Parents often ask paediatricians for advice about the best way to care for their children. There are discrepancies in the literature on this subject. The objective of this study is to evaluate the influence of attending kindergartens at the risk of acute infections and the use of health care resources in children less than 24 months.
Population and methodsA prospective longitudinal study was conducted on two cohorts of children aged 0–24 months (born between 1 January and 30 September 2010), who were grouped according to whether they attended kindergarten or not, and were usually seen in 33 paediatric clinics of the Principality of Asturias Public Health Service.
Results and conclusionsA total of 975 children were studied, of whom 43.7% attended a kindergarten at 24 months. Attending kindergarten increases the risk of pneumonia by 131%, recurrent wheezing by 69%, bronchitis by 57%, and otitis media by 64%. Early exposure to kindergarten increases the risk of pneumonia from 2.31 to 2.81, and the mean emergency room visits from 1 to 2.3.
The mean antibiotic cycle is 1.7 in children who do not go to kindergarten, 3.4 if started within the first 6 months, and 2 if they start at 18 months.
Care attendance is a factor of risk of infectious diseases increases if they attend at an early age.
Los padres con frecuencia solicitan a los pediatras consejo acerca del mejor sistema para el cuidado de sus hijos. En la literatura existen discrepancias al respecto. El objetivo de este estudio es evaluar la influencia de la asistencia a la guardería sobre el riesgo de infecciones agudas y la utilización de recursos sanitarios en los niños menores de 24 meses.
Población y métodosEstudio longitudinal prospectivo de 2 cohortes de niños de 0–24 meses que se diferencian por la asistencia o no a la guardería, nacidos entre el 1 de enero y el 30 de septiembre de 2010 y que acuden habitualmente a las consultas de 33 pediatras del Servicio Público de Salud del Principado de Asturias.
Resultados y conclusionesSe estudiaron 975 niños. A los 24 meses acuden a la guardería el 43,7%. Asistir a guardería incrementa el riesgo de padecer neumonía en un 131%, el de sibilancias recurrentes en un 69%, el de bronquitis un 57% y el de otitis media en un 64%. La exposición temprana a la guardería incrementa el riesgo de neumonías de 2,31 a 2,81 y la media de visitas a urgencias desde 1 a 2,3.
La media de ciclos de antibióticos es de 1,7 para los que no van a la guardería, de 3,4 si la inician en los 6 primeros meses y de 2 si comienzan a partir de los 18 meses.
La asistencia a guarderías es un factor de riesgo de padecer enfermedades infecciosas que aumenta si asisten desde edades tempranas.
Women and mothers have traditionally adopted the main role in the rearing of their children. At present, in our country, childbirth gives rise to new circumstances in which most citizens require the help of specialised services to take care of their young.1 The maternity leave period in Spain lasts 16 weeks,2 while it lasts 68 weeks in Sweden.3 The law allows working mothers to devote 1h a day to breastfeeding for 9 months. Thus, child care centres become a social need and demand. According to population surveys, in 2010, 25.01% of women employed out of the home in Spain reported engaging specialised services for the care of their children.4
Child care attendance does have an influence on children's health. A literature review published in 20075 concluded that child care attendance was associated with a significant increase in acute infectious disease in childhood, which also has an impact on society and the immediate household environment.6 Furthermore, it has economic consequences through increased health care costs and the cost associated with parental absences from work.7
In recent years, there has been social debate about the best way to care for children during early childhood. Some studies have been published in support of the psychosocial benefits of attending child care centres, although these benefits have not been proven in populations that are not at psychosocial risk.8 In this context, families often ask the paediatrician about the best way to care for their children. Learning the actual facts will better guide decision-making on this subject while taking into account the circumstances of the household and the health status of each child.
Objectives- •
To assess the influence of child care attendance on the risk of acute infection, use of pharmacological agents and use of health resources in children younger than 24 months. To establish the influence of other factors.
- •
To assess whether the “child care exposure time” factor increases the incidence of infectious diseases and the use of pharmacological agents.
- •
To learn the reasons for using child care from participant responses.
