Breast milk is the optimal food during the first months of life. The main objective was to analyse the factors associated with not initiating breastfeeding in terms of maternal lifestyles, epidemiological characteristics and information on breastfeeding.
Material and methodObservational analytical study of cases and controls in 6 primary care centres. The sample included women with a child under 5 years, with an estimated necessary sample size of 166 cases (women who did not initiate breastfeeding) and 166 controls (women who began breastfeeding). Sociodemographic and maternal lifestyle variables were measured before and during pregnancy, such as physical activity using the BPAAT questionnaire, diet with the MEDAS-14 questionnaire, and tobacco and alcohol consumption. We assessed the information and opinions about breastfeeding as well as previous experience with it.
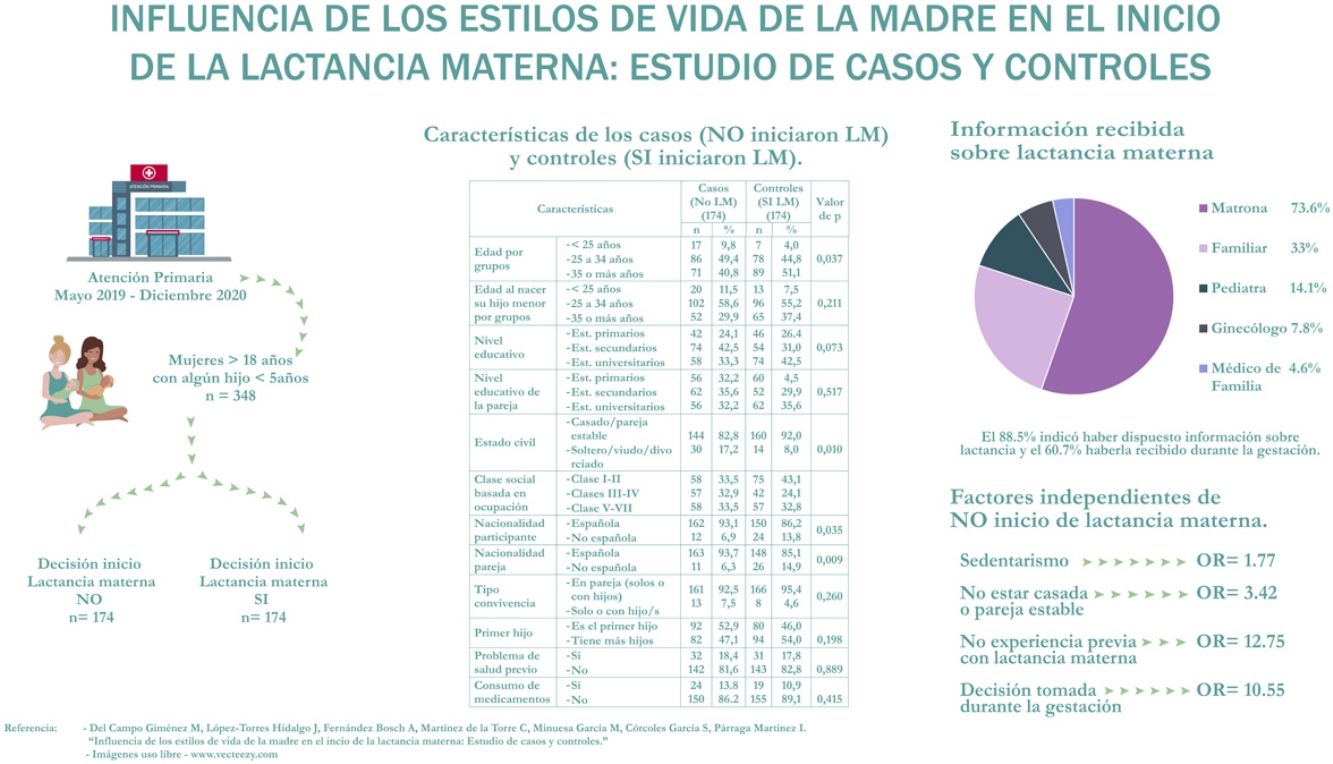
ResultsThe study included 348 women (174 cases and 174 controls) with a mean age of 33.4 years (SD, 5.4). The variables independently associated with not initiating breastfeeding were: absence of previous experience with breastfeeding (odds ratio [OR], 12.75), making the decision during pregnancy or delivery (OR, 10.55), not being married or in a partnership (OR, 3.42) and being sedentary for periods of 2 hours or greater/day during pregnancy (OR, 1.77).
