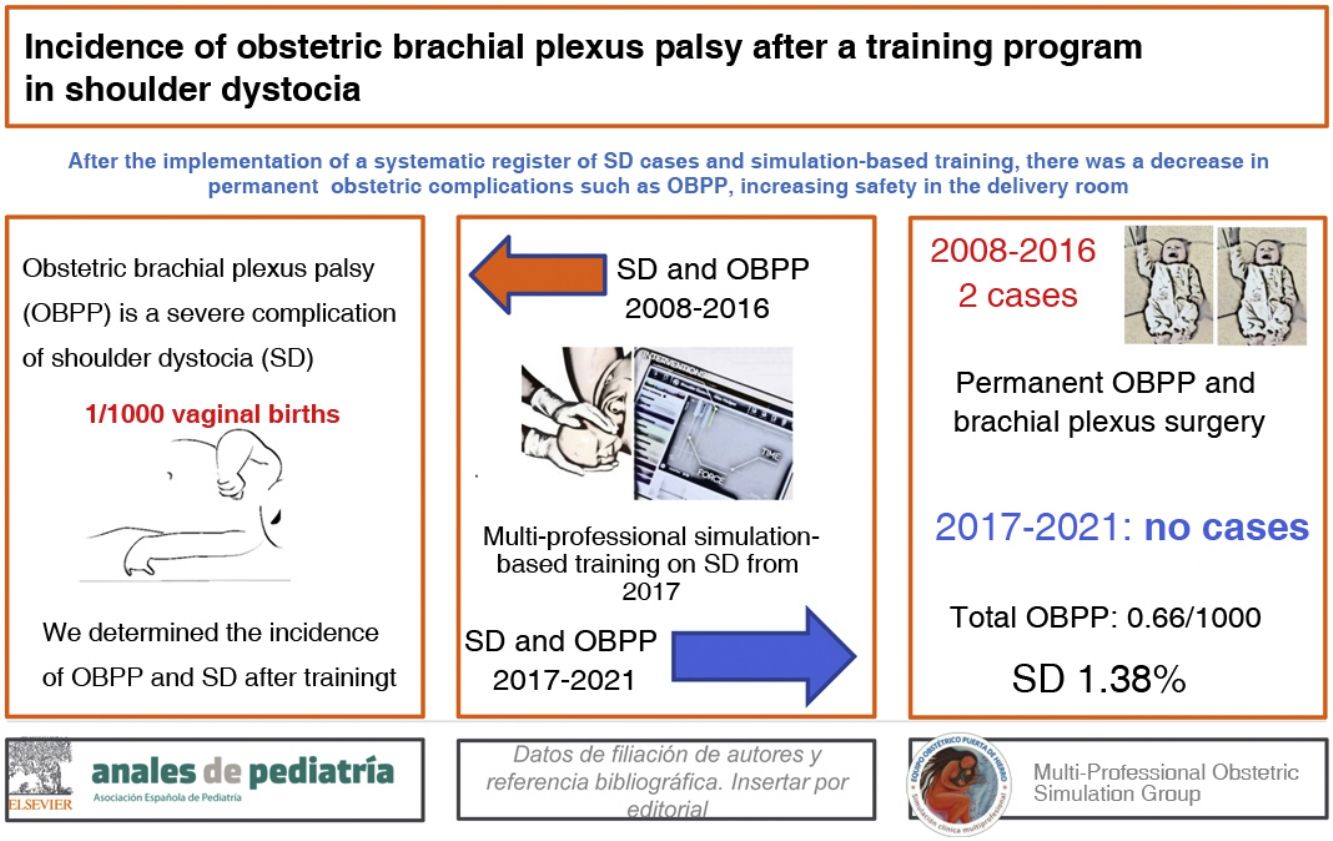
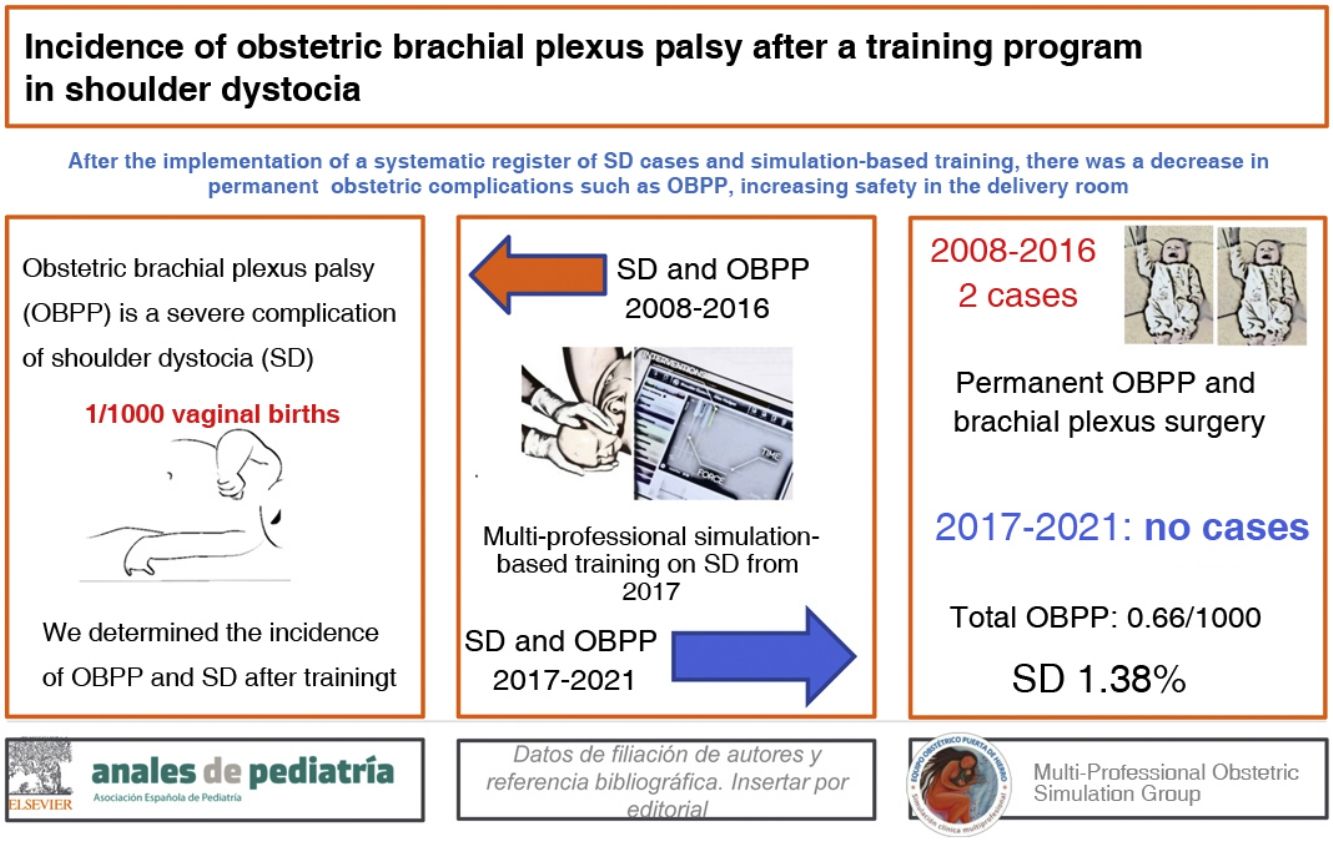
Shoulder dystocia is a nonpreventable obstetric emergency that causes severe complications, such as obstetric brachial plexus palsy. The objective of the study was to determine the incidence of obstetric brachial plexus palsy and other neonatal complications associated with shoulder dystocia in deliveries managed in a university hospital after the implementation of a simulation-based training that was offered to all the labour and delivery staff on a voluntary basis.
Material and methodsRetrospective observational study including all cases of shoulder dystocia and associated complications (mainly obstetric brachial plexus palsy) documented between January 2017 and December 2020, after the implementation of the training. In addition, we collected retrospective data on cases of obstetric brachial plexus palsy that developed in the hospital before the training (2008–2016).
ResultsIn the 2017–2020 period, in the total of 125 cases of shoulder dystocia (amounting to 1.38% of vaginal deliveries), there were 14 cases of obstetric brachial plexus palsy (11.2% of the cases of shoulder dystocia), 7 clavicle fractures and 1 humerus fracture; none of the cases of obstetric brachial plexus palsy was permanent or required treatment or rehabilitation past six months. In the years preceding the training, there were 7 cases of obstetric brachial plexus palsy, 2 permanent and 5 temporary (3 of which required rehabilitation).
ConclusionThese results reflect the importance of knowing the morbidity present in the labour and delivery ward and the potential benefit of simulation-based training programmes in the resolution of these obstetric complications.
La distocia de hombros es una emergencia obstétrica no prevenible que causa graves complicaciones, como la parálisis braquial obstétrica. El objetivo del estudio fue determinar la incidencia de parálisis braquial obstétrica y de otras complicaciones neonatales asociadas a la distocia de hombros en los partos atendidos en un Hospital Universitario tras la implantación de un curso basado en simulación, de carácter voluntario y destinado a todos los profesionales en paritorio.
Material y métodosEstudio observacional retrospectivo; registro de los casos de distocia de hombros y de las complicaciones asociadas (principalmente parálisis braquial obstétrica) que tuvieron lugar entre enero de 2017 y diciembre de 2020, tras la implantación del curso. De forma paralela, se rescataron los casos de parálisis braquial obstétrica que tuvieron lugar en el hospital antes del entrenamiento (2008–2016).