We conducted a prospective longitudinal study with two cohorts of children 0–24 months of age that differed in that they attended or did not attend child care (exposure factor); the study was adapted for Asturias from the one designed by the working group of the Asociación Española de Pediatría de Atención Primaria (Spanish Association of Primary Care Paediatrics).9
Inclusion criteriaChildren born between January 1 and September 30, 2010, seen regularly at primary care (PC) paediatric clinics of the Servicio Público de Salud del Principado de Asturias (Public Health Service of the Principality of Asturias [SESPA]), and whose families agreed to participate in the study after being fully informed.
Exclusion criteriaChildren with severe immunodeficiencies or respiratory diseases, heart disease requiring surgery, and children that were not seen regularly at the PC paediatric clinics.
ParticipantsThe study engaged the participation of 35 paediatricians and 20 nurses from the 8 health areas of the SESPA that recruited 1139 children.
Study variablesIndependent variable: child care attendance, yes or no (dichotomous variable), which defined the two cohorts. We documented the age the child started attending in months, and the reasons for attendance.
Descriptive variablesPersonal characteristics: inclusion code, date of birth, sex, gestational age, birth weight, neonatal morbidity, breastfeeding, vaccines from the official immunisation schedule of Asturias and optional vaccines (pneumococcal, rotavirus and varicella vaccines).
Household characteristics: number of siblings; parental characteristics: age, educational level, employed yes/no, smoking, allergies, asthma.
Dependent variablesNumber and type of acute infections leading to health visits (to PC paediatricians or emergency services): bacteraemia, bronchiolitis, acute bronchitis, conjunctivitis, exanthematous viral diseases, pharyngitis, pharyngotonsillitis, acute gastroenteritis, influenza, laryngitis, meningitis, pneumonia, acute otitis media, common cold, sepsis, recurrent wheezing episodes, all of them previously defined according to the Nelson Textbook of Pediatrics.10
Used medications: antibiotics, bronchodilators, inhaled and oral corticosteroids and montelukast.
Visits to emergency and paediatrics services: we excluded visits corresponding to the checkups of the well-child programme.
Data collectionWe collected the data from the electronic medical records and from interviews with the adults that accompanied children to scheduled check-up visits at ages 6, 12, 18 and 24 months, which consisted of personal interviews and the collection of data in questionnaires previously designed for this purpose. Data for the descriptive variables were collected at the first visit and data for the outcome variables at 6, 12, 18 and 24 months, and they were recorded in the forms filled out in each visit. The informed consent form (Appendix 1) given to the parents included an explicit statement on the adherence and compliance with legislation and with ethical principles.
Statistical analysisWe performed a descriptive analysis of the data collected for the different variables. To assess whether the age at first enrolment in child care affected the risk of having infectious diseases, we also analysed the sample by age intervals: less than 6 months, 6–11 months, 12–17 months and 18–24 months. To learn whether the “child care attendance” variable influenced the use of health services, we analysed this use by age (using the same age intervals) and the difference in the number of health care visits before and after enrolment in child care.
We used Pearson's chi square test for comparisons of two qualitative variables, and calculated effect measures such as the relative risk, which we present with their 95% confidence intervals. We calculated adjusted risks by means of binary multiple logistic regression models for sex, gestational age, birth weight, neonatal morbidity, breastfeeding, vaccinations, presence or lack of siblings, and parental variables including age, educational level, allergies, asthma and smoking. We used Student's or Welch's t tests for comparisons of two means, and the Kruskal–Wallis test to compare more than two. We tested for normality and equality of variance using the Shapiro–Wilk and the Ansari-Bradley tests, respectively. We set the level of statistical significance at P<.05.
We performed the statistical analysis with the R® software (R Development Core Team, 2012), version 2.15.
ResultsWe collected the data for 1139 children at age 6 months, 1092 at 12 months, and 975 at 24 months. Thus, 14.3% of cases were lost to followup due to three paediatricians changing jobs (7.9%) and participating children moving to new addresses (7.4%).
Individual and family dataTable 1 shows the individual and family characteristics of all the children in the sample and of children in each of the cohorts (attending/not attending child care), with the corresponding percentages and statistical significance.
