Eating disorders (EDs) develop more frequently in young females. Following the COVID-19 pandemic, there has been evidence of an increase in children and adolescents, with an earlier onset and a worse body weight and nutritional status. The aim of this study was to determine whether this trend has also been observed in our region over the past 6 years.
Material and methodsWe conducted a retrospective and descriptive cohort study in paediatric patients with a diagnosis of ED, referred during the 3 years preceding and following the declaration of the state of alarm due to the pandemic. We analysed and compared clinical, anthropometric and laboratory variables and bioelectrical impedance and bone density data.
ResultsOf the 129 patients in the sample, 28 were referred before the lockdown period and 101 after. When we compared these groups, we found a longer time elapsed from onset to the initial assessment (mean delay, 11.87 [SD, 6.75] vs. 6.64 [SD, 4.36] months), a greater hospitalization rate (14.1% vs. 10.1%), and lower vitamin D values (mean level, 28.19 [SD, 9.95] vs. 34.39 [SD, 11.87] ng/mL) in the post-lockdown group. We also found a greater frequency of self-harm suicide attempts in these patients.
ConclusionsThis study confirms the increasing trend in EDs in children and adolescents in our area. Moreover, we found differences in the clinical characteristics and time elapsed to diagnosis compared to the patients referred to the hospital before the pandemic.
Los trastornos de la conducta alimentaria (TCA) se presentan con mayor frecuencia en personas jóvenes de sexo femenino. Tras la pandemia por COVID-19, se ha descrito su incremento en niños y adolescentes, con presentación a edades más tempranas y peor estado ponderal y nutricional. Este estudio pretende constatar si esa tendencia se cumple también en nuestro medio.
Material y métodosSe realizó un estudio de cohortes descriptivo, retrospectivo en el que se incluye a los pacientes pediátricos con diagnóstico de TCA, remitidos durante los tres años previos y posteriores a la declaración del estado de alerta por la pandemia. Se analizaron y compararon parámetros clínicos, antropométricos, analíticos, bioimpedancia eléctrica y densitometría ósea.
ResultadosDe los 129 pacientes de la muestra, 28 se derivaron en periodo pre-confinamiento y 101 tras el mismo. En comparación, el segundo grupo presentó mayor tiempo de evolución hasta su primera valoración (11,87 ± 6,75 frente a 6,64 ± 4,36 meses), más hospitalizaciones (14,1% frente a 10,1%), y una reducción de los valores de vitamina D (28,19 ± 9,95 frente a 34,39 ± 11,87 ng/mL). Asimismo, estos pacientes asociaban con más frecuencia autolesiones e intentos de suicidio.
ConclusionesSe comprobó la tendencia creciente de los TCA en niños y adolescentes en nuestro medio. Además, se observaron diferencias en algunas de sus características clínicas, en su gravedad, y en el tiempo de evolución hasta el diagnóstico, en comparación con los pacientes remitidos antes de la pandemia.
Feeding or eating disorders (FEDs) are a group of diseases of multifactorial aetiology and a biopsychosocial nature. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) classifies them into various groups based on their clinical features, among which the most salient in older children and adolescents are those characterised by an underlying distorted body image and fear of weight gain: anorexia nervosa (AN), bulimia nervosa (BN), binge-eating disorder (BED), other specified feeding or eating disorders (OSFEDs, which include atypical AN, BN and BED) and unspecified feeding or eating disorders (UFEDs).1,2
These FED subtypes are more prevalent in female adolescents and female young adults and at ages 13–15 years. The estimated prevalence in Western countries is of 2.4% in the general population. A systematic review found that the most prevalent disorder was AN (prevalence ranging from 1.7% to 3.6% in females and 0.1% in males),3 although UFEDs and OSFEDs appeared to be on a progressively increasing trend.4,5
These diseases are associated with high morbidity and mortality and frequently co-occur with other psychiatric disorders, such as anxiety, depression, personality disorders or obsessive-compulsive disorder; suicide is one of the main causes of death in affected patients.1,6,7
The current literature broaches the potential role of biological, cultural and psychosocial factors in the aetiology and pathogenesis of FEDs. Among the latter, the potential risk factors, in addition to body dissatisfaction or the idealization of certain beauty standards could include stressful experiences or a history of trauma.8
In fact, the incidence of both FEDs and other psychiatric disorders has been increasing worldwide in the past few decades.9 Recently, in the context of the coronavirus disease 2019 (COVID-19) pandemic, several studies have found evidence that the risk of developing some of these disorders may have increased, especially in the most vulnerable subsets of the population, like children and youth.10–13