ConclusionsIn our study, the determining factors associated with not initiating breastfeeding were the lack of previous experience with breastfeeding, the timing of the decision about breastfeeding, and marital status. When it came to lifestyle, only a sedentary lifestyle was associated with not initiating breastfeeding, while dietary or other habits had no influence.
La lactancia materna es la alimentación óptima durante los primeros meses de vida. El objetivo principal fue analizar los factores relacionados con no iniciar la lactancia materna, tanto referidos a los estilos de vida maternos como a las características epidemiológicas y la información sobre lactancia.
Material y métodoEstudio analítico observacional de casos y controles en seis Centros de Salud. Se seleccionaron mujeres con algún hijo menor de 5 años, estimando un tamaño muestral de 166 casos (mujeres que no iniciaron lactancia materna) y 166 controles (que iniciaron lactancia). Se midieron variables sociodemográficas y estilos de vida maternos antes y durante la gestación como la actividad física mediante el cuestionario BPAAT, la dieta con el cuestionario MEDAS14 y el consumo de tabaco y alcohol. Se valoró la información y opiniones sobre lactancia, así como la experiencia previa.
ResultadosSe incluyeron 348 mujeres (174 casos y 174 controles) con una edad media de 33,4 años (DE:5,4). Fueron variables asociadas de manera independiente con no iniciar lactancia: ausencia de experiencia previa con lactancia (OR:12,75), tomar la decisión durante la gestación o parto (OR:10,55), no estar casada o con pareja (OR:3,42) y permanecer sedentaria ≥2 horas/día durante la gestación (OR:1,77).
ConclusionesEn nuestro estudio, los factores determinantes que se asocian a no iniciar lactancia materna son la ausencia de experiencia previa con lactancia, el momento de la decisión sobre la lactancia y el estado civil. Entre los estilos de vida, solo el sedentarismo se asocia a no iniciar lactancia materna, mientras que no tienen influencia los hábitos alimentarios u otros
Breastmilk covers the nutritional needs of the newborn, facilitating the maturation process.1 Thus, the World Health organization recommends exclusive breastfeeding in the first 6 months of life, followed by breastfeeding combined with complementary foods through at least age 2 years.2 Formula feeding in infancy is associated with an increased risk of morbidity, a higher incidence of infection and an increased mortality.3
Early initiation of breastfeeding is associated with a lower neonatal mortality4 and with a longer duration of breastfeeding.5 Although the benefits of breastfeeding to the child and the mother are well known, a considerable proportion of women choose not to breastfeed.5,6
The results of nationwide studies in Spain show a prevalence of initiation of exclusive breastfeeding of 77% and of mixed feeding of 88%.6
On the other hand, considering maternal lifestyles before and during breastfeeding may be useful, as the maternal weight, level of activity and metabolism will determine the dietary intake each particular woman requires to achieve an optimal nutritional status. The importance of the diet has been addressed in relation to specific nutrients, food groups and specific dietary patterns. Thus, among the patterns considered healthy, the Mediterranean diet is the one supported most strongly by the current evidence and is one of the patterns that should be recommended.7 In consequence, establishing the degree of adherence to the Mediterranean diet could be helpful to assess the quality of the diet in women before and during gestation.
Although not every lifestyle habit has been studied in relation to the decision to initiate breastfeeding, there is evidence that smoking has a negative impact on breastfeeding initiation and duration.8 Obesity is also negatively correlated to breastfeeding initiation and maintenance in the first year post birth.9
In short, breastfeeding is considered the optimal nutrition during infancy. Different clinical practice guidelines and national and international public health and social welfare institutions have issued recommendations on the need to implement strategies to promote breastfeeding.1 Identifying the factors associated with the lack of breastfeeding initiation is particularly relevant to allow the development of interventions to address them to be integrated in breastfeeding promotion strategies. Therefore, in light of all of the above, the aim of our study was to identify factors associated with the absence of breastfeeding initiation in mothers visiting primary care clinics, both in terms of lifestyle and in terms of epidemiological characteristics and breastfeeding education.