Comparison (in percentages) of all the variables analysed in the two cohorts (attending and not attending child care) and statistical significance of the comparisons.
| % total | % in child care | % not in child care | Significance | |
|---|---|---|---|---|
| Sex | ||||
| Male | 50.74 | 53.14 | 48.88 | .22 |
| Female | 49.26 | 46.86 | 51.12 | |
| Gestational age | ||||
| <37wks | 9.70 | 11.22 | 8.51 | .35 |
| 37–40wks | 71.80 | 70.00 | 73.16 | |
| >40wks | 18.50 | 18.78 | 18.34 | |
| Birth weight | ||||
| <2kg | 2.20 | 1.47 | 2.86 | .55 |
| 2–2.5kg | 6.30 | 6.60 | 6.11 | |
| 2.5–4kg | 87.50 | 88.02 | 87.02 | |
| >4kg | 4.00 | 3.91 | 4.01 | |
| Neonatal morbidity | ||||
| Yes | 14.60 | 14.46 | 14.71 | .99 |
| Breastfeeding | ||||
| No | 27.12 | 27.99 | 26.46 | .88 |
| Less than 6 months | 39.86 | 40.22 | 39.58 | |
| 6–12 months | 22.05 | 22.55 | 21.67 | |
| More than 12 months | 10.97 | 9.24 | 12.29 | |
| Vaccinated against pneumococcus | ||||
| Yes | 84.31 | 89.20 | 80.33 | <.01 |
| Vaccinated against rotavirus | ||||
| Yes | 22.60 | 27.70 | 18.03 | <.01 |
| Vaccinated against varicella | ||||
| Yes | 25.50 | 27.00 | 24.41 | .39 |
| Father's age | ||||
| <20 years | 0.40 | 0.00 | 0.75 | .15 |
| 21–34 years | 43.30 | 41.77 | 44.53 | |
| 35–40 years | 39.20 | 42.01 | 36.98 | |
| >40 years | 17.10 | 16.22 | 17.74 | |
| Father's educational level | ||||
| Primary school | 27.10 | 19.41 | 33.08 | <.01 |
| Secondary school | 39.20 | 41.03 | 37.83 | |
| University | 33.70 | 39.56 | 29.09 | |
| Father currently employed | ||||
| Yes | 93.70 | 94.06 | 93.50 | .83 |
| Father with asthma | ||||
| Yes | 11.18 | 12.14 | 10.45 | .49 |
| Father with allergies | ||||
| Yes | 20.68 | 20.39 | 20.90 | .67 |
| Father that smokes | ||||
| Yes | 33.50 | 32.52 | 34.33 | .61 |
| Mother's age | ||||
| <20 years | 1.17 | 0.24 | 1.88 | .12 |
| 21–34 years | 58.98 | 59.90 | 58.27 | |
| 35–40 years | 34.43 | 34.96 | 34.02 | |
| >40 years | 5.42 | 4.89 | 5.83 | |
| Mother's educational level | ||||
| Primary school | 17.33 | 11.79 | 21.59 | <.01 |
| Secondary school | 40.64 | 38.33 | 42.42 | |
| University | 42.03 | 49.88 | 35.98 | |
| Mother currently employed | ||||
| Yes | 72.00 | 80.35 | 65.63 | <.01 |
| Mother with asthma | ||||
| Yes | 11.28 | 13.59 | 9.50 | .08 |
| Mother with allergies | ||||
| Yes | 23.60 | 25.24 | 22.35 | .33 |
| Mother that smokes | ||||
| Yes | 21.40 | 21.36 | 21.42 | .99 |
| Siblings | ||||
| No | 59.73 | 63.86 | 65.02 | .28 |
| One | 33.65 | 30.12 | 26.82 | |
| Two or more | 6.62 | 6.02 | 8.15 | |
By age 2 years, 43.7% of the children in the study attended child care. Fig. 1 shows the number of children first enrolled in child care at intervals of one month of age. The highest peak occurred between 5 and 6 months of age.
According to the data we collected, the most common reason for enrolling children in child care (90.7% of cases) was that parents were employed and nobody else was available to care for the child.
Behaviour of the two groups (attending/not attending child care) in relation to the different diseases under studyWe assessed and compared the following for each disease in each of the two cohorts (attending/not attending child care):
- •
Incidence (having suffered one or more episodes of the various diseases).
- •
Mean number of episodes.
- •
Relative risk (RR) of having the disease.
- •
Adjusted risk.
When it came to the mean number of episodes experienced by the children, we found statistically significant differences for all the diseases under consideration (P<.05), except for severe infections with a very low incidence (bacteraemia, meningitis and sepsis) and for viral pharyngitis and sinusitis. We also found clear differences between both groups when we compared the incidence of disease, save for the aforementioned diseases and influenza, laryngitis and recurrent wheezing.
