sleep Questionnaire (BISQ).
- –
BEARS.
- –
Sleep Disturbance Scale for Children (SDSC).
- –
- 5.
Polysomnography and actigraphy. Diagnostic tests should be selected based on clinical findings with the purpose of confirming the clinical impression. They should never replace the anamnesis. Polysomnography is indicated when there is a strong clinical suspicion of sleep-related breathing disorder (SRBD), atypical parasomnia, periodic limb movement disorder, clinically unconfirmed restless leg syndrome (RLS) or nocturnal seizures if the findings of the clinical history and conventional encephalography are inconclusive.20,21Actigraphy monitors body motion and assesses sleep and wake patterns in the natural environment of the patient. It can measure the total sleep time, sleep efficiency, wake after sleep onset, and sleep onset latency. It is recommended for determining sleep patterns and documenting response to treatment in children and special paediatric populations.22
Insomnia is frequently secondary to the manifestations of other pathologies and/or circumstances23:
- 1.
Normal variations in sleep. changes in sleep duration and pattern occur throughout the lifespan, with great interindividual variability.24
- 2.
Medical disorders:
- –
Pain, pruritus.25
- –
Respiratory disorders.26
- –
Gastrointestinal disorders. Gastroesophageal reflux, constipation, chronic abdominal pain or inflammatory intestinal disease.27
- –
Neurodevelopmental disorders. ADHD (25–50%), cognitive disorders (10–86%), autism spectrum disorders (48–56%), cerebral palsy (45%). Insomnia is one of the diagnostic criteria for certain diseases (Rett syndrome, Williams syndrome or Smith-Magenis syndrome).28,29
- –
Epilepsy. Frontal lobe epilepsy, requires differential diagnosis including nighttime awakenings or parasomnias.
- –
Iron deficiency. Ferritin levels of less than 35 to 50ng/mL, even in the absence of anaemia, have been associated with insomnia.30
- –
Other medical conditions. Baby colic, moderate-severe traumatic brain injury (even months after the injury).31
- –
Primary sleep disorders. RLS, enuresis, SRBDs, circadian rhythm disorders (delayed sleep phase syndrome in adolescents). Homemade video recordings can be helpful.
- –
- 3.
Psychiatric disorders (anxiety, depression).32 There is a complex and bidirectional relationship between psychiatric disorders and sleep.
- –
Anxiety disorders: stressful situations, intrusive thoughts or post-traumatic stress disorder.
- –
Depression: mood disorders are associated with a subjective perception of insomnia and, at the same time, insomnia exacerbates depressive symptoms—it doubles the risk of suffering from depression.
- –
- 4.
Pharmaceuticals and abused substances:
- –
Caffeine, alcohol and nicotine.33
- –
Beta-adrenergic drugs (salbutamol), stimulants (methylphenidate, lisdexamfetamine [take into account the potential rebound effect after discontinuation of treatment]), corticosteroids, anticonvulsants (lamotrigine) or antidepressants (SSRIs).
- –
- 5.
Environmental factors: noise, excessive light (electronic devices) and inappropriate temperature. Inadequate sleep habits.