The measures taken to contain the spread of SARS-CoV-2 may have contributed to the deterioration of mental health in the population10–14: home confinement and social distancing have been associated with increased levels of stress and worry, among other factors. These facts may have precluded adequate coping, facilitating the development of anxiety or depression symptoms.10–15 Adolescents, in particular, could be more vulnerable to the development of psychological disturbances under these conditions.11,12,16 Specifically, the discontinuation of in-person learning and the decrease in athletic activities, combined with the increased use of social media,11,15,17–19 promoted the dissemination among adolescents of fake news and access to content focused on physical appearance and personal image.15,20 All of this could have exacerbated concerns about body image and therefore increased the risk of a FED.1,9,15,17,20–23
Supporting this hypothesis, several countries have reported an increase in the newly diagnosed cases of FEDs since 2020, with a predominance of AN in both the adult and the paediatric population.15,21–25
Some studies have also found evidence suggestive of possible shifts in their presentation: younger age of onset, greater symptom severity and an increase in the proportion of cases classified as atypical anorexia.22,24 An increase in the number of referrals and hospitalizations due to psychiatric disorders overall and FEDs in particular has also been reported in Spain.18,26,27
In this context, the aim of our study was to determine whether this trend was also present in our area by analysing the patients assessed in our hospital, which is the provincial referral centre for FEDs in children and adolescents, in the 3 years preceding and the 3 years following the declaration of the state of alert due to the COVID-19 pandemic.
Material and methodsObjectivesThe primary objective was to assess the impact of the COVID-19 pandemic in the frequency of paediatric cases of FEDs newly diagnosed in our province in the past 6 years based on the data on patients evaluated by the Child and Adolescent Nutrition Unit, which is the provincial referral unt for FEDs. The study focused on 5 types of FEDs: AN, BN, BED, OSFEDs and UFEDs.
The secondary objective was to compare the characteristics of the patients in the period before and the period after the lockdown in terms of age of onset, clinical condition, anthropometric measurements and nutritional status.
Study designWe conducted a retrospective descriptive cohort study.
The sample included patients referred to the outpatient clinics or hospitalised in the paediatric inpatient ward who underwent an initial assessment by the paediatric nutrition team, aged less than 17 years, either male or female, given a diagnosis of FED (AN, BN, BED, OSFED or UFED subtype) based on the DSM-5 criteria. The diagnosis was made by a psychiatrist specialised in FEDs.
We included every patient who met the inclusion criteria in the past 6 years (March 15, 2017-March 14, 2023), dividing the total study period in two periods separated by the date of the declaration of the state of alert due to the COVID-19 pandemic and the imposition of the lockdown/home confinement measure in Spain: before March 14, 2020 (prepandemic period) and after (post-pandemic/post-lockdown period). Part of this cohort has been described previously in terms of its characteristics and body composition.
We collected epidemiological data (age, sex, type of FED), clinical data (time elapsed from onset, percentage of body weight lost, symptoms associated with the FED, menarche, secondary amenorrhoea or significant delay in menses, psychiatric comorbidities, pharmacological treatment, self-injury or suicidal attempts, history of bullying or social isolation, history of overweight or obesity), laboratory data (complete blood count, iron profile, lipid profile, blood chemistry panel, 25-hydroxyvitamin D [25-OH-D], B12 and folic acid, albumin, thyroid hormones, estradiol, follicle-stimulating hormone [FSH], luteinizing hormone [LH], leptin [measurement of leptin levels started to be ordered from 2021]), anthropometric data (weight, height, body mass index [BMI], arm circumference and triceps skinfold; recording the raw value and the z score using the Hernández et al. growth tables28 of 1988), bone scintigraphy data (ordered in patients with severe undernutrition, delayed puberty or secondary amenorrhoea lasting more than 6 months: lumbar and overall z score) and bioelectrical impedance analysis (BIA) data (since the necessary equipment [Akern BIA 101 Anniversary system, Pontassieve, Florence, Italy] was not available before, these measurements started to be taken from September 2020).