Children that attended child care had a higher adjusted risk for having bronchiolitis, bronchitis, conjunctivitis, exanthematous viral illnesses, pharyngotonsillitis, gastroenteritis, pneumonia, otitis media and recurrent wheezing (Table 2).
Incidence, mean number of episodes, relative and adjusted risk of suffering the different diseases for the two cohorts under study (attending or not attending child care) of children 0–24 months of age.
| % of children with at least one episode by child care attendance or lack thereof, and P value | Mean number of episodes by child care attendance or lack thereof, and P value | Relative risk of suffering the diseasesRR (95% CI) | Adjusted riskaOR (95% CI) | |||||
|---|---|---|---|---|---|---|---|---|
| In child care N=549 | Not in child careN=426 | P | Not in child careN=549 | In child careN=426 | P | |||
| Bacteraemia | 0.04 | 0.9 | .40 | 0 | 0.01 | .23 | 2.58 (0.47–1.4) | 2.92 (0.13–22.56) |
| Bronchiolitis | 25.8 | 37.1 | <.01 | 0.34 | 0.51 | <.01 | 1.43 (1.19–1.73) | 1.91 (1.36–2.69) |
| Bronchitis | 27.8 | 44.1 | <.01 | 0.47 | 0.82 | <.01 | 1.57 (1.33–1.87) | 1.77 (1.28–2.46) |
| Conjunctivitis | 32.8 | 48.8 | <.01 | 0.49 | 0.81 | <.01 | 1.46 (1.26–1.71) | 2.19 (1.59–3.04) |
| Exanthematous viral illnesses | 27.8 | 40.8 | <.01 | 0.39 | 0.58 | <.01 | 1.46 (1.23–1.75) | 1.56 (1.12–2.19) |
| Viral pharyngitis | 32.1 | 35.2 | .36 | 0.48 | 0.59 | .07 | 1.11 (0.93–1.33) | 1.08 (0.78–1.49) |
| Pharyngotonsillitis | 13.3 | 23.2 | <.01 | 0.18 | 0.35 | <.01 | 1.77 (1.34–2.33) | 2.17 (1.45–3.27) |
| Gastroenteritis | 45.7 | 57 | .02 | 0.72 | 0.95 | <.01 | 1.25 (1.11–1.42) | 1.68 (1.23–2.30) |
| Influenza | 7.9 | 12 | .15 | 0.09 | 0.15 | .03 | 1.49 (1.02–2.19) | 1.27 (0.75–2.13) |
| Laryngitis | 21.3 | 26.3 | .20 | 0.3 | 0.43 | .01 | 1.23 (0.98–1.55) | 1.41 (0.99–2.03) |
| Meningitis | 0.9 | 0.9 | .63 | 0.01 | 0.01 | .82 | 1.03 (0.28–3.81) | 0.53 (0.08–2.79) |
| Pneumonia | 3.4 | 8 | .01 | 0.04 | 0.09 | .01 | 2.31 (1.33–3.98) | 2.18 (1.08–4.56) |
| Otitis media | 29.4 | 48.8 | <.01 | 0.5 | 1 | <.01 | 1.64 (1.39–1.93) | 2.01 (1.47–2.77) |
| Common cold | 90.5 | 93.7 | .01 | 3.46 | 4.35 | <.01 | 1.03 (0.99–1.07) | 1.55 (0.86–2.86) |
| Sepsis | 4.1 | 4.5 | .94 | 0.06 | 0.06 | .83 | 1.11 (0.61–2.03) | 0.88 (0.41–1.88) |
| Recurrent wheezing | 12.4 | 20.9 | .06 | 0.31 | 0.57 | <.01 | 1.69 (1.26–2.25) | 2.09 (1.35–3.28) |
| Sinusitis | 6.8 | 10.6 | .35 | 0.18 | 0.22 | .55 | 1.53 (1.01–2.3) | 1.44 (0.83–2.49) |
| Viral illness | 4.5 | 8.5 | <.01 | 0.05 | 0.09 | .02 | 2.07 (1.21–3.35) | 1.65 (0.89–3.07) |
Of all children in the sample, 7.3% were attending child care at 6 months, 18.56% at 12 months, 32.51% at 18 months and 43.7% at 24 months.