Although pharmacological treatment has been used extensively, behavioural therapy (teaching the patient strategies to promote good habits) is more widely accepted and has longer-lasting effects.34
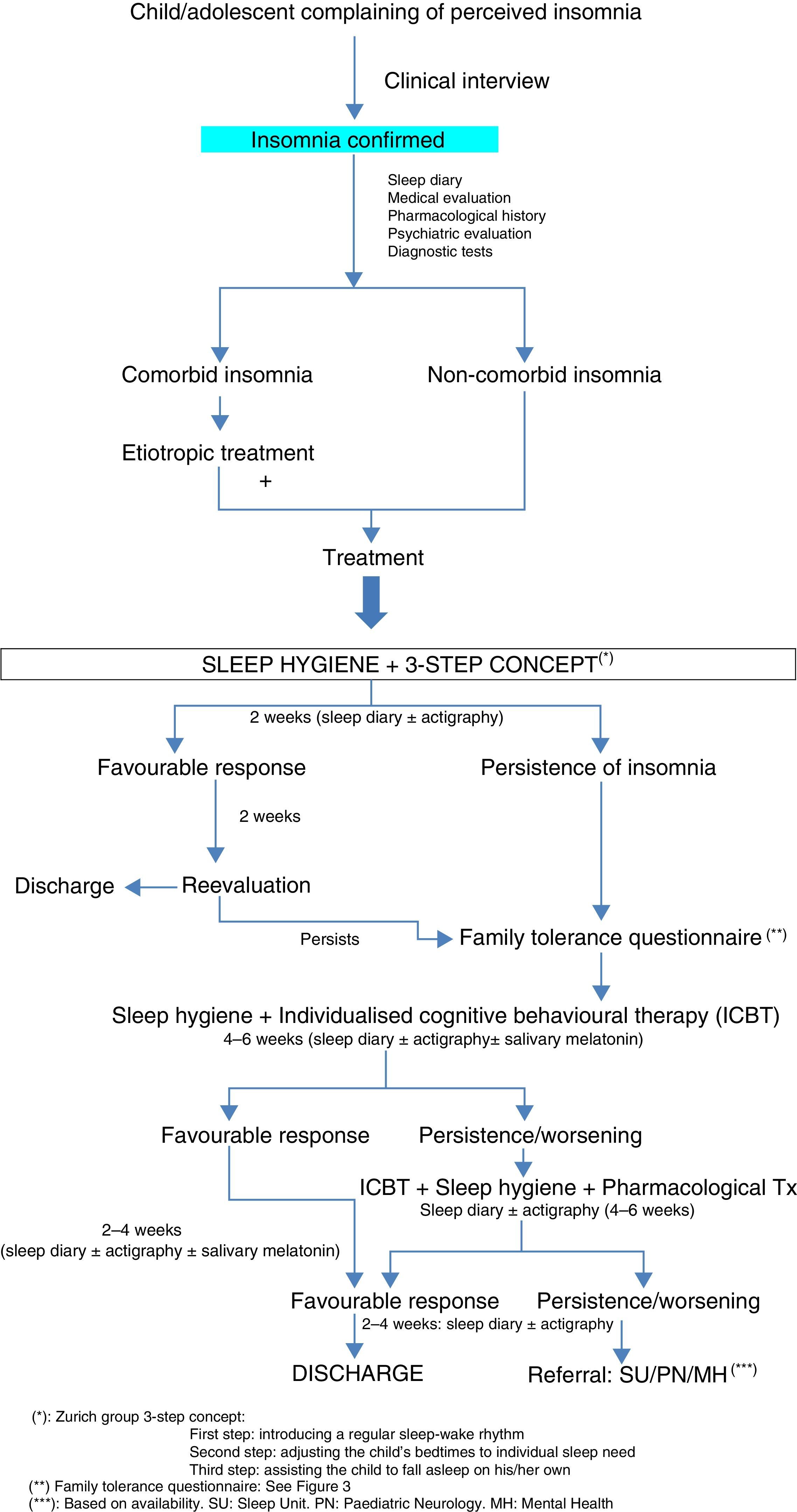
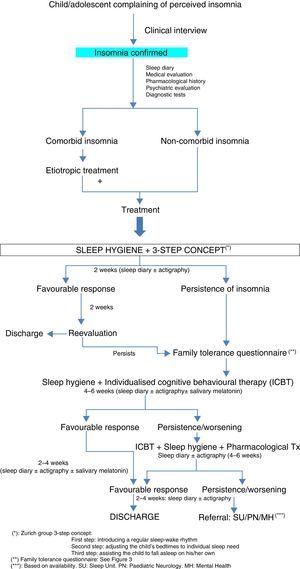
The consensus group proposes a progressive approach to insomnia disorders, as shown in the flowchart (Fig. 1).
- (A)
Behavioural therapy: various strategies, such as sleep hygiene, environmental and dietary measures, and psychological treatment.35 A combination of several or all strategies increases effectiveness.
