Changes in lifestyle and diet have led to a progressive increase in the prevalence of overweight and obesity. This disorder can lead to significant physical and psychosocial effects that affect the health related quality of life (HRQOL). Adolescence is a time of great vulnerability and very decisive in personality development. The objective of this study was to assess the influence of weight status on HRQoL in adolescents.
Population and methodsA cross-sectional study conducted on adolescents of 12–16 years old and an assessment of HRQOL using the CHIP-Adolescents Edition questionnaires.
ResultsOut of a total of 89 adolescents included, 60.7% had a normal weight and 39.3% were overweight–obese. The normal weight participants had a higher mean age than overweight–obesity participants, 14.2 vs. 13.6 years old, respectively. There were no other differences in sociodemographic characteristics between groups. Overweight–obese adolescents had a worse HRQoL, specifically as regards less resilience, lower capacity for physical activity, less family involvement, and greater peer influence. Moreover, the girls showed a lower self-esteem, satisfaction, resilience and physical activity than boys. Furthermore, less home safety and health, higher individual risk and greater peer influence was reported with increasing age of participants.
ConclusionOverweight–obesity negatively affects the HRQoL of adolescents. It is important to evaluate the psychosocial aspects from the perspective of the adolescents, in order to offer them a complete, personalised and multidisciplinary care.
Los cambios en el estilo de vida y la alimentación han conllevado un aumento progresivo de la prevalencia del sobrepeso-obesidad. Esta enfermedad puede conllevar importantes repercusiones físicas y psicosociales que deterioran la calidad de vida relacionada con la salud (CVRS). La adolescencia es una etapa de gran vulnerabilidad por el entorno y muy determinante en el desarrollo de la personalidad del individuo. El objetivo fue evaluar la influencia del estado ponderal en la CVRS de los adolescentes.
Población y métodosEstudio transversal de adolescentes de 12 a 16 años. Evaluación de la CVRS mediante los cuestionarios CHIP-Adolescent Edition.
ResultadosOchenta y nueve adolescentes, 60,7%, eran normoponderales y el 39,3% tenía sobrepeso-obesidad. Los participantes normoponderales tenían una edad media superior a los participantes con sobrepeso-obesidad, 14,2 frente a 13,6 años, respectivamente. No había otras diferencias entre las características sociodemográficas de ambos grupos. Los adolescentes con sobrepeso-obesidad reflejaron peor CVRS, concretamente refirieron menor resistencia, menor capacidad de actividad física, menor participación familiar y mayor influencia de sus iguales. Asimismo, las chicas reflejaron menor autoestima, satisfacción, resistencia y capacidad de actividad física que los chicos. Por otro lado, a medida que aumentaba la edad de los participantes, referían menor salud y seguridad en el hogar, mayor riesgo individual y mayor influencia de sus iguales.
ConclusiónEl sobrepeso-obesidad repercute negativamente en la CVRS de los adolescentes. Consideramos importante evaluar los aspectos psicosociales desde la perspectiva del paciente para poder ofrecerle una atención personalizada y multidisciplinar.