Material and methodsWe conducted an observational and analytical case-control study with participation of women managed in 6 health districts. The study took place between May 2019 and December 2020.
Participants were women aged 18 or more years that had a child aged less than 5 years, managed in the participating primary care centres, and who gave informed consent to participation. We excluded mothers whose children had a birth weight of less than 2500 g, were born before 37 weeks of gestation, required admission to the neonatal unit or had an illness that contraindicated breastfeeding, and mothers in whom breastfeeding was contraindicated or with language barriers that hindered comprehension of the questionnaire.
Our definition of case was a woman meeting the inclusion criteria that had a child under 5 years and who had not initiated breastfeeding. We defined breastfeeding initiation as placing the infant to the breast or feeding the infant breast milk within 48 h from birth, based on the 2017 clinical practice guidelines on breastfeeding of the Spanish Ministry of Health, Social Services and Equality.2 We included mothers who had initiated breastfeeding as controls. For the sample size calculation, we used an alpha level of 005 and a beta level of 020 (two-tailed) for the detection of a minimum odds ratio of 2, assuming a proportion of exposure in the control group of 25% and a 1:1 case-control ratio. With these parameters, we estimated that we needed 166 cases and 166 controls. Ultimately, we compared 174 cases (who did not initiate breastfeeding) to 174 controls (who initiated breastfeeding). We selected the controls from the same population from which we selected the cases through convenience sampling (selecting one control per case) of the women who made on-demand visits for any reason to participating primary care family medicine or paediatrics clinics in the 6 health care districts included in the study.
After obtaining their informed consent, we scheduled appointments for the selected participants to interview them at their respective primary care centres. The study design and procedures were approved by the Ethics Committee for Research with Medicines of the Hospital de Albacete.
We collected data through a pre-coded questionnaire designed specifically for the study, including information on the sociodemographic characteristics of the participants: current age, age at birth of the youngest child, educational attainment, marital status, socioeconomic status,10 type of household, number of offspring and nationality. We also collected data on paternal sociodemographic characteristics (educational attainment, occupation and nationality), maternal health problems (International Classification of Primary Care-2 [ICPC-2] of the World Organization of Family Doctors), child-related variables (date of birth, sex, birth weight, weeks of gestation, type of delivery, health problems) and pregnancy-related variables (childbirth education delivered by midwife, prenatal care). The breastfeeding variables under study were: initiation of breastfeeding (yes/no), timing of decision whether to breastfeed or not (before/during pregnancy), breastfeeding/lactation education, previous experience with breastfeeding (favourable/unfavourable) and maternal and paternal perception of breastfeeding (in favour/against). Last of all, we collected data on variables related to maternal lifestyle before and during pregnancy, such as physical inactivity (assessed by means of the validated Spanish version of the Brief Physical Activity Assessment Tool [BPAAT]11,12), sedentary habits (“Do you have periods of sedentary activity lasting more than 2 straight hours throughout the day?”),13 diet (Mediterranean Diet Adherence Screener questionnaire [MEDAS-14])14 and tobacco and alcohol consumption. Each answer reflecting adherence in an item of the MEDAS-14 yields 1 point, so the possible score ranges from 0 to 14. We categorised scores based on the level of adherence to the Mediterranean diet as high (11–14 points), moderate (7–10 points) and low (0–6 points).
In terms of the analysis, following data scrubbing, we performed a descriptive analysis by means of proportions, measures of central tendency and measures of dispersion as applicable based on the nature of the variables. We assessed the normality of the distribution with the Kolmogorov-Smirnov test. We carried out a bivariate analysis comparing the frequency in the case versus control group of qualitative variables by means of the χ2 test and of quantitative variables by means of the Student t or Mann–Whitney U test as applicable. The level of statistical significance was established at 5% for all analysis, and all tests were two-tailed. To assess the magnitude of the association, we calculated the crude odds ratio (OR) with the corresponding 95% confidence interval (CI). Having identified which variables were associated with the lack of breastfeeding initiation, we performed a multivariate analysis by unconditional binary logistic regression, calculating adjusted ORs. The independent variables included in the model were the sociodemographic characteristics, breastfeeding-related variables and lifestyle-related variables, and the dependent variable was the presence/absence of breastfeeding initiation. The fit of the model was assessed by means of the Hosmer–Lemeshow test. The data were analysed with the statistical software applications SPSS version 250 and Epidat version 31.