- (B)
A, 1. Sleep hygiene: establishment bedtime routines, with regular times for going to bed and getting up (Table 4). Sending the child to sleep, to bed, or to the child's room should not be used as a punishment.
- (C)
A, 2. Environmental and dietary measures
- 1.
Promote physical activity, avoiding it close to bedtime.
- 2.
Avoid screens within one hour from bedtime.
- 3.
Temperature of 19 to 22°C.
- 4.
Quiet.
- 5.
Avoid eating within half hour from bedtime, and do not consume caffeinated or energy drinks after midday. Carbohydrates and foods rich in tryptophan promote sleep.36
A, 3. Psychological treatment: intervention at the family level. It should start with a psychoeducational intervention, explaining the theoretical underpinnings of behavioural modification, and resolving questions and concerns.
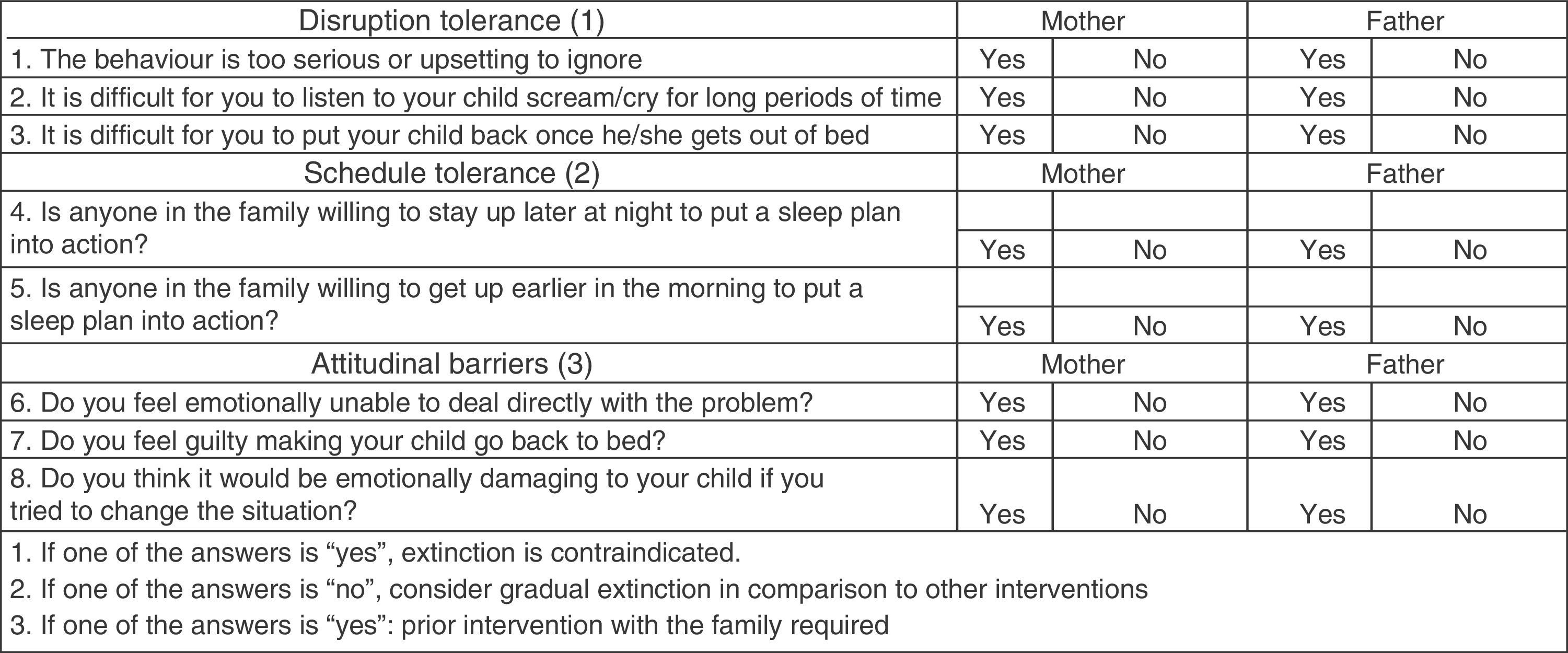
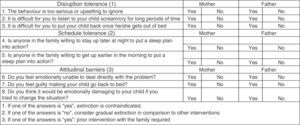
The treatment plan will be individualised based on the behaviours and expectations of the family (Fig. 2). Different strategies whose efficacy is supported by high-grade scientific evidence should be contemplated. Chief among them are those aiming to reduce arousal and cognitive-behavioural interventions.37 Relaxation has proven to be very effective, and includes teaching breathing, progressive muscle relaxation or meditation techniques.