Blood samples for testing were collected after the initial assessment in the nutrition clinic, within the following month, independently of the phase of the menstrual cycle or the time of year. We defined deficiency in blood chemistry results as a value below the normal range for age based on the reference ranges applied in the laboratory of our hospital. We defined secondary amenorrhoea as absence of menses for three consecutive months in patients with regular periods or for at least 6 months in patients with irregular periods. Overweight was defined as a BMI z score greater than 1 and obesity as a BMI z score greater than 2.
Statistical analysisWe conducted a descriptive analysis of the data, calculating the mean, standard deviation (SD), first, second (median) and third quartiles to describe continuous variables and absolute frequencies and percentages for categorical variables. In the bivariate analysis, we compared continuous variables in independent groups with the Student t test. The normality of the distribution was evaluated by means of the Kolmogorov-Smirnov test, and the null could not be rejected for any variable save the time elapsed from onset, the weight z score, the levels of estradiol, folic acid and LH, for which a normal distribution was assumed based on the central limit theorem. We compared categorical variables using the χ2 test or the Fisher exact test as applicable. We also calculated the Pearson correlation coefficient (r) to assess the correlation between two continuous variables.
For laboratory results with values below the threshold of detection of the used technique, we substituted them by half of the minimum detectable value.
The statistical analysis was performed with the statistical package SPSS version 21 (IBM SPSS Statistics), considering P values significant when they were less than 0.05 and marginally significant when they were less than 0.1.
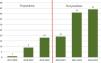
ResultsThe sample included 129 patients (28 in the prepandemic period and 101 in the post-lockdown period). They were grouped into 6 periods ranging from March 15 of one year and March 14 of the following year, separated by the date that the home confinement lockdown period started (Fig. 1). There was an increasing trend in the incidence of FEDs, and the case distribution was 21.7% in the prepandemic period and the remaining 78.3% in the post-lockdown period (P < .001).
The mean age was 14.17 years (SD, 1.3; range, 9.6–168), and there was a predominance of the female sex (91.5%).
The most prevalent diagnosis was AN (81.4%). Furthermore, 16.3% of cases were diagnosed as UFED and 2.3% as BN. None of the patients were referred for BED. Of the total patients with a FED, 13.4% required hospital admission at the time of diagnosis.
The mean time elapsed from onset of symptoms to the evaluation was 10.7 months (SD, 6.6; 1–36 months). The most frequent clinical manifestation was intake restriction (98.4% of patients) followed by excessive compensatory exercise (58.9%). In addition, 29.5% of patients engaged in purging behaviours and 27.9% in bingeing behaviours.
In the initial assessment, the anthropometric characteristics of the patients were as follows: weight z, −0.91 (SD, 5.41); height z, 0.30 (SD, 0.84); BMI, 1.92 kg/m2 (SD, 0.94; BMI z, −0.75;); arm circumference z, −0.32 (SD, 1.53); triceps skinfold z, −0.64 (SD, 0.75).
Taking into account the maximum weight recorded before symptom onset, the mean weight loss at the time of diagnosis was of 4.12%, although there was substantial variation (SD, 8.87; 0 %–40 %). There was a previous history of overweight or obesity in 17.80% of the patients.
Among the female patients, 88.8% had undergone menarche, and 56% of this subset had secondary amenorrhoea or significantly delayed menstruation compared to previous cycles with a mean delay of 5 months (SD, 3.58; range, 1–18).
A bone scintigraphy was performed in 61 patients, with a mean lumbar z score of −0.23 (SD, 1.02; range, −2.3 to −2) and a mean overall z score of 0.25 (SD, 0.83; range, −2.1 to −2.1). The scan found decreased bone mineral density in 1.6% (z < −2).
When it came to blood tests, there were haematological abnormalities in 14.2% of patients (anaemia, microcytosis or macrocytosis, hypochromia). Of all patients, 34.5% had ferropenia, 27.4% dyslipidaemia and 39.8% deficient levels of 25-hydroxyvitamin D. The mean leptin level, measured in 52 patients (all in the post-pandemic group) was 8.83 ng/mL (SD, 9.72; range, 0.05–38.20).
A BIA was performed in 109 patients, and Table 1 presents the measures of central tendency for the corresponding results.