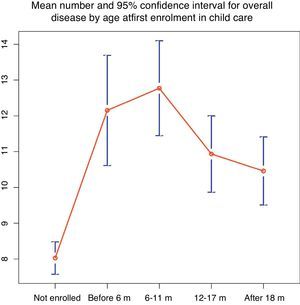
The mean number of episodes of disease (for all diseases) was lower in children that did not attend child care, and highest in children that started attending child care in the first 12 months of life (Fig. 2).
In children that had started attending child care by 6 months, the RR of having pneumonia, otitis media, recurrent wheezing or viral illnesses was twice as large (Table 3), and the RR of having bronchiolitis, bronchitis and exanthematous viral illnesses was 1.5 times to twice as large. While the RR for having conjunctivitis, gastroenteritis and common colds was higher in children that attended child care, we found no statistically significant differences based on age at first enrolment.
Relative risk (RR) of suffering the various illnesses by age at first enrolment in child care.
| RR for first enrolment before age 6mN=72(95% CI) | RR for first enrolment at age 6–11mN=109(95% CI) | RR for first enrolment at age 12–17mN=136(95% CI) | RR for first enrolment after age 18mN=109(95% CI) | |
|---|---|---|---|---|
| Bronchiolitis | 1.87 (1.42–2.47) | 1.52 (1.16 2.01) | 1.34 (1.02–1.75) | 1.17 (0.85–1.61) |
| Bronchitis | 1.83 (1.41–2.38) | 1.93 (1.55–2.4) | 1.18 (0.86–1.55) | 1.53 (1.19–1.98) |
| Conjunctivitis | 1.58 (1.24–2.03) | 1.57 (1.26–1.94) | 1.48 (1.2–1.81) | 1.27 (0.98–1.62) |
| Exanthematous viral illnesses | 1.74 (1.32–2.29) | 1.48 (1.14–1.92) | 1.45 (1.13–1.85) | 1.28 (0.96–1.71) |
| Viral pharyngitis | 0.92 (0.63–1.34) | 1.04 (0.78–1.39) | 1.18 (0.92–1.52) | 1.22 (0.93–1.58) |
| Pharyngotonsillitis | 1.27 (0.73–2.23) | 2.03 (1.39–2.96) | 2.02 (1.42–2.87) | 1.54 (1.001–2.37) |
| Gastroenteritis | 1.28 (1.03–1.59) | 1.25 (1.04–1.51) | 1.32 (1.12–1.56) | 1.15 (0.94–1.4) |
| Influenza | 1.73 (0.91–3.29) | 1.37 (0.75–2.51) | 1.28 (0.72–2.27) | 1.72 (0.99–2.97) |
| Laryngitis | 1.3 (0.87–1.96) | 1.55 (1.13–2.12) | 1.21 (0.87–1.67) | 0.9 (0.59–1.37) |
| Pneumonia | 2.81 (1.22–6.45) | 2.91 (1.43–5.95) | 1.69 (0.76–3.79) | 2.12 (0.95–4.72) |
| Otitis media | 2.01 (1.59–2.53) | 1.82 (1.47–2.26) | 1.41 (1.11–1.78) | 1.51 (1.18–1.93) |
| Common cold | 1.09 (1.05–1.13) | 1.03 (0.98–1.09) | 1.01 (0.96–1.07) | 1.02 (0.96–1.08) |
| Recurrent wheezing | 2.35 (1.54–3.59) | 1.63 (1.05–2.52) | 1.66 (1.12–2.48) | 1.33 (0.83–2.15) |
| Sinusitis | 1.81 (0.91–3.58) | 1.46 (0.77–2.76) | 1.81 (1.05–3.09) | 1.06 (0.51–2.21) |
| Viral illness | 2.65 (1.23–5.71) | 1.09 (0.42–2.82) | 1.93 (0.96–3.86) | 2.63 (1.25–5.12) |
We assessed the potential influence of other variables included in the study on the incidence of bronchiolitis, bronchitis, exanthematous viral illnesses, pneumonia, acute otitis media, recurrent wheezing, viral illnesses and acute gastroenteritis.
We found no association between gestational age, maternal or paternal smoking, and vaccination against pneumococcus and the incidence of these diseases. Table 4 presents the variables for which we found an association.
