The ingestion of a caustic agent is the most common cause of admission after being in contact with a domestic product. A group of patients could be considered low risk and not require aggressive procedures such a corticosteroid administration and endoscopy, especially in the paediatric population.
ObjectiveTo evaluate the safety and benefit of a less aggressive protocol for patients defined as low risk.
Material and methodsAn analytical–observational study conducted on patients who consulted for caustic ingestion between January 2011 and December 2015. Two periods were differentiated according to the current protocol. Period-1: usual protocol (which included admission and parenteral corticosteroid and antibiotic administration) and Period-2: less aggressive protocol for the low risk patients (oral intake test after 6h and discharged if they remained asymptomatic). Low risk patients were considered as those who met the following criteria: unintentional intake, absence of symptoms and oral lesions. In the rest of the patients the usual protocol was performed. Re-admission with a diagnosis of digestive lesions was considered as a complication.
ResultsForty-eight patients were included in period 1, and 35 in period 2. In period 2, thirteen patients met low risk criteria. The adherence to the less aggressive protocol was 100%. None of the low risk patients required admission or endoscopy after discharge. In period 1 the adherence to the usual protocol was 60.4%. Six patients would have benefited from the application of the less aggressive protocol.
ConclusionsAdopting a more conservative attitude in low risk patients is safe. These patients benefit from clinical observation, without performing more aggressive measures with their possible iatrogenic adverse effects.
La ingesta de cáusticos es la causa más frecuente de consulta tras el contacto con un producto doméstico. Un grupo de pacientes podría considerarse de bajo riesgo y no recibir corticoides parenterales ni realizársele endoscopia, procedimiento considerado terapéuticamente agresivo, sobre todo en la edad pediátrica.
ObjetivoEvaluar la seguridad y el beneficio de un protocolo menos agresivo en los pacientes definidos de bajo riesgo.
Material y métodosEstudio analítico-observacional de los pacientes que consultaron por ingesta de cáustico entre enero de 2011 y diciembre de 2015. Se diferenciaron 2 periodos según el protocolo vigente. Periodo-1: protocolo habitual (incluido ingreso y administración de corticoide-antibiótico parenteral) y periodo-2: protocolo menos agresivo en los pacientes de bajo riesgo (prueba de tolerancia oral tras 6h y alta hospitalaria si persistían asintomáticos). Se consideraron de bajo riesgo si se cumplían todos los criterios: ingesta involuntaria, ausencia de síntomas y lesiones orales. En el resto de pacientes se mantuvo el protocolo habitual. Se consideró como complicación el reingreso con diagnóstico de lesiones digestivas.
ResultadosSe incluyeron 48 pacientes en el periodo 1 y 35 en el periodo 2. En el periodo 2 cumplían criterios de bajo riesgo 13 pacientes. La adherencia al protocolo menos agresivo fue del 100%. Ningún paciente de bajo riesgo precisó ingreso tras el alta ni realización de endoscopia. En el periodo 1 la adherencia al protocolo habitual fue del 60,4%. Seis pacientes se habrían beneficiado de la aplicación del protocolo menos agresivo.
ConclusionesAdoptar una actitud más conservadora en los pacientes de bajo riesgo es seguro. Estos pacientes se benefician de la realización de una observación clínica, obviando medidas más agresivas con posibles efectos iatrogénicos secundarios.
The ingestion of caustic substances is the most frequent reason for visiting the paediatric emergency department (PED)after contact with a household cleaning product. In addition, caustic substances are the group of toxic substances most likely to cause sequelae.1
Traditionally, guidelines for the management of caustic ingestion have included parenteral administration of corticosteroids and antibiotics. The purpose of steroid therapy was to reduce the risk of oesophageal stenosis by decreasing the inflammatory response, while the purpose of antibiotherapy was to reduce the risk of infection associated to the administration of high doses of corticosteroids.2–5
In recent years, numerous studies have been conducted with the aim of proving or refuting the protective effect of steroid therapy in these patients. At present, it is generally believed that there is sufficient scientific evidence to recommend the use of high doses of dexamethasone in patients with confirmed grade IIb oesophageal burns following ingestion of a caustic substance or patients with airway involvement.6–9 However, its efficacy and safety in all other patients are still under debate, and international guidelines do not recommend its routine use, restricting this intervention to select patients.6–8,10
The aim of our study was to determine the safety and benefits of implementing a less aggressive protocol in patients at low risk of caustic injury.