Bioelectrical impedance analysis results (n = 109 patients).
| FFM (kg) | TBW (L) | ECW (L) | BCM (kg) | FM (kg) | PhA (°) | %FM (%) | %FF (%) | %TBW (%) | BCMI | |
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | 36.34 | 29.35 | 12.60 | 18.23 | 10.06 | 5.41 | 21.59 | 78.96 | 64.07 | 6.98 |
| SD | 6.96 | 4.76 | 2.72 | 4.81 | 5.20 | 0.97 | 10.07 | 7.72 | 9.12 | 1.67 |
| Minimum | 23 | 14 | 8.2 | 4.9 | 0 | 3.2 | −0.1 | 56.4 | 9.9 | −1 |
| Maximum | 61.4 | 46.1 | 21.9 | 39.3 | 35.9 | 11.2 | 88.8 | 100.1 | 87.5 | 13.5 |
| Percentiles | ||||||||||
| 25th | 31.4 | 26.3 | 10.6 | 15 | 6.5 | 4.7 | 15.45 | 73.25 | 59.4 | 6 |
| 50th | 35.4 | 28.6 | 12 | 17.9 | 9.3 | 5.4 | 21.3 | 78.7 | 63.5 | 6.69 |
| 75th | 40.35 | 31.6 | 14.1 | 20.65 | 13.1 | 5.85 | 36.75 | 84.55 | 69.3 | 7.85 |
BCM, body cell mass; BCMI, body cell mass index; ECW, extracellular water; FFM, fat-free mass; FM, fat mass; PhA, phase angle; SD, standard deviation; TBW, total body water.
In the total sample, 36.7% had psychiatric comorbidities, most frequently depression, mixed anxiety-depression, autism spectrum disorder, adjustment disorder, disruptive behaviour and conduct disorders or problems with peer relationships and personality disorders. In addition, 12.5% reported self-injury or suicidal attempts and 41.8% bullying or social isolation. In addition, 42.5% were in treatment with antidepressants.
When we compared the characteristics of the prepandemic vs. the post-pandemic groups (Table 2), we found a significant difference in the time elapsed from onset to initial assessment, with greater delay in the post-pandemic period (mean delay, 6.64 [prepandemic] vs. 11.87 [post-pandemic] months; mean difference [MD], 5.2; 95% confidence interval [CI], 2.6–7.9; P < .001). The mean vitamin D level was lower in the post-pandemic group (MD, −6.2; 95% CI, −11.5 to −0.89; P = .023). We did not find significant differences in age, the percentage of weight loss relative to the maximum recorded weight or any other clinical or laboratory variable between the groups.
Comparison of clinical, anthropometric, bone density and laboratory variables in the pre- and post-pandemic groups.
| Prepandemic | Post-pandemic | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean (SD) | Median | IQR (Q1;Q3) | n | Mean (SD) | Median | IQR (Q1;Q3) | P | |
| Clinical variables | |||||||||
| Age (years) | 28 | 13.83 (1.26) | 13.89 | 13.04; 14.92 | 101 | 14.27 (1.3) | 14.33 | 13.63; 15.17 | .112 |
| Time to initial assessment (months) | 28 | 6.64 (4.36) | 5 | 4; 9.75 | 99 | 11.87 (6.75) | 10 | 7; 14 | < .001 |
| Anthropometric measurements | |||||||||
| Weight (z) | 28 | −0.44 (0.71) | −0.48 | −0.79; 0.03 | 101 | −1.04 (6.1) | −0.61 | −1; −0.07 | .601 |
| Height (z) | 28 | 0.4 (0.7) | 0.07 | −0.05; 1.2 | 101 | 0.28 (0.87) | 0.38 | −0.28; 0.9 | .474 |
| BMI (kg/m2) | 28 | 17.74 (2.81) | 17.1 | 15.69; 19.96 | 101 | 17.97 (3.41) | 17.31 | 15.72; 19.59 | .738 |
| BMI (z) | 28 | −0.76 (0.83) | −0.91 | −1.26; −0.21 | 101 | −0.75 (0.97) | −0.91 | −1.44; −0.29 | .955 |