Relative risk (RR) of suffering the diseases for which we found an association with the different variables under study.
| Bronchiolitis(95% CI) | Bronchitis(95% CI) | Recurrent wheezing(95% CI) | Pneumonia(95% CI) | Gastroenteritis(95% CI) | |
|---|---|---|---|---|---|
| Neonatal morbidity | 1.59 (1.24–2.06) | ||||
| Female sex | 0.65 (0.53–0.85) | 0.75 (0.62–0.89) | 0.51 (0.38–0.7) | – | |
| Presence of siblings | 1.25 (1.01–1.57) | – | 1.52 (1.14–2.03) | 0.77 (0.67–0.88) | |
| Maternal asthma | 1.34 (1.04–1.72) | 1.81 (1.28–2.57) | |||
| Maternal allergies | 1.35 (1.11–1.64) | 1.81 (1.05–3.11) |
We found no association between breastfeeding and the incidence of the diseases under study.
Use of resourcesChild care attendance was associated with a statistically significant increase in the number of visits to emergency services and paediatric clinics in every age group under study (Table 5).
Mean number of visits per month to emergency room and paediatrician before and after enrolment in child care for different age intervals.
| Age intervals | Mean number of visits/month to emergency room by age interval and P value | Mean number of visits/month to paediatrician by age interval and P value | ||||
|---|---|---|---|---|---|---|
| Before enrolment in child care | After enrolment in child care | P | Before enrolment in child care | After enrolment in child care | P | |
| 6–11m | 0.09 | 0.16 | <0.01 | 0.27 | 1.24 | <0.01 |
| 12–17m | 0.09 | 0.15 | <0.01 | 0.55 | 0.83 | <0.01 |
| 18–24m | 0.03 | 0.49 | <0.01 | 0.57 | 0.96 | <0.01 |
The RR of using medications (antibiotics, inhaled or oral corticosteroids and montelukast) was greater in children that had enrolled earlier in child care (Table 6).
Relative risk (RR) for medication use by age at first enrolment in child care.
| Age at first child care enrolment | Antibiotics, RR (95% CI) | Oral corticosteroids, RR (95% CI) | Inhaled bronchodilators, RR (95% CI) | Oral bronchodilators, RR (95% CI) | Montelukast, RR (95% CI) |
|---|---|---|---|---|---|
| Less than 6m | 1.48 (1.35–1.62) | 2.15 (1.69–2.73) | 2.01 (1.49–2.7) | 1.72 (1.29–2.27) | 3.69 (2.14–6.37) |
| 6–11m | 1.36 (1.23–1.5) | 1.52 (1.17–1.97) | 2.01 (1.56–2.6) | 1.43 (1.09–1.88) | 1.83 (0.98–3.43) |
| 12–17m | 1.31 (1.18–1.45) | 1.08 (0.81–1.45) | 1.39 (1.04–1.86) | 0.96 (0.7–1.31) | 2.99 (1.79–4.79) |
| 18–24m | 1.11 (0.96–1.27) | 0.88 (0.61–1.26) | 1.21 (0.86–1.7) | 1.11 (0.8–1.51) | 0.46 (0.14–1.47) |
The mean number of courses of antibiotics received in the two years of the study was lower in children that did not attend child care (1.71). The largest numbers corresponded to children that started attending child care at 1–6 months of age (3.35) and those that started at 7–11 months of age (3.64), with the number decreasing in children that started child care at 13–18 months (2.78) and at age 18 months and older (2.17).
DiscussionWe conducted this study in the PC paediatric offices of the public health system, where 75% to 100% of the children receive care on a regular basis.11–13
The study was conducted by 33 paediatricians and 20 nurses on a voluntary basis. They collected the data in the course of regular paediatric visits to optimise the research capacity of PC paediatrics. The number of participating paediatricians allowed the recruitment of a large sample, but it carried a potential lack of uniformity in diagnostic criteria, which we tried to minimise by establishing definitions before the start of the study.
As for the methodology, the study started with two cohorts that were initially uniform, but exposure to the independent variable (child care attendance) could be associated with other potential confounding factors, so we controlled for all the variables included in the study. The comparison of the two cohorts only revealed significant differences (Table 1) in the history of vaccination against pneumococcus and rotavirus (probably because these vaccines are particularly recommended if children attend child care), in the level of education of fathers and mothers, and in maternal employment, with active employment of the mother being precisely the main reason why children were enrolled in child care.