Figure 2.Family tolerance questionnaire. Source: del Rosso and Hoque.25
The available scientific evidence shows that cognitive-behavioural treatment is the most effective and widely used approach in the management of insomnia.38 The main strategies are:
- 1.
Extinction. Ignoring the child's demands from bedtime to waking time. This shortens sleep onset latency and reduces the number of wakings. If the child goes to the parents’ bed, parents must return the child to bed without additional interaction. At first, there may be a transient increase in the problematic behaviour (an “extinction burst”) as the child intensifies intrusions in an attempt to elicit past responses. If parents persist in ignoring the child's demands, the problematic behaviour will gradually fade. The psychological process at play is the elimination of reinforcements.
- 2.
Graduated extinction. Parents progressively ignore the child, increasing the time intervals between interactions.
- 3.
Positive reinforcement. Positive reinforcers help initiate sleep or prolong its duration.
- 4.
Response cost. Suppression of the positive stimulus that acts as a reinforcer for insomnia. This is achieved by delaying bedtime when the positive reinforcer of insomnia is the positive interaction with the parents at bedtime.
- 5.
Delayed bedtime. Bedtime is temporarily delayed to match the actual timing of sleep initiation.
- 6.
Scheduled awakenings. Pre-emptive awakenings are scheduled prior to the spontaneous awakenings of the child. The parents then provide positive reinforcers such as feeding or tucking in the child, preventing the unpleasant stimuli associated with spontaneous awakenings.
- 7.
“Bedtime pass programme”. Effective in children aged more than 3 years that resist going to bed. The child is given a series of notecards that can be exchanged for behaviours such as getting a story, drinking water, etc., with the agreement that once the child runs out of cards, the child must go to sleep.
- 1.
- (D)
Pharmacological treatment: it should not be the first or the only treatment modality, and must be integrated in a broader treatment plan.