Overweight–obesity is an endemic disease in developed countries. They are the most frequent metabolic disorders in the western world. The World Health Organization believes that it constitutes a serious public health problem and has labelled it as the pandemic of the XXI century.1 According to the last national survey conducted in Spain, the Encuesta Nacional de Salud de España 2011–2012, the prevalence of overweight in the 2–17 year old population is of 18.26%, and the prevalence of obesity of 9.56%. The figures specific to the Autonomous Community of Navarra for this age group show a prevalence of overweight and obesity of 15.79% and 7.81%, respectively.2
The aetiology of obesity has been subject to numerous studies. Nowadays, it would be more accurate to speak of “obesities” than of “obesity”, as there is evidence that it can be due to endogenous or exogenous causes; be a primary disease or develop secondary to another condition; or be a monogenic or polygenic trait.3 The literature has described numerous clinical and metabolic complications associated with excess body fat, both in the short and the long term: insulin resistance, hypercholesterolaemia, type 2 diabetes mellitus, metabolic syndrome, polycystic ovary syndrome, or cardiovascular disease.4,5 Excess body fat is also associated with behavioural and psychosocial complications: eating disorders, anxiety, depression, dependence, passivity, poor academic performance, social isolation, real or perceived discrimination, and low self-esteem.6–8
The concept of health encompasses more than the absence of disease. In children and adolescents, the concept of health has certain characteristics, as stated by Starfield: “The measurement of health in children should consider their capacity to fully participate in physical, social, and psychosocial activities and functions adequate to their age.”9 The concept of health-related quality of life (HRQoL) entered the healthcare field in the 1970s, and stemmed from the belief that patient wellbeing and how patients experience their disease and the medical care they receive are important factors to consider during treatment and followup.10,11 Adolescence is a key stage in the development of an individual's personality and traits, and it is a very vulnerable period during which individuals are particularly susceptible to beneficial and deleterious environmental factors. As noted above, overweight and obesity have a significant impact on overall HRQoL and on self-esteem, physical wellbeing, and emotional wellbeing in particular.
There are studies about the impact of overweight–obesity on the HRQoL of adolescents, but so far none have been conducted in Spain. Our hypothesis was that overweight and obesity may have physical and psychosocial consequences that are detrimental to the HRQoL of adolescents. The aim of this study was to analyse the scores obtained by adolescents 12–16 years of age for different aspects of HRQoL and assess whether there are differences associated with sociodemographic characteristics or weight status.
Patients and methodsStudy designWe performed a descriptive, observational, cross-sectional study.
Ethical considerationsThe study was approved by the research ethics committee of our hospital in March 2010.
Study sample and participantsWe included adolescents of both sexes (45 male and 44 female) 12–16 years of age with normal weight, overweight or obesity that received care in our general paediatrics department or care for overweight or obesity in the paediatric endocrinology department of our hospital between April 1, 2010 and December 15, 2011, and who agreed to their voluntary participation in the study.
We provided information about the study and obtained the informed consent of the parents of the participants and the written consent of the adolescents, who were considered minors capable of consenting, at the hospital. We reviewed the medical and anthropometric data and provided the questionnaire used to assess HRQoL, the Child Health and Illness Profile-Adolescent Edition (CHIP-AE).
Inclusion criteria: age 12–16 years, voluntary agreement to participate in the study, as well as written informed consent from legal guardians and participants.
Exclusion criteria: presence of acute or chronic disease other than overweight–obesity that affected the HRQoL of the patient, or not giving consent or revoking it at any time during the study.
Withdrawal criteria: inability to fill out the questionnaires properly or insufficient number of answered questions.
The sample size was calculated in relation to the 32 patients 12–16 years of age with overweight–obesity that were being followed up in the paediatric endocrinology department. Taking into account potential losses and new diagnoses, we estimated a minimum sample size of 35 cases and at least one control per case.
We established the 12–16 years of age interval to avoid mixing preadolescents and adolescents. When we included the control group the purpose was to ensure that the two groups that we were to compare would have a similar social background.
The participants (n=89) were classified according to the body mass index (BMI) calculated in the hospital using the standards established by Ferrández-Longás et al. (1980–2002)12 as a reference. We used the BMI because it is a good correlate for the amount of body fat assessed by means of computer tomography or magnetic resonance imaging, which are the gold standards in body fat measurement. Participants with a BMI below the 85th percentile for their age and sex were classified as having a normal weight, participants with a BMI equal or greater than the 85th and below the 95th as overweight, and participants with a BMI above the 95th percentile as obese.13
Measurement of health-related quality of lifeWe used the adolescent edition of the CHIP self-administered questionnaire, developed by the Johns Hopkins Bloomberg School of Public Health.14 This is the first self-reported health assessment tool based on a multidimensional concept of health specifically designed for adolescents that has been published in the medical literature.15 The reliability and validity of the Spanish version have been demonstrated.16 The CHIP-AE is addressed to adolescents 12–16 years of age. The questionnaire is organised into 5 domains, each of which comprises information on the aspects listed in parentheses: satisfaction (self-esteem, self-perception, satisfaction with oneself and one's own health), discomfort (physical comfort, emotional comfort, and limitations of daily activity), resilience (family involvement, problem solving abilities for issues characteristic of this age, resilience in physical activity, and health and safety in the home environment), risk avoidance (engagement in risk activities, attitudes that threaten achievement, and peer influences) and achievement (academic achievement and achievement in age-appropriate responsibilities). The questionnaire also has 14 subdomains that provide detailed information of each of the domains (see Table 1).17
Scores of the CHIP-AE questionnaire domains and subdomains by weight status.