Materials and methodsWe conducted an observational and analytical study in a PED of a tertiary women's and children's hospital that manages approximately 100000 paediatric visits a year. We included all patients aged less than 18 years who sought care for ingestion of a caustic substance between January 2011 and December 2015. To this end, we reviewed the health records of all patients with a documented reason for the visit or a final diagnosis related to exposure to a toxic substance.
We defined caustic substance as any substance with a pH of 3.5 or lower, or a pH of 12.5 or greater, as well as products with an unknown pH or a pH outside the defined range in patients presenting with symptoms and/or signs indicative of caustic injury.
The usual protocol for the management of caustic ingestion in the PED under study was hospital admission with fasting, analgesia, gastroprotection and parenteral steroid therapy and antibiotherapy. Once admitted, the patient underwent evaluation by a gastroenterologist, who decided whether performance of oesophagogastroduodenoscopy (OGD) was necessary based on the findings of the history taking, physical examination and/or the persistence of symptoms.
A less aggressive protocol for the management of low-risk patients was introduced in June 2013. Low risk was defined, based on an evaluation of risk factors for gastrointestinal lesions previously performed in the PED,11 as meeting all of the following criteria: unintentional ingestion, absence of symptoms, absence of vomiting (spontaneous or induced) and absence of oral lesions. These patients were kept nil per os until 6h had elapsed from ingestion of the substance, after which tolerance of oral intake was tested. If patients exhibited adequate tolerance, they could be discharged home without need of hospital admission or diagnostic tests. The usual protocol was still applied to patients who were not considered low-risk, and the gastroenterologist determined whether an OGD was necessary.