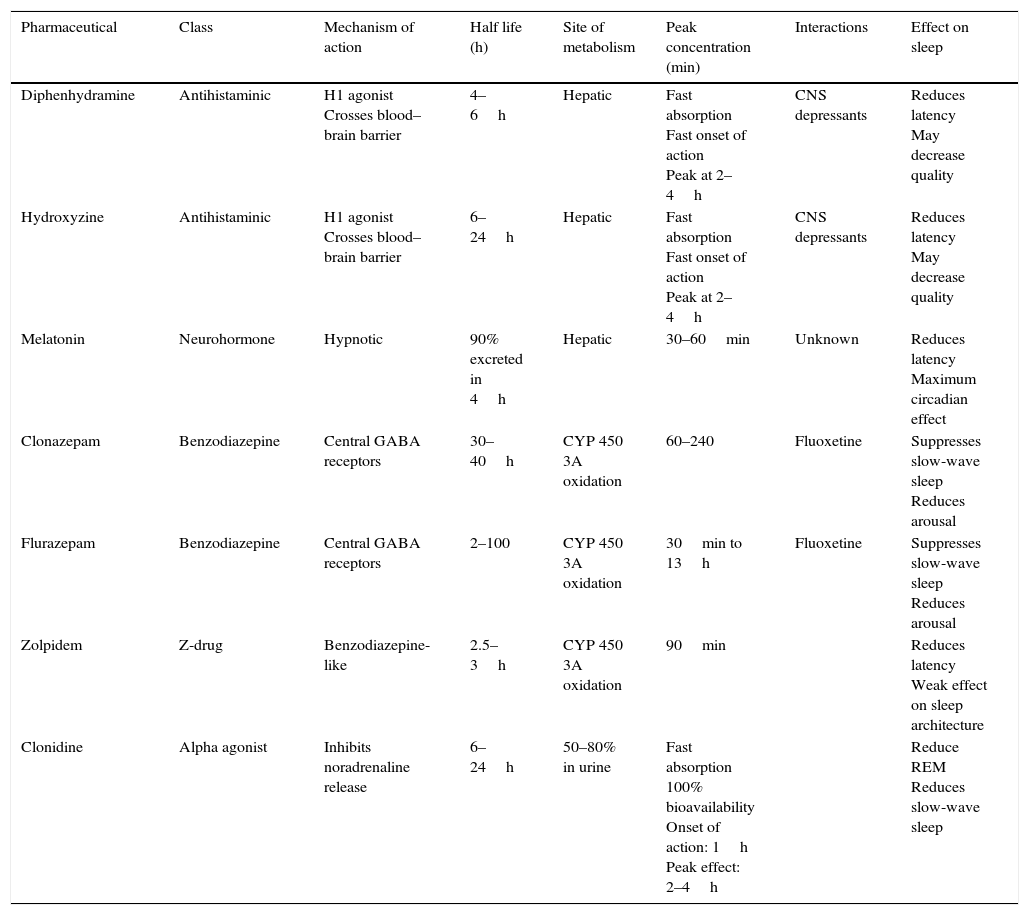
Table 3 summarises the most frequently used drugs. They are all used off-label, and there is little scientific evidence on their efficacy and safety in the intermediate and long term.
Table 3.Drugs used to treat insomnia.
Pharmaceutical Class Mechanism of action Half life (h) Site of metabolism Peak concentration (min) Interactions Effect on sleep Diphenhydramine Antihistaminic H1 agonist
Crosses blood–brain barrier4–6h Hepatic Fast absorption
Fast onset of action
Peak at 2–4hCNS depressants Reduces latency
May decrease qualityHydroxyzine Antihistaminic H1 agonist
Crosses blood–brain barrier6–24h Hepatic Fast absorption
Fast onset of action
Peak at 2–4hCNS depressants Reduces latency
May decrease qualityMelatonin Neurohormone Hypnotic 90% excreted in 4h Hepatic 30–60min Unknown Reduces latency
Maximum circadian effectClonazepam Benzodiazepine Central GABA receptors 30–40h CYP 450 3A oxidation 60–240 Fluoxetine Suppresses slow-wave sleep
Reduces arousalFlurazepam Benzodiazepine Central GABA receptors 2–100 CYP 450 3A oxidation 30min to 13h Fluoxetine Suppresses slow-wave sleep
Reduces arousalZolpidem Z-drug Benzodiazepine-like 2.5–3h CYP 450 3A oxidation 90min Reduces latency
Weak effect on sleep architectureClonidine Alpha agonist Inhibits noradrenaline release 6–24h 50–80% in urine Fast absorption
100% bioavailability
Onset of action: 1h
Peak effect: 2–4hReduce REM
Reduces slow-wave sleepTable 4.Phytotherapy.
Name Mechanism of action Dosage Effect on sleep Comments Valerian Binds benzodiazepine receptors 2–3g×3/day Shortens sleep latency
Increases deep sleep (?)Rare toxicity Chamomile Binds benzodiazepine receptors 1–3g×3/day Shortens sleep latency (?) Hypertensive effect Kava CNS depression 60–120mg/day Improves sleep efficiency Weak anxiolytic
Liver toxicityLavender CNS depression Inhaling essential oil Improves sleep efficiency Potentiates effects of alcohol Certain overall guidelines apply39:
- 1.
Pharmacological treatment must be as short as possible (<4 weeks) and administered at the minimum effective dose.