| Normal weightn=54 | Overweight–obesityn=35 | Conventional analysis | Adjusted analysis** | ||
|---|---|---|---|---|---|
| P value* | P value | Significant model for | |||
| Satisfaction | 57.41 (51.39–60.2) | 55.5 (51.1–60.5) | .537 | .263 | Sex (female)# |
| Satisfaction with health | 54.55 (7.62) | 54.01 (7) | .738 | .257 | |
| Self-esteem | 58.02 (52.81–59.76) | 56.28 (49.34–59.76) | .503 | .42 | Sex (female) |
| Discomfort | 57.69 (52.45–61.91) | 59.9 (57.41–63.54) | .134 | .251 | |
| Physical comfort | 57.55 (51.83–61.47) | 59.41 (55.58–62.67) | .151 | .145 | |
| Emotional comfort | 57.9 (50.87–63.76) | 57.9 (55.56–64.35) | .306 | .51 | |
| Limitation of activity | 54.71 (51.24–58.17) | 58.17 (54.71–58.17) | .386 | .357 | |
| Resilience | 59.82 (55.56–63.09) | 54.75 (53.57–61.41) | .022 | .003 | Sex (female) |
| Family involvement | 57.25 (53.77–62.48) | 55.11 (49.42–58.99) | .092 | .017 | |
| Problem solving | 52.11 (47.19–54.56) | 49.65 (44.74–57.02) | .591 | .607 | |
| Physical activity | 53.53 (8.54) | 50.73 (8.58) | .135 | .04 | Sex (female) |
| Home safety and health | 58.52 (5.33) | 58.13 (5.17) | .75 | .329 | Age (older) |
| Risk avoidance | 61.11 (56.62–64.07) | 61.92 (59.28–64.86) | .467 | .704 | Age (older) |
| Individual risks | 61.48 (57.54–63.3) | 62.09 (58.75–63.45) | .384 | .774 | Age (older) |
| Threats to achievement | 55.6 (51.02–60.18) | 57.89 (55.03–61.33) | .047 | .229 | |
| Peer influences | 62.63 (56.69–65.59) | 59.66 (56.69–65.59) | .479 | .024 | Age (older) |
| Achievement | 10.53 (5.9–16.72) | 8.98 (2.02–12.08) | .179 | .417 | |
| Academic achievement | 61.48 (10.51) | 58.48 (11.25) | .204 | .106 | |
| Work achievement | −16.0 (−16.0 to −16.0) | −16.0 (−16.0 to −16.0) | .529 | .923 | |
The score correlates positively with health: a higher score is indicative of greater satisfaction and wellbeing, fewer risks, etcetera. Participants had to answer at least 70% of the questions in each domain or subdomain.18
Data collectionThe independent variables under consideration were (1) sex; (2) age; (3) anthropometric variables measured at the hospital with participants in underwear: weight measured in kilograms with TANITA® scales accurate to 0.05kg; height measured in centimetres with a Harpender stadiometer accurate to 0.1cm and with the participant standing barefoot with the heels, buttocks, shoulder blades and occiput touching the stadiometer; BMI, defined as the weight in kilograms divided by the squared height in metres; (4) personal history (diseases, allergies, treatments, surgeries); (5) nutrition-specific followup: we requested a 7-day food count and checked whether it adhered to the recommendations given at the hospital according to their normal or overweight–obesity status; we considered that the patient did not comply with the recommendations if they did not follow them 2 or more times a day and 3 or more days a week; and (6) socioeconomic status measured with The Family Affluence Scale II, which asks about the presence and number of family cars, individual bedrooms, holidays, and computers in the participant's household; the scale is considered appropriate to assess a family's expenditure and consumption; the sum of the values obtained in each section is used to categorise socioeconomic status as low (score, 0–3), middle (4–6) or high (7 or greater).19
The dependent variables were the domains and subdomains into which the information obtained through the questionnaire is organised (see Table 1).