When it came to the diseases that we analysed, in addition to infectious illnesses we studied the episodes of recurrent wheezing because they are a potentially severe condition with a high prevalence in Asturias (45.6% of children have at least one episode of wheezing in the first 36 months of life).14 Each episode of disease leading to a health visit and resulting in a specific diagnosis was documented a single time, even if the child visited health services more than once for the same episode.
Of all the children in our sample, 43.7% attended child care, similar to the figure reported in “Estadística de las enseñanzas no universitarias,”15 according to which 49.8% of children are enrolled in out-of-home care by 2 years. More than 90% of respondents in our study reported that the reason for sending their child to child care was “being employed and not having anyone to take care of them”.
Consistent with other published studies5,16,17 the incidence of infectious disease was higher in children that attended child care than in those that did not. The relative risks of suffering the different diseases increased in percentages similar to those observed in other studies,8 so that the risk of pneumonia increased by 131%, that of recurrent wheezing by 69%, that of bronchitis by 57% and that of otitis media by 64%. When we transformed the estimated risks to attributable proportions, we found that child care attendance could account for 36% of pneumonias, 23% of recurrent wheezing cases, 30% of viral illnesses, 25% of pharyngotonsillitis cases, and 20% of bronchitis cases.
Since early enrolment in child care increases the “exposure time” to it, and considering that one of the factors with the strongest influence on the incidence of infectious disease is the age at enrolment,18 we calculated the influence of this exposure factor for each age interval on each of the diseases under consideration. We observed that early enrolment in child care (before age 12 months) was associated with an increase in the number of episodes of disease overall (Fig. 2). The RR (Table 3) of suffering from the potentially most severe diseases (pneumonia, otitis media, bronchitis, bronchiolitis and recurrent wheezing) was between 1.5 and 2 times higher in children that started attending child care before age 6 months. The RR of suffering from recurrent wheezing was particularly noteworthy, as it was 1.69 for children that attended child care, and rose to 2.35 in children that started attending in the first 6 months of life.
The RR of contracting pneumonia was 2.31 times higher in children that attended child care, and it increased to 2.81 in children that started attending before age 6 months. Other published works have reported RRs that were higher by factors of 9.4919 and 5.1416; vaccination against pneumococcus, which reaches a coverage of 85% in our region, may play a significant role in this.
One limitation of the study is that we did not take into account the characteristics of the child care centres nor the time spent at the centre by each child; in this regard, a study of similar characteristics that was also conducted in a public health service16 did not find differences in disease incidence depending on the number of hours spent at the child care centre nor the child-to-caregiver ratio in the facility.
We recorded the prevalence of breastfeeding (BF) and the age at which it was discontinued; we did not document exclusive BF, but overall BF. Our analysis of the role of BF on infant morbidity did not reveal a significant protection against infectious diseases. While the protective effect of BF has been widely documented,17,20 our results are similar to those of other studies in developed countries.21,22 Still, the data of our study must be interpreted with caution, as the study was not designed to assess the influence of BF in the morbidity of the sample, which may result in various biases.20,23
The number of visits, both to paediatric clinics and to emergency services, includes every time that the children sought services, even if more than one visit was made for a single episode. The mean number of visits to the emergency room was higher in children that attended child care and increased if attendance started at an early age, with the mean number of visits per year to the emergency room being 1 in children that did not attend child care and 2.3 in children that were enrolled by age 6 months. The number of visits per year to the paediatrician ranged from a mean of 6.3 in children that did not attend child care to a mean of 9 in children that started attending before age 6 months. When it came to the use of medications, 85% of children that attended child care had taken antibiotics and 40% had used bronchodilators, compared to 68% and 22.7%, respectively, of children that were never enrolled in child care.
We feel that it is necessary that we continue to followup the two cohorts to assess their outcomes after school enrolment at 4 and 5 years of age.
ConclusionsChild care attendance is a risk factor for contracting infectious diseases. The risk is higher when children attend at earlier ages; and this is also true of the risk of using pharmacological agents and of the use of emergency room and paediatric services.
Some of these diseases, such as bronchiolitis, recurrent wheezing, pneumonia and otitis, may have a significant impact on the health of the affected children. The high frequency of episodes of disease suffered by children, even if the processes are mild, can affect their development.
Parents and guardians send children to child care mostly because they work and there is nobody else who can take care of them. They should be appropriately informed to be able to make the best choices for their children.