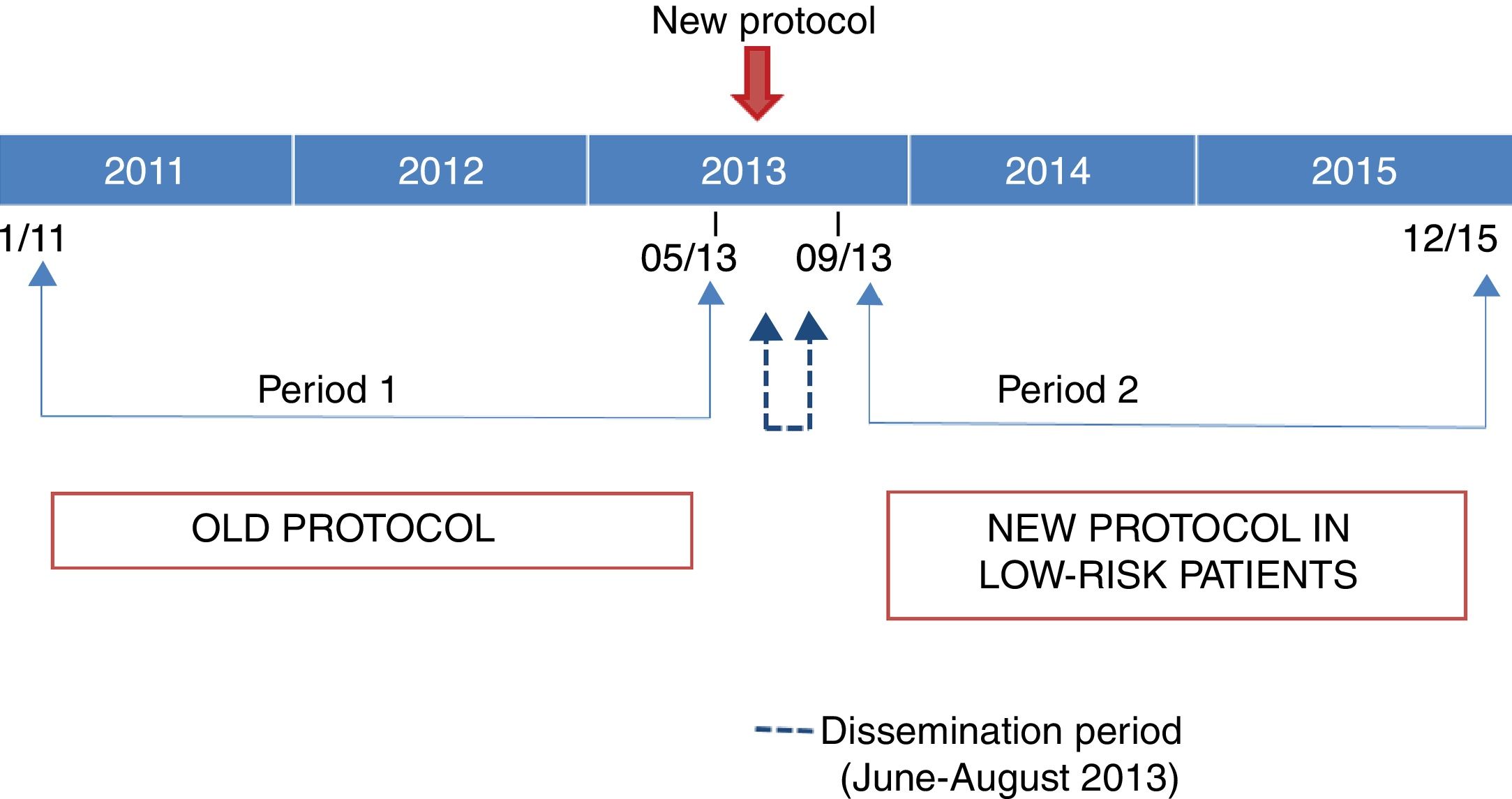
We classified the patients in the sample into 2 groups based on the period when they were managed (before or after the introduction of the new protocol). Period 1 went from January 1, 2011 to May 31, 2013 (2.5 years) and period 2 from September 1, 2013 to December 31, 2015 (2.4 years). The 3 intervening months (June 1, 2013 to August 31, 2013) were the months when the new protocol was being introduced, and we considered them a transitional period.
Fig. 1 shows the distribution of the periods included in the study based on the protocol in use.
Through the retrospective review of electronic health records, we collected data on epidemiological, clinical and management variables. We graded gastrointestinal lesions based on the Zargar classification.12 We considered the need of readmission with performance of an OGD for diagnosis of gastrointestinal lesions a complication. For each patient, we searched the regionwide public health care database of Catalonia for a period of at least 2 months following the ingestion to verify that the patient had not been readmitted in a different hospital.
To determine the positive impact of the implementation of the new protocol, we assessed the adherence to the current protocol in each period and retrospectively estimated how many patients in the first period could have benefitted from the application of the new protocol.
We entered and processed the extracted data in a relational database (Microsoft Access, Microsoft Corporation, Redmond, USA). The statistical analysis was performed with the software SPSS version 21.0 for Windows, using tests to analyse the distribution of the data (Kolmogorov–Smirnov) and to compare quantitative data (Mann–Whitney U) and qualitative data (chi square, contingency table, Fisher exact test). We considered P-values of less than .05 statistically significant.
The study was approved by the research ethics board of our hospital.