ResultsThe sample included 348 women (174 cases and 174 controls) with a mean age of 33.4 years (SD, 5.4). The participation rate was 93% (26 women declined participation). The mean age was significantly lower in the case group compared to the control group, both at the time of the interview (32.7 vs 34.2 years; P = .007) and at the time of delivery (31.7 vs 32.5; P = .038). Table 1 presents the characteristics of the cases and controls. As can be seen in the table, there were statistically significant differences between the 2 groups in marital status and in the national origin of both the participants and their partners.
Characteristics of cases and controls.
| Characteristic | Cases (no BF initiation) (N = 174) | Controls (BF initiation) (N = 174) | P | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Age group (years) | |||||
| <25 | 17 | 9.8 | 7 | 4.0 | .037 |
| 25−34 | 86 | 49.4 | 78 | 44.8 | |
| ≥35 | 71 | 40.8 | 89 | 51.1 | |
| Age at birth of the youngest child by age group (years) | |||||
| <25 | 20 | 11.5 | 13 | 7.5 | .211 |
| 25−34 | 102 | 58.6 | 96 | 55.2 | |
| ≥35 | 52 | 29.9 | 65 | 37.4 | |
| Maternal educational attainment | |||||
| Primary education | 42 | 24.1 | 46 | 264 | .073 |
| Secondary education | 74 | 42.5 | 54 | 31.0 | |
| University education | 58 | 33.3 | 74 | 42.5 | |
| Paternal educational attainment | |||||
| Primary education | 56 | 32.2 | 60 | 34.5 | .517 |
| Secondary education | 62 | 35.6 | 52 | 29.9 | |
| University education | 56 | 32.2 | 62 | 35.6 | |
| Marital status | |||||
| Married/domestic partnership | 144 | 82.8 | 160 | 92.0 | .010 |
| Single/widow/divorced | 30 | 17.2 | 14 | 8.0 | |
| Social class based on the occupation held for the longest timea | |||||
| Class I-IIb | 58 | 33.5 | 75 | 43.1 | .108 |
| Class III-IVc | 57 | 32.9 | 42 | 24.1 | |
| Class V-VIId | 58 | 33.5 | 57 | 32.8 | |
| Nationality of participant | |||||
| Spanish | 162 | 93.1 | 150 | 86.2 | .035 |
| Other | 12 | 6.9 | 24 | 13.8 | |
| Nationality of partner | |||||
| Spanish | 163 | 93.7 | 148 | 85.1 | .009 |
| Other | 11 | 6.3 | 26 | 14.9 | |
| Type of household | |||||
| Couple (alone or with children) | 161 | 92.5 | 166 | 95.4 | .260 |
| Single (alone, with a child or other individuals) | 13 | 7.5 | 8 | 4.6 | |
| First child | |||||
| Youngest was first child | 92 | 52.9 | 80 | 46.0 | .198 |
| Had previous children | 82 | 47.1 | 94 | 54.0 | |
| Pre-existing health conditions | |||||
| Yes | 32 | 18.4 | 31 | 17.8 | .889 |
| No | 142 | 81.6 | 143 | 82.8 | |
| Current medication | |||||
| Yes | 24 | 13.8 | 19 | 10.9 | .415 |
| No | 150 | 86.2 | 155 | 89.1 | |
Cases: women that did not initiate breastfeeding; controls: women that initiated breastfeeding. Statistical significance: P-value obtained in the χ2 test. Statistical significance was established at a level of 5%, so comparisons were considered significant if P < .05.
BF, breastfeeding; NK/NA, not known/no answer.