Considering these results, it seems advisable that alternative strategies are considered for taking care of the youngest children, and that public authorities grant parents the opportunity to choose the best type of care for their children, extending the duration of maternity, paternity and breastfeeding leaves, as has already been done in other countries in the European Union.
FundingThis study has been funded by the Oficina de Investigación Biosanitaria del Principado de Asturias (Office of Biological Health research of the Principality of Asturias [OIB]) File AP10-11, Resolution of June 25, 2010.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors are thankful for the help received from the Unidad de Consultoría Estadística (Unit of Statistics Consulting) of the Servicios Científico-Técnicos (Scientific and Technical Services) of the Universidad de Oviedo, and in particular for the help of Tania Iglesias Cabo, and the contributions in the editing of this article of the family physician Ángel Comas Fuentes.
We are carrying out a research project called “Influence of child care attendance on the morbidity and use of health care resources in children 0 to 2 years of age”.
We are going to study children that attend child care and children that do not in order to compare the number of infections that they develop.
We will be collecting data on your child and any diseases that your child has in the first two years of life.
We will at no point perform diagnostic tests nor recommend treatments that are not indicated for whichever disease your child has.
The participation of your child is voluntary, and you can withdraw your child from the study whenever you so choose.
The personal data of your child will be kept confidential at all times, conforming to the law currently in force in Spain (Law 15/99 on the protection of personal data).
We hope that you will be interested in this initiative, and that we can count on your help and collaboration.
If you need further information, please ask your doctor.
I, ……………………………………………………………………………………… (first and last names)
As the………………………………………………………………………. (relationship with participant)of…………………………………………………………………………………………………………………………………….(name of participant)
Agree for his/her participation in this study.
Signature of patient representative Signature of paediatrician
Name of signing party/date
Aidé Aladro Antuña, Ana María Pérez López, Begoña Domínguez Aurrecoechea, Encarnación Díez Estrada, Francisco Javier Fernández López, José Ignacio Pérez Candás, Leonor Merino Ramos, María Fernández Francés, María Ángeles Ordóñez Alonso, Purificación López Vilar, Sonia Ballesteros García.
Collaborators in research: Isabel González-Posada Gómez; Sonia Alonso Álvarez; María Agustina Alonso Álvarez-Diana Solís; Diana Josefina Collao Alonso-Margot Morán Gutiérrez; Ángel Costales-Gloria Peláez; Mar Coto Fuente-Mónica Cudeiro Álvarez; José I. Pérez Candás-Beatriz Fernández López;Ana Mª Pérez López-Mª Pilar Flórez Rodríguez; Leonor Merino Ramos-Cruz Andrés Álvarez; Isolina Patallo Arias-Mónica Fernández Inestal; Ana Pérez Baquero-Carmen Díaz Fernández; Silvia Ruisanchez Díez; María Fernández Francés-Antonia Sordo-Sonia Ballesteros-Mª Antonia Castillo; Begoña Domínguez-Lidia González Guerra; Águeda García Merino; Encarnación Díez Estrada-Teresa García; Francisco J. Fernández López-M. Teresa Cañón del Cueto; Purificación López Vilar-Laura Tascón Delgado; Isabel Tamargo Fernández; Laura Lagunilla Herrero; Concepción Polo Mellado-Cruz Bustamante Perlado Susana Parrondo-Nevada Juanes Cuervo; Ana Arranz Velasco; Belén Aguirrezabalaga González; Mario Gutiérrez Fernández; Isabel Mora Gandarillas; Rosa Mª Rodríguez Posada; Isabel Fernández Álvarez Cascos; Isabel Carballo Castillo; Felipe González Rodríguez-Tatiana Álvarez González; Zoa Albina García Amorin; Aidé Aladro Antuña-Monserrat Fernández Revilla; Fernando Nuño Martín; Maria Ángeles Ordóñez Alonso.
Please cite this article as: Domínguez Aurrecoechea B, Fernández Francés M, Ordóñez Alonso MÁ, López Vilar P, Pérez Candás JI, Merino Ramos L, et al. Enfermedad infecciosa y consumo de recursos sanitarios en menores de 2 años que acuden a guarderías. An Pediatr (Barc). 2015;83:149–159.
Previous presentation: This study was presented at the European Congress in Primary Care Paediatrics; July 2013; Tel Aviv, Israel.