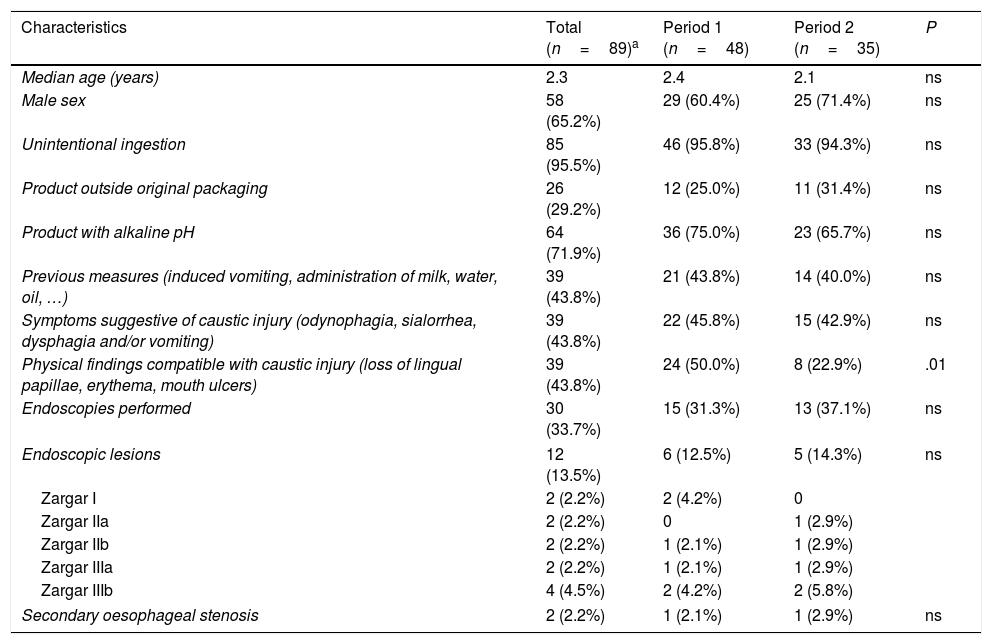
ResultsThe sample included 89 cases of caustic substance ingestion out of a total of 487 099 visits managed at the PED during the period under study (0.02%). Forty-eight patients were managed in period 1 and 35 in period 2; 6 patients were managed during the transitional period (when the protocol was being introduced). Table 1 presents the epidemiological and clinical characteristics of patients overall and by period under study. Two patients developed secondary oesophageal stenosis. Both patients had ingested degreasers (with a pH of 12.5 and 14, respectively) and presented with manifestations suggestive of caustic injury (odynophagia, sialorrhoea, vomiting and oral lesions), and the initial OGD found Zargar grade IIIa-b lesions.
Epidemiological and clinical characteristics of patients that sought care for suspected ingestion of a caustic substance.
| Characteristics | Total (n=89)a | Period 1 (n=48) | Period 2 (n=35) | P |
|---|---|---|---|---|
| Median age (years) | 2.3 | 2.4 | 2.1 | ns |
| Male sex | 58 (65.2%) | 29 (60.4%) | 25 (71.4%) | ns |
| Unintentional ingestion | 85 (95.5%) | 46 (95.8%) | 33 (94.3%) | ns |
| Product outside original packaging | 26 (29.2%) | 12 (25.0%) | 11 (31.4%) | ns |
| Product with alkaline pH | 64 (71.9%) | 36 (75.0%) | 23 (65.7%) | ns |
| Previous measures (induced vomiting, administration of milk, water, oil, …) | 39 (43.8%) | 21 (43.8%) | 14 (40.0%) | ns |
| Symptoms suggestive of caustic injury (odynophagia, sialorrhea, dysphagia and/or vomiting) | 39 (43.8%) | 22 (45.8%) | 15 (42.9%) | ns |
| Physical findings compatible with caustic injury (loss of lingual papillae, erythema, mouth ulcers) | 39 (43.8%) | 24 (50.0%) | 8 (22.9%) | .01 |
| Endoscopies performed | 30 (33.7%) | 15 (31.3%) | 13 (37.1%) | ns |
| Endoscopic lesions | 12 (13.5%) | 6 (12.5%) | 5 (14.3%) | ns |
| Zargar I | 2 (2.2%) | 2 (4.2%) | 0 | |
| Zargar IIa | 2 (2.2%) | 0 | 1 (2.9%) | |
| Zargar IIb | 2 (2.2%) | 1 (2.1%) | 1 (2.9%) | |
| Zargar IIIa | 2 (2.2%) | 1 (2.1%) | 1 (2.9%) | |
| Zargar IIIb | 4 (4.5%) | 2 (4.2%) | 2 (5.8%) | |
| Secondary oesophageal stenosis | 2 (2.2%) | 1 (2.1%) | 1 (2.9%) | ns |
ns: not significant.