When it came to the characteristics of the child of interest, the mean birth weight was 3249.3 g (SD, 459.4) and the median duration of gestation 39 weeks (interquartile range, 38–40). There were no differences in mean birth weight or the weeks of gestation between the group that initiated breastfeeding and the group that did not. Table 2 presents the characteristics related to the pregnancy, delivery and inpatient care in both groups, classifying the data into 2 categories to obtain dichotomous variables. We found that the proportions corresponding to the delivery of prenatal care by a midwife at a primary care centre and prenatal care by an obstetrician differed between the cases and controls.
Characteristics related to pregnancy, delivery and inpatient care in the case and control groups.
| Characteristic | Cases (no BF initiation) (N = 174) | Controls (BF initiation) (N = 174) | P | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Type of delivery | |||||
| Uncomplicated | 120 | 69.0 | 126 | 72.4 | .480 |
| Caesarean section | 54 | 31.0 | 48 | 27.6 | |
| Sex of child | |||||
| Female | 87 | 50.0 | 86 | 49.4 | .915 |
| Male | 87 | 50.0 | 88 | 50.6 | |
| Health problem in child at birth that did not contraindicate breastfeeding | |||||
| Yes | 1 | 0.6 | 4 | 2.3 | .177 |
| No | 173 | 99.4 | 170 | 97.7 | |
| Follow-up in prenatal care programme | |||||
| Yes | 171 | 98.3 | 162 | 93.1 | .018 |
| No | 3 | 1.7 | 12 | 6.9 | |
| Follow-up of pregnancy in obstetrics | |||||
| Yes | 173 | 99.4 | 167 | 96.0 | .032 |
| No | 1 | 0.6 | 7 | 4.0 | |
| Presence of problems during pregnancy that did not contraindicate breastfeeding | |||||
| Yes | 33 | 19 | 39 | 22.4 | .427 |
| No | 141 | 81 | 135 | 77.6 | |
| Rooming in of mother and child during the hospital stay | |||||
| Yes | 165 | 94.8 | 156 | 89.7 | .071 |
| No | 9 | 5.2 | 18 | 10.3 | |
Cases: women that did not initiate breastfeeding; controls: women that initiated breastfeeding. Statistical significance: P-value obtained in the χ2 test. Statistical significance was established at a level of 5%, so comparisons were considered significant if P < .05. The Fisher exact test was also used.
BF, breastfeeding.
Table 3 summarises the opinions of participants regarding breastfeeding, their previous experience, the information that had been available to them and the timing of the decision whether to breastfeed. When it came to the perception of any previous experience breastfeeding, 41.4% of participants reporting having breastfed in the past, of who 70.1% had a favourable experience. Overall, breastfeeding was perceived favourably by 69.3% of participants and 64.4% of their partners. The table shows significantly different proportions between cases and controls as regards previous experience with breastfeeding and the timing of the decision whether to breastfeed. As regards breastfeeding education, 88.5% of participants reported having received information on breastfeeding, and 60.7% receiving information during the pregnancy. The most frequent source of the information was the midwife (73.6%), followed by relatives (33.0%). Paediatricians provided information on breastfeeding in 14.1% of cases, gynaecologists in 7.8% and family physicians in 4.6%. The decision whether or not to breastfeed was made before the pregnancy by 67.5% of participants (95% CI, 62.5%–72.6%).
Opinions and information about breastfeeding, previous experience with it and timing of decision whether to breastfeed.
| Characteristic | Cases (no BF initiation) (N = 174) | Controls (BF initiation) (N = 174) | P | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Previous breastfeeding | |||||
| Yes | 54 | 31.0 | 90 | 51.7 | <.001 |
| No | 120 | 69.0 | 84 | 48.3 | |
| General perception of breastfeeding of the participant | |||||
| Favourable | 121 | 69.5 | 120 | 69.0 | .908 |
| Unfavourable or indifferent | 53 | 30.5 | 54 | 31.0 | |
| General perception of breastfeeding of the partner | |||||
| Favourable | 105 | 60.3 | 119 | 68.4 | .117 |
| Unfavourable or indifferent | 69 | 39.7 | 55 | 31.6 | |
| Timing of decision whether or not to breastfeed | |||||
| Before gestation | 81 | 46.6 | 154 | 88.5 | <.001 |
| During gestation or at birth | 93 | 53.4 | 20 | 11.5 | |
| Participant received information about breastfeeding | |||||
| Yes | 157 | 90.2 | 151 | 86.8 | .313 |
| No | 17 | 9.8 | 23 | 13.2 | |
| Participant considered the information on breastfeeding she had received sufficient | |||||
| Yes | 129 | 74.1 | 114 | 65.5 | .080 |
| No/Not sure | 45 | 25.9 | 60 | 34.5 | |
Cases: women that did not initiate breastfeeding; controls: women that initiated breastfeeding. Statistical significance: P-value obtained in the χ2 test. Statistical significance was established at a level of 5%, so comparisons were considered significant if P < .05.