Statistical analysisWe assigned consecutive code numbers to the questionnaires to ensure the confidentiality and anonymity of the participants.
We performed a descriptive analysis of the sociodemographic characteristics of the groups to compare, normal weight versus overweight–obesity. Categorical variables were compared by means of the chi square test. Quantitative variables with a normal distribution were compared using Student's t test, and continuous variables that did not have a normal distribution using the Mann–Whitney U test.
We performed a multivariate multiple regression analysis of the scores obtained in the different domains and subdomains relative to weight status and adjusted for sex, age and socioeconomic status.
We have used error plots for the graphical representation of quantitative variables with a normal distribution, and box plots for quantitative variables that did not follow a normal distribution.
The statistical analysis was performed with IBM SPSS Statistics version 20.0 (Chicago) for Windows.
ResultsOf the 99 adolescents that were asked to participate in the study, 7 declined. Of the 92 adolescents that agreed to participate, 3 were withdrawn because they did not answer the required minimum number of questions. The final sample included 89 adolescents of both sexes, 12–16 years of age. Of all participants, 54 were classified as having normal weight, and 35 as having overweight–obesity. Table 2 shows the sociodemographic characteristics of the participants.
Sociodemographic characteristics of the sample.
| Normal weightn=54 (60.7%) | Overweight–obesityn=35 (39.3%) | P value* | |
|---|---|---|---|
| Sex | |||
| Male | 30 (55.6%) | 14 (40%) | .152 |
| Female | 24 (44.4%) | 21 (60%) | |
| Age | 14.2 (1.32) | 13.6 (1.18) | .022 |
| Socioeconomic status | |||
| Low-middle | 35 (64.8%) | 19 (54.3%) | .321 |
| High | 19 (35.2%) | 16 (45.7%) | |
| BMI SDs** | −0.36 (−0.78 to 0.33) | 2.07 (1.78 to 3.25) | <.001 |
P-values for chi square test for categorical variables (expressed as absolute frequency and percentage), Student's t test for normally distributed continuous variables (expressed as mean and standard deviation) and Mann–Whitney U test for non-normally distributed variables (expressed as median and IQR).
We found significant differences between the weight status groups in the compliance with the dietary recommendations. Of all participants with overweight–obesity, 45.7% were in compliance, compared to 1.9% of participants with normal weight (P<.001).
The multivariate analysis of the scores of the domains and subdomains by weight status and adjusted for sex, age and socioeconomic status revealed that adolescents with overweight–obesity had less resilience (P=.003), less family involvement (P=.017), less capacity for physical activity (P=.04) and more peer influences (P=.024) (Fig. 1).
Furthermore, the multivariate analysis showed that the scores obtained by girls were significantly lower than those of boys in the satisfaction (P=.001) and resilience (P=.001) domains, and in the self-esteem (P<.001) and physical activity (P<.001) subdomains (Fig. 2).
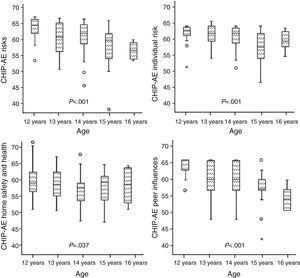
The multiple linear regression analysis showed that as the age of participants increased, they obtained lower scores in the risks domain (P<.001) and in the home health and safety (P=.037), individual risk (P=.001) and peer influences (P<.001) subdomains (Fig. 3).