Includes 6 patients in the transition period (June 1, 2013 to August 31, 2013). Period 1: January 1, 2011 to May 31, 2013 (customary protocol for caustic ingestion). Period 2: September 1, 2013 to December 31, 2015 (less aggressive protocol for management of caustic ingestion in low-risk patients).
We found a proportion of adherence to the protocol of 60.4% in period 1 and 71.4% in period 2 (P=.3).
Of the 35 patients managed in period 2, 13 (37.1%) met the low-risk criteria. All of them were managed with the new protocol (100% adherence) and sent home after adequate oral tolerance was verified. None required readmission or evaluation by OGD at a later time.
Retrospectively, we categorised as low-risk 6 patients in period 1 (14.6%) and 1 patient in the transitional period. Two of these patients received corticosteroids and antibiotics, and none underwent an endoscopy.
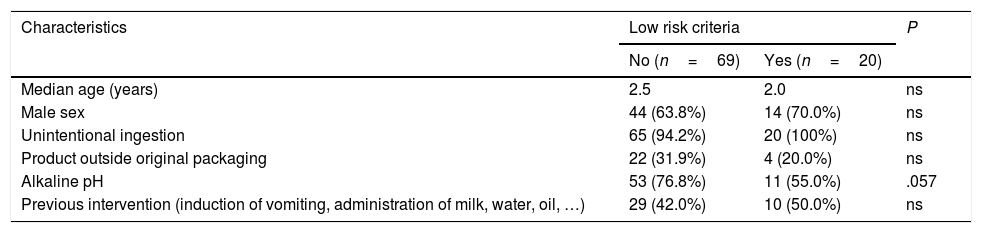
Table 2 compares the epidemiologic characteristics of patients that could be considered at low risk with the rest of the patients.
Comparison of epidemiologic characteristics of patients that sought care for suspected ingestion of a caustic substance based on whether they met or did not meet the criteria for low risk of gastrointestinal lesions.
| Characteristics | Low risk criteria | P | |
|---|---|---|---|
| No (n=69) | Yes (n=20) | ||
| Median age (years) | 2.5 | 2.0 | ns |
| Male sex | 44 (63.8%) | 14 (70.0%) | ns |
| Unintentional ingestion | 65 (94.2%) | 20 (100%) | ns |
| Product outside original packaging | 22 (31.9%) | 4 (20.0%) | ns |
| Alkaline pH | 53 (76.8%) | 11 (55.0%) | .057 |
| Previous intervention (induction of vomiting, administration of milk, water, oil, …) | 29 (42.0%) | 10 (50.0%) | ns |
The ingestion of caustic products continues to be a reason for visits to the PED that may result in severe permanent sequelae. The most salient epidemiologic characteristics in our study were the high proportion of cases in which the product had not been stored in the original packaging (29.2%), and the proportion of patients in whom family members carried out interventions that are not indicated for this problem (43.8%). It is alarming that these results are similar or worse than those found in a previous study by Rodríguez Guerineau et al.11 conducted in the same PED between 2005 and 2010 (16.7% and 46.1%, respectively). This shows that the need to implement interventions to improve health education in families continues to be unmet.