| Maximum weight loss (%) | 25 | 19.21 (9.70) | 19 | 13.90; 25 | 96 | 18.20 (11.05) | 18 | 11.5; 25.9 | .66 |
| Arm circumference (z) | 2 | −4.25 (2.88) | −4.25 | −− | 78 | −0.22 (1.38) | −0.11 | 0; 0.4 | < .001 |
| Triceps skinfold z score | 2 | −0.12 (2.43) | −0.12 | −− | 75 | −0.65 (0.7) | −0.72 | 0; −0.26 | .32 |
| Bone density (scintigraphy) | |||||||||
| Lumbar (z) | 9 | −0.17 (1.12) | 0 | −1.15; 0.9 | 52 | −0.24 (1.02) | −0.1 | −1; 0.5 | .852 |
| Overall (z) | 9 | 0.42 (0.65) | 0.3 | 0; 1 | 53 | 0.22 (0.86) | 0.4 | −0.3; 0.8 | .511 |
| Laboratory tests | |||||||||
| 25-OH-D (ng/mL) | 19 | 34.39 (11.87) | 34.4 | 27.6; 38.3 | 73 | 28.19 (9.95) | 25.8 | 22.05; 33.05 | .023 |
| Vitamin B12 (pg/dL) | 19 | 603.77 (222.36) | 561 | 402; 763 | 75 | 541.24 (190.19) | 513 | 407; 635 | .219 |
| Folic acid (ng/mL) | 21 | 6.29 (3.38) | 6 | 3.35; 8.5 | 73 | 6.46 (4.51) | 5 | 3.4; 8 | .837 |
| Basal FSH (mIU/mL) | 15 | 3.99 (3.03) | 3.95 | 0.95; 7.14 | 59 | 5.09 (3.18) | 5.36 | 2.08; 7.14 | .236 |
| Basal LH (mIU/mL) | 15 | 1.86 (2.4) | 0.63 | 0.1; 2.48 | 64 | 4.89 (5.91) | 3.065 | 0.33; 7.17 | .056 |
| Estradiol (pg/mL) | 5 | 108.82 (188.24) | 36.7 | 7.5; 246.2 | 56 | 42.26 (45.27) | 26.05 | 10; 55.17 | .474 |
BMI, body mass index; FSH, follicle-stimulating hormone; LH, luteinizing hormone; 25-OH-D, 25-hydroxyvitamin D.
The time elapsed from onset was negatively correlated to weight loss (r = −0.24; P = .008) and ferritin levels (r = −0.26; P = .008).
In female patients with secondary amenorrhoea, the mean time elapsed from onset to diagnosis was shorter (9.64 vs. 12.59 months; P = .026), the mean age at diagnosis younger (14.39 vs. 13.76 years; P = .009) and leptin values lower (7.41 ng/mL vs. 12.85 ng/mL; P = .064), without differences in the bone density z scores or any other variables.
DiscussionDuring the COVID-19 pandemic, the incidence of FEDs increased markedly worldwide.24,25,29–32 This has also been observed in Spain, with a particularly marked increase after the lockdown period.26
Our study demonstrated that the same trend occurred in the child and adolescent population of our province. Specifically, the number of referred patients doubled immediately after the end of the lockdown, after which the increasing trend has remained steady.
As regards the type of FEDs diagnosed in the patients, the most frequent type was AN, followed by BN and UFED. However, none of the patients in the sample was referred due to BED. Paradoxically, an increase in the frequency of bingeing episodes and the incidence of BED has been reported after the pandemic, in part due to the breakdown of routines and the increased stress and decreased physical activity experienced during this period.33,34 At present, the prevalence of BED is greater than the prevalence of BN, based on evidence such as the World Health Organization mental health surveys.35 Therefore, we surmise that BED may be underdiagnosed in our area, and that awareness of this disease needs to be raised to allow its detection and appropriate treatment.