BF, breastfeeding.
As regards lifestyle habits, Table 4 shows that the proportion of participants with sedentary habits was higher in the group that did not breastfeed both before and during pregnancy, while the proportion of smokers was higher in this group only during pregnancy. This table also presents the characteristics of participants in the case and control groups in relation to other lifestyle habits and the adherence to the Mediterranean diet, overall and for each of the 14 items of the MEDAS-14. The mean score in the MEDAS-14 was 8.3 points before pregnancy and 8.9 points during pregnancy (on a scale from 0 to 14), with no differences between cases and controls. We also found no differences in the use of alcohol, physical inactivity or adherence to the Mediterranean diet.
Characteristics associated with lifestyle habits and distribution of adherence to each of the 14 items of the dietary questionnaire before and during pregnancy in cases and controls.
| Before gestation | During gestation | |||||
|---|---|---|---|---|---|---|
| Cases (no BF initiation) (N = 174) n (%) | Controls (BF initiation) (N = 174) n (%) | P | Cases (no BF initiation) (N = 174) n (%) | Controls (BF initiation) (N = 174) n (%) | P | |
| Participant lifestyle habits | ||||||
| Tobacco use | 38 (21.8) | 29 (16.7) | 0.221 | 28 (16.1) | 15 (8.6) | .034 |
| Any alcohol consumption | 77 (44.3) | 72 (41.4) | 0.588 | 7 (4.0) | 5 (2.9) | .557 |
| Physical inactivity (BPAAT) | 38 (21.8) | 43 (24.7) | 0.526 | 66 (37.9) | 57 (32.8) | .313 |
| Sedentary periods ≥2 h/day | 106 (60.9) | 77 (42.1) | 0.002 | 128 (73.6) | 102 (58.6) | .003 |
| Adherence to Mediterranean diet (MEDAS-14) | 0.900 | .507 | ||||
| High | 31 (17.8) | 29 (16.7) | 37 (21.3) | 44 (25.3) | ||
| Moderate | 112 (64.4) | 111 (63.8) | 110 (63.2) | 109 (62.6) | ||
| Low | 31 (17.8) | 34 (19.5) | 27 (15.5) | 21 (12.1) | ||
| MEDAS-14 questionnaire items | ||||||
| Olive oil as main source of added lipids | 171 (98.3) | 165 (94.8) | 0.078 | 169 (97.1) | 163 (93.7) | .125 |
| ≥2 tablespoons of olive oil/day | 171 (98.3) | 167 (96.0) | 0.199 | 170 (97.7) | 165 (94.8) | .158 |
| ≥2 servings of vegetables/day | 96 (55.2) | 90 (51.7) | 0.519 | 106 (60.9) | 97 (55.7) | .328 |
| ≥3 pieces of fruit/day | 72 (41.4) | 75 (51.0) | 0.745 | 86 (49.4) | 92 (52.9) | .520 |
| ≤1 serving of red meat and/or cured meat/day | 53 (30.5) | 47 (27.0) | 0.477 | 75 (43.1) | 76 (43.7) | .914 |
| ≤1 serving of butter and derivatives/day | 134 (77.0) | 132 (75.9) | 0.801 | 136 (78.2) | 137 (78.7) | .896 |
| ≤1 sugary drink/day | 77 (44.3) | 87 (50.0) | 0.283 | 109 (62.6) | 120 (69.0) | .214 |
| ≥ 3 glasses of wine/week | 13 (7.5) | 3 (1.7) | 0.010 | 1 (0.6) | 2 (1.1) | .562 |
| ≥3 servings of legumes/week | 77 (44.3) | 70 (40.2) | 0.447 | 83 (47.7) | 80 (46.0) | .747 |
| ≥3 servings of fish or shellfish/week | 68 (39.1) | 70 (40.2) | 0.827 | 70 (40.2) | 80 (46.0) | .279 |
| <3 industrial baked goods/week | 90 (51.7) | 101 (58.0) | 0.236 | 95 (54.6) | 107 (61.5) | .192 |
| ≥1 serving of nuts/week | 105 (60.3) | 134 (77.0) | 0.001 | 111 (63.8) | 135 (77.6) | .005 |
| Predominant consumption of white meat | 161 (92.5) | 149 (85.6) | 0.039 | 160 (92.0) | 152 (87.4) | .159 |
| ≥2 servings of stir-fried vegetables/week | 149 (85.6) | 154 (88.5) | 0.424 | 153 (87.9) | 152 (87.4) | .871 |
Cases: women that did not initiate breastfeeding; controls: women that initiated breastfeeding. Statistical significance was established at a level of 5%, so comparisons were considered significant if P < .05.