DiscussionSeveral authors have assessed the psychosocial consequences of overweight and obesity in adolescents, but there are few studies on the impact of excess weight in their HRQoL. We must nevertheless take into account that psychosocial aspects are, in fact, part of HRQoL.
The works of Mirza et al. and Sjoberg et al. show that excess weight in adolescence leads to body dissatisfaction, low self-esteem and a higher incidence of depression, which are more pronounced in female adolescents.20,21 The study by Al-Akour et al. conducted in Jordan as well as the study by Beer et al. conducted in the Netherlands showed an association between the presence of overweight–obesity and lower scores in every aspect of HRQoL.22,23 Keating et al. specifically analysed the consequences of excess weigh on physical aspects and observed that overweight and obese patients obtained significantly lower scores compared to patients with normal weight.24 According to the review by Griffiths et al., as BMI increases, self-esteem and HRQoL decrease.25,26 The results that we present here are consistent with all of the above.
Still, weight status in not the sole determinant of HRQoL. The differences in perception between the sexes have a considerable impact on its consequences on HRQoL. Several studies have reported that the influence of body image, social acceptance and mood impairment is stronger in female than in male adolescents, which makes girls more vulnerable to psychosocial disorders.20,24,27,28 These differences were also observed in our study, as girls reported lower satisfaction, self-esteem, resiliency and physical capacity than boys.
Excess weight often elicits teasing from peers. The increased influence of the environment combined with perceived teasing and bullying lead to greater insecurity, lower self-esteem and emotional wellbeing, and more difficult interpersonal relationships.29,30 As children grow they become more aware of their environment and of interpersonal differences; self-criticism increases and negative self-perceptions and self-dissatisfaction develop, negatively affecting HRQoL. The decrease in self-esteem leads to increased peer influence and a reduced perceived social acceptance. These aspects may lead to a more introverted character that, as our results demonstrate, may reduce family involvement. The reduced interaction with the family may delay finding the help that the adolescent needs.29,31,32
To date, there are no other published studies of this nature conducted on the adolescent population in Spain. A European multicentre study on the impact of overweight on the HRQoL of participants 8–18 years of age included a representative sample of 714 individuals from Spain; the study concluded that overweight and obesity have deleterious effects on HRQoL, especially on physical comfort and self-perception.33
The anthropometric measurements were taken at the hospital by trained staff, as opposed to self-reported. None of the participants had IBM values at the border between normal weight and overweight–obesity, which guarantees that the groups were separated correctly.
The main limitation of this study is its cross-sectional design, which can establish correlation but not causality. Furthermore, we used a convenience sample because those participants could then be considered for health-promoting interventions, but this means that the sample may not be representative of the adolescent population of Navarra. There may also be a selection bias, as the adolescents with overweight–obesity that seek care in the endocrinology department may have a greater awareness of the repercussions of their disease. One of the main biases to consider is the observer bias: since participants are aware of being questioned, they give more favourable responses in regards to their health status. However, this potential confounding factor would not invalidate the results of this study, since were it not at play, the differences found in the study would be even greater.
ConclusionOverweight–obesity has a detrimental effect on the HRQoL of adolescents, but it must be taken into account that sex and age have a significant impact on the decrease of HRQoL.
The stronger influence of body image and social acceptance in women makes them more vulnerable to psychosocial disorders. These negative perceptions already occur in female adolescents and have an influence on the development of their personality and behaviour.
We believe that in order to offer patients personalised and multidisciplinary care it is crucial that we know the subjective perception and impact of their health status, and to assess the emotional and psychosocial features related to health from the perspective of the paediatric patient.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Herranz Barbero A, López de Mesa MR, Azcona San Julián C. Influencia del exceso de peso en la calidad de vida relacionada con la salud de los adolescentes. An Pediatr (Barc). 2015;82:131–138.
Previous presentation: the results of this study were presented in part as an oral communication under the title “Repercusión del sobrepeso y la obesidad en la calidad de vida relacionada con la salud de los adolescentes” at the 61 Congreso de la Asociación Española de Pediatría; May 31–June 2, 2012; Granada, Spain.