At the time of diagnosis of the eating disorder, 17 patients in the sample had to be admitted to hospital. Of this total, 14 were admitted after the lockdown, amounting to 14.1% of the patients in the post-pandemic period. The increased severity of disease and rate of hospitalization of patients with FEDs after the pandemic (especially AN) has also been reported in other countries.13,15,24
We did not find significant differences in the mean age of the patients in the two periods under study, in contrast to the findings of other authors.27,36 However, the mean delay from onset to diagnosis did increase significantly, nearly doubling after the lockdown period. One plausible explanation is the reduction in the provision of in-person health care services during the lockdown, providing most services through the phone, a medium through which the physical and psychosocial assessment of the patient is limited, among other possible reasons. In addition, the observed delay in referral, combined with the recorded age at the time of the initial assessment in the nutrition department, suggests that the age at onset of FEDs in the post-pandemic group could be actually lower. There is no question that this delay in the referral to speciality care and, therefore, in diagnosis and treatment initiation, worsens the prognosis of FEDs and hinders recovery.37 Interventions to raise awareness and educate the general population, specific training of health care professionals and streamlined pathways for referral to specialised care are among the possible strategies that could improve this time intervals.
In addition, we found that the greater the weight loss of patients, the shorter the time elapsed to referral, regardless of when they developed the FED (before or during the pandemic). At the same time, we found a shorter time to referral in female patients who already had secondary amenorrhoea. This association suggests that more severe undernutrition and the presence of amenorrhoea are more alarming to patients, their families and health care providers, leading to faster activation of the care pathway. If this were the case, it would be important to keep in mind that diagnosis and treatment could be delayed in patients with smaller weight losses. Thus, due to this delay, such patients could present with disease at a more severe stage or once it has become chronic.
When it came to psychiatric comorbidities, the frequency was similar in patients referred before and during the pandemic. However, in the post-pandemic group, there was a higher incidence of self-injury and suicide attempts. This increase in self-harm and suicidal behaviour has already been described in previous studies, and the Asociación Española de Pediatría (Spanish Association of Pediatrics) has even issued a warning about it.38–40
The laboratory values did not differ significantly between the groups, except for vitamin D levels, which were lower in the post-pandemic patients. A study published in 2022 reported a high frequency of vitamin D deficiency in the population aged less than 18 years and the authors hypothesised that it could be associated with the home confinement period and the decrease in outdoor activities.41 However, we ought to underscore that we were not able to control the time of year that vitamin D levels were measured in our patients, as the sample was collected at the time of the initial evaluation by the nutrition care team, so we were not able to assess the potential role of the level of solar radiation in these results.
LimitationsDuring the period under study, our hospital was the referral centre for FEDs in our province, so we assumed that most paediatric patients with FEDs would be included in the sample, thus providing a record of substantial scope and value for the estimation of the incidence of FEDs in this age group.
However, it is possible that patients with less severe disorders or at the age threshold between paediatric and adult care were not referred to speciality care or referred to the adult care services, resulting in missing data. On the other hand, since BIA was not available in the prepandemic period, we were not able to compare BIA results in the two groups.
Conclusion- •
We found a progressive increase in the incidence of FEDs in children and adolescents in our population in the 3 years following the lockdown due to the COVID-19 pandemic compared to the 3 previous years.
- •
The diagnosis of FEDs was delayed after the lockdown, with a longer time elapsed from the onset of symptoms to the initial assessment in the paediatric nutrition clinic.
- •
Patients with greater weight losses and female patients with amenorrhoea were referred within a shorter time frame, independently of when the onset of the FED occurred.
- •
In the group of patients diagnosed after the pandemic, there was a higher frequency of self-injury and of suicidal attempt.
- •
The frequency of hospital admission at diagnosis was higher in patients referred during the pandemic, which is suggestive of a greater severity of FED symptoms during this period.
- •
Vitamin D levels were significantly lower in the post-pandemic group, which may reflect a decreased exposure to sunlight after the imposition of the lockdown.
This research did not receive any external funding.
Ethical considerationsThe study was conducted in adherence to current ethical principles, laws and regulations in Europe and Spain. It was evaluated and approved by the Ethics Committee of Research with Medicines of our hospital.
Conflicts of interestMercedes Murray Hurtado and Álvaro Martín Rivada received financial support in the past 5 years to fund travel, lodging and registration fees for attendance to courses and congresses, as well as fees as instructors, from Nestlé Health Science, Abbott, Nutricia, Fresenius Kabi, Mead & Johnson and Casen Recordati; however, these authors deny having any conflicts of interest that could interfere with the results of the present study. Yolanda Ramallo Quintero and Silvia Pestano García have no conflicts of interest to disclose.
We thank the Official Board of Physicians of Tenerife for their guidance on the methodology and statistical analysis of this study.