BF, breastfeeding.
Table 5 presents the variables found to be independently associated with the lack of breastfeeding initiation in mothers of a child aged less than 5 years in the logistic regression analysis, with the corresponding ORs and CIs.
Factors associated with the lack of breastfeeding initiation identified in the multivariate analysis (logistic regression).
| OR | 95% CI | P | |
|---|---|---|---|
| Lack of previous experience breastfeeding | 12.75 | 5.13−31.66 | <.001 |
| Decision made during pregnancy or at time of birth | 10.55 | 5.63−19.77 | <.001 |
| Being unmarried or without a stable partner | 3.42 | 1.56−7.51 | .002 |
| Sedentary periods ≥ 2 h/day during pregnancy | 1.77 | 1.01−3.09 | .046 |
CI, confidence interval; OR, odds ratio.
Although the benefits of breastfeeding for the child and mother are well known, more than 10% of mothers in Spain choose not to initiate breastfeeding for the child’s nutrition.6 In our study, we found that the factors associated independently with the lack of breastfeeding initiation were maternal sedentary lifestyle, single status, lack of previous experience breastfeeding and having made the decision regarding breastfeeding during the pregnancy. We also found that both the percentage of smokers and the frequency of maternal sedentary lifestyle during pregnancy were higher in the group of mothers who did not initiation breastfeeding, with no significant differences in other lifestyle habits between those who initiated breastfeeding and those who did not. However, the only factor that was independently associated with the decision not to breastfeed in the multivariate analysis was maternal physical inactivity during pregnancy.
As regards sociodemographic characteristics, consistent with previous studies,15–17 we found a lower frequency of breastfeeding in women who were not in a stable relationship. Our findings were also in agreement with previous evidence of an association of greater maternal age and breastfeeding initiation.16,18 We also found similar results to those described in the literature regarding maternal nationality, as the proportion of women from countries other than Spain was higher in the group that chose to breastfeed compared to the group that did not.19,20 This can be related to employment circumstances and sociocultural aspects. However, contrary to previous studies, we did not find an association between socioeconomic status and breastfeeding initiation.16
Women consider breastfeeding the optimal nutrition for their children,21 in agreement with the predominantly favourable perception of breastfeeding in the women that participated in our study and their partners in both the case and control groups. This could be related to the impact of promotion campaigns and the role of the sources of information on breastfeeding, as most interviewees reported having received information, most frequently from the midwife. However, our findings demonstrate that this widely held opinion was not necessarily reflected in the feeding modality chosen for their infants. A possible explanation is that personal decisions regarding breastfeeding are also dependent on other aspects, such as maternal choices, difficulties in breastfeeding initiation and maternal health problems.6
Although we found different proportions in the case and control groups of women that received prenatal care from a midwife and women that received prenatal care from an obstetrician, this difference did not remain significant when confounders were taken into account in the multivariate analysis. It is likely that, in both cases, the results of the crude analysis were due to the fact that only a minority of women were not followed up by these professionals (midwife and obstetrician).