When we compared the epidemiological characteristics of patients based on whether they did or not meet the low-risk criteria, we found a lower proportion of patients that had ingested products with an alkaline pH in the low-risk group. This finding was consistent with those of other authors that found an association between greater alkalinity and a greater likelihood of lesions,13–15 although other studies found a highly acidic pH to be an independent risk factor for mortality after ingestion of caustic substances.16
When it comes to hospital management, our findings support the safety and beneficial effect of selecting patients at low risk of gastrointestinal lesions. All patients that were considered low risk and treated conservatively had favourable outcomes. If these selection criteria had been applied to the patients analysed in the first period under study, parenteral drug administration and hospital admission could have been avoided in many cases, sparing patients unnecessary inconvenience and reducing the associated costs.
On the other hand, the implementation of a less aggressive protocol improved adherence on the part of health professionals, with an adherence of 100% observed in the group of low-risk patients. The proportions of adherence to the customary protocol suggest that the paediatricians in the PED consider it excessively aggressive and prefer, in some instances, to maintain a watchful waiting approach until the patient can be evaluated in the gastroenterology department. As is the case of the low-risk protocol, this approach is consistent with the findings of studies published in recent years, which recommend the selection of patients at high-risk of gastrointestinal lesions for performance of OGD, and determining whether parenteral anti-inflammatory treatment is indicated based on its findings.
Two recent systematic reviews (Bird et al.2 and Bonnici et al.16) have concluded that adults who are asymptomatic after ingestion of a caustic substance do not require any diagnostic tests or hospital admission. In paediatric patients who ingested the substance unintentionally and are asymptomatic, a period of observation is recommended to increase safety, as well as verification that these patients remain asymptomatic after reintroducing oral intake. Bonnici et al. also analysed the usefulness of computed tomography to diagnose caustic injuries. These authors consider that there is not sufficient evidence to have computed tomography replace OGD as the gold standard, but that this method may be an adequate alternative when OGD is not safe (for instance, in cases of upper airway oedema) or cannot be performed (lack of an endoscopist).
The consensus guidelines of the World Society of Emergency Surgery,10 the European Society of Gastrointestinal Endoscopy (ESGE) and the European Society for Paediatric Gastroenterology Hepatology and Nutrition7,8 recommend performance of an OGD, within the first 24h only if the patient presents symptoms indicative of injury by a caustic substance. A watchful waiting approach is recommended in asymptomatic patients that can be followed up. The guidelines also recommend administration of a short course of high-dose dexamethasone (3 days) in patients with respiratory symptoms or grade IIb oesophagitis for prevention of secondary stenosis. This recommendation is based on the fact that these lesions are associated with the highest probability of producing stenosis and are not transmural lesions, so that they can still respond to anti-inflamatory treatment.6–10,13 We must use these recommendations as a guide to restrict the use of corticosteroids following caustic ingestion.
The main limitation of our study involves its retrospective design, which can result in missing data. Although we reviewed the regionwide electronic health record database of Catalonia to detect potential additional visits to other health care facilities, we cannot rule out the possibility that patients sought care in private hospitals whose records are not included in this database. However, the reference centres for performance of paediatric OGD in Catalonia are mainly public hospitals, so it is unlikely that this information was missing from the source. Another important limitation is the small number of low-risk patients, although we believe that the fact that none of the patients managed with the conservative approach developed complications is significant. Lastly, our study was conducted in a single centre, and therefore it may not be possible to extrapolate its results.
In conclusion, the results suggest that it is safe to adopt a more conservative approach in the management of low-risk patients. These patients benefit from clinical observation and the avoidance of more aggressive interventions that could give rise to iatrogenic adverse events.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Ripoll Trujillo N, Martínez Sánchez L, Habimana Jordana A, Trenchs Sainz de La Maza V, Vila Miravet V, Luaces Cubells C. Ingesta de cáusticos: análisis de la seguridad y beneficio de un protocolo menos agresivo. An Pediatr (Barc). 2019;90:207–212.