- 2.
The drug should be selected based on the characteristics of the insomnia, the patient and the environment. Paediatricians should become acquainted with the pharmacological profile of hypnotics.
- 3.
The timing of administration is important. Treatment is less effective if administered at the circadian peak in alertness that typically occurs in late afternoon.
- 4.
Close monitoring of side effects, especially during withdrawal.
- 5.
It may exacerbate comorbid sleep disorders (SRBD).
- 6.
Beware of potential interactions with other drugs. Especial care should be taken in adolescents (possibility of pregnancy and substance use).
- 7.
Evaluate the use of over-the-counter medication by the family.
- 1.
The consensus group considers that, in addition to iron supplementation, two other drug groups are indicated for management at the PC level. If they are not effective, the patient should be referred to a specialised unit:
- (A)
First-line drug: melatonin.35
Advantages: reduces sleep onset latency.
Disadvantages: few studies support its safety in the intermediate and long term when it is used for prolonged periods of time.
Dosage: the initial dose should be 1 to 3mg in infancy and early childhood, and 2.5 to 5mg in older children, gradually adjusting the dose based on patient response. Adolescents: 1 to 5mg.
It should always be administered at the same time, between 30 and 60min before the usual bedtime.
There are no data on the use of extended-release melatonin in children with normal development.
Duration: it should not exceed four weeks of continued treatment.
In sleep-onset insomnia treated with melatonin alone, treatment discontinuation leads to recurrence of the original problem in 90% of cases.
- (B)
Second-line drugs (after 4 weeks of treatment with melatonin with unsatisfactory results).
First-generation antihistamines (diphenhydramine, hydroxyzine).40
Diphenhydramine: rapidly absorbed, does not produce gastric irritation.
Advantages: paediatricians are familiar with its use.
Especially useful in acute situations.
Disadvantages: some studies support its efficacy, while others failed to find a difference between treatment and placebo.
There is a risk of paradoxical reaction.
Dosage: 1mg/kg.
Hydroxyzine: dosage: 12 months to 6 years, 1 to 2.5mg/kg at night. Age more than 6 years, 1 to 2mg/kg at night.
Duration: 4 weeks.
The rest of the drugs listed in Table 3 should be used following a thorough evaluation by a specialised unit.
- (C)
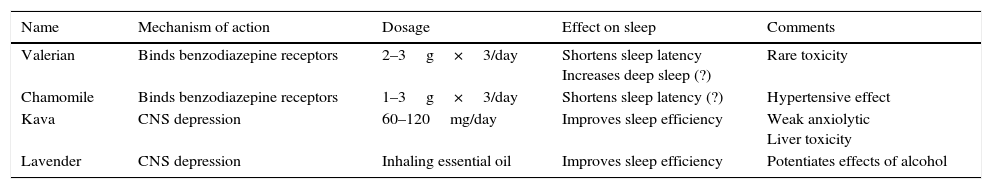
Phytotherapy. Table 4 summarises the main properties of the most frequently used treatments.
Its use is based on tradition, with scarce data from evidence-based medicine.
Few studies have found evidence of the usefulness of specific herbal treatments in the paediatric population, and these remedies have generally not been tested. Parents must be made aware of the lack of studies demonstrating the efficacy and safety of these substances in children and adolescents, as well as the lack of knowledge regarding their dosage, susceptibility and potential contaminants.
This consensus group recommends a holistic approach to chronic insomnia in children and adolescents, with evaluation of predisposing and aetiological factors.
Treatment should always be individualised and start with sleep hygiene and cognitive-behavioural measures. Pharmacological treatment should be as short as possible and be administered at the minimum effective dose.
Conflicts of interestThe authors have no conflict of interests to declare.
Please cite this article as: Pin Arboledas G, Soto Insuga V, Jurado Luque MJ, Fernandez Gomariz C, Hidalgo Vicario I, Lluch Rosello A, et al. Insomnio en niños y adolescentes. Documento de consenso. An Pediatr (Barc). 2017;86:165.