Few studies have analysed the association of breastfeeding with maternal physical activity and nutrition lifestyle habits before and during pregnancy. Our study evinced that a sedentary lifestyle during pregnancy and making decisions regarding breastfeeding after conception were associated with not initiating breastfeeding. Similar results in relation to the timing of decision-making regarding breastfeeding have been reported in the past,22 probably reflecting the stronger influence of cultural, familial and personal beliefs predating gestation, while during pregnancy, the barriers to combining breastfeeding and usual activities become more apparent. Our study also evinced, consistent with the previous literature,23,24 the influence of past experience with breastfeeding on the decision to practice it again.
During pregnancy and breastfeeding, women care more for their health,23,25 which could extend to the health of their children, influencing attitudes in favour of healthier lifestyles for themselves and for their newborn infants. Thus, there is evidence of a positive impact of a healthy lifestyle on breastfeeding initiation and duration.16 In our study, we analysed lifestyles before and during pregnancy, and found differences between the 2 groups under study only in the use of tobacco and sedentary lifestyles, although remaining sedentary for periods lasting 2 or more hours each day during pregnancy was the only factor independently associated with the lack of breastfeeding initiation. The association between tobacco use and not breastfeeding has been observed before.8,18,26,27 There is also previous evidence of a greater probability of breastfeeding initiation in more physically active women,16 while our findings did not evince differences between the two groups in physical activity, although we did find an association between being physically inactive for long periods of time and not breastfeeding.
On the other hand, we did not find differences in the adherence to the Mediterranean diet, although we did find differences in the consumption of specific food groups, such as alcohol and white meat before pregnancy and nuts both before and during pregnancy. It is possible that the characteristics of the population under study and the type of questionnaire used influenced the results, as other studies that analysed the diet of pregnant women applied more extensive questionnaires that assessed the consumption of more food groups.28,29
One potential limitation of the study is the absence of randomization, as we recruited participants consecutively as they visited their respective primary care centres. However, we believe that the sample may be representative of the population of women with at least 1 child under 5 years, as most of the population in our area receives services through the national public health care system,30 and a majority makes visits to the primary care centre during the year.31 Furthermore, the data were collected retrospectively, from a few days to 4 years after childbirth, so we cannot exclude the possibility of recall bias, which is common in studies with this type of design. Another potential limitation is that we did not ask about the consumption of substances other than tobacco or alcohol. Also, possibly, another limitation is the questionnaire used to measure adherence to the Mediterranean diet, as this instrument assigns a positive score to the consumption of more than 3 glasses of wine a week. This is a controversial aspect, as the World Health Organization advises against the consumption of any alcohol, as no amount of alcohol is considered safe.32 In addition, we did not ask about the reasons that breastfeeding was not initiated, which could be considered a limitation of the study.
Interventions implemented to increase breastfeeding rates have often yielded unexpected results.33 The data collected in our study allowed us to identify a maternal sedentary lifestyle and making decisions regarding breastfeeding during pregnancy as modifiable factors associated with breastfeeding initiation. However, we did not find evidence of the potential impact of maternal healthy lifestyle habits on the decision to choose the best possible feeding modality for the child in the first months of life. We did identify factors associated with breastfeeding initiation that were not modifiable, such as marital status and previous experience with breastfeeding. Thus, further research may be needed on other potential modifiable predictors to target in future strategies to improve breastfeeding rates. On the other hand, studies are also required on the sources of information about breastfeeding, as our findings identified the midwife as the main source of information, while family physicians and paediatricians rarely provided information on the subject, despite being professionals in a particularly advantageous position to promote breastfeeding.34,35
In conclusion, our findings allowed us to identify a series of characteristics in pregnant women that increase the risk of not initiating breastfeeding, such as lack of previous experience breastfeeding, having made the decision whether to breastfeed during pregnancy, as opposed to before, and not being married or in a partnership. As regards lifestyle habits, a sedentary lifestyle was the only factor we found to be associated with lack of breastfeeding initiation, while dietary or other habits were not found to have an impact. The presence of these characteristics can be interpreted as a red flag in everyday clinical practice, allowing for more specific intervention (by the midwife, obstetrician, paediatrician or family physician) in the identified mother by devoting the necessary time and resources to explore her beliefs and concerns and recommend breastfeeding as an option to consider.
Conflicts of interestThe authors have no conflicts of interest to declare.