ResultadosEn el período 2017–2020, de entre 125 distocias de hombros (lo que representa el 1,38% de los partos vaginales), hubo 14 casos de parálisis braquial obstétrica (el 11,2% de las distocias de hombros), siete fracturas de clavícula y una fractura de húmero; ninguna de las parálisis braquiales obstétricas fue permanente ni precisó de tratamiento o rehabilitación más allá de los seis meses. En los años anteriores al entrenamiento, hubo siete casos de parálisis braquial obstétrica, dos permanentes y cinco transitorias (tres de las cuales precisaron rehabilitación).
ConclusiónEstos resultados reflejan la importancia de conocer la morbilidad presente en el paritorio y el posible beneficio de la formación basada en simulación para la resolución de estas complicaciones obstétricas.
Shoulder dystocia (SD) is an unpredictable and unpreventable obstetric emergency.1,2 It occurs when the shoulders of the foetus are stuck in the mother’s pelvis and additional manoeuvres are required to deliver the baby (Table 1). It is very infrequent, but it entails serious complications for the mother (postpartum haemorrhage and fourth degree tear), and the neonate (such as obstetric brachial plexus palsy),2–5 the incidence of which may increase with inadequate management of SD,6–8 in addition to clavicle and/or humerus fractures, brachial plexus injury, foetal hypoxia and, on rare instances, neonatal death.1,9
Manoeuvres used for resolution of shoulder dystocia.
| First-line manoeuvres | |
|---|---|
| McRoberts manoeuvre | Hip hyperflexion with opening of the lumbosacral angle and flattening of the pelvis by 6 °, which helps the shoulder drop |
| Suprapubic pressure | Exerted on the anterior shoulder in the direction of the foetal chest to help the shoulder dislodge from the symphysis while producing a modest shortening of the foetal bisacromial diameter. |
| Gaskin manoeuvre | The mother is rolled on all fours on a flat and preferably elevated surface |
| Second-line manoeuvres | |
|---|---|
| Posterior arm delivery | The hand is introduced in the sacral hollow to reach the posterior shoulder. Pressure is exerted on the antecubital fossa to make the forearm flex. Then, the arm is carefully passed over the chest |
| Woods manoeuvre | (Woods corkscrew manoeuvre) Rotation of the posterior shoulder by 180° to bring it to the anterior position thereby dislodging the anterior shoulder |
| Rubin manoeuvre | Pressure is applied on the scapula of the anterior shoulder in the direction of the sternum to adduct the shoulder and reduce the bisacromial diameter |
| Third-line manoeuvres | |
|---|---|
| Abdominal rescue | Performance of emergency caesarean section with low transverse hysterectomy to perform manoeuvres through the incision to disimpact the shoulder and assist vaginal extraction. |
| Zavanelli manoeuvre | Cephalic replacement followed by caesarean delivery |
SD, shoulder dystocia.
On the other hand, obstetric brachial plexus palsy (OBPP) is a condition that develops during childbirth and may involve the whole or part of the upper extremity, resulting in complete paralysis or limited active motion due to mechanical injury to brachial plexus nerves.10,11 The incidence of OBPP is estimated at 1.5–2 cases per 1000 live births and its clinical presentation depends on the nerve roots involved and the extent of the injury. The most frequent form involves nerve roots C5 and C6 (upper plexus or Duchenne-Erb palsy) manifesting with functional impairment of the shoulder, followed by involvement of the upper and intermediate plexus (C5–C7).12,13 The nerve injury is classified into 3 categories based on the traumatic stretching of the axons contained in the brachial plexus, which are, in order of increasing severity and poorer prognosis, neurapraxia, axonotmesis and neurotmesis.14,15
The Practical Obstetric Multi-Professional Training (PROMPT) Foundation classifies OBPPs with a pragmatic approach that does not adhere to any of the published classifications. It considers brachial plexus palsy temporary in cases in which, after SD, some sign of arm weakness is detected but resolves completely without treatment or surgery within 12 months. Its protocol also contemplates a medium-term analysis, cases of OBPP that persist up to 6 months. The cases of OBPP it considers most severe are those lasting longer than 12 months.16,17
The PROMPT Foundation in Bristol has developed a multi-professional obstetric emergencies training programme, lasting 1 day, that has been validated and described in previous publications.18–20 A decade after the introduction of this simulation-based annual programme of mandatory, multi-professional training for intrapartum emergencies, there were no cases of permanent brachial plexus injury in the Southmead Hospital in Bristol (United Kingdom).16,17
The multi-professional obstetric simulation group is a group of obstetricians, midwives, nurses and anaesthesiologists trained in the PROMPT programme developed in the United Kingdom that has been offering simulation-based training in the management of several obstetric emergencies, including SD, since June 2015.
The objective of the study was to determine the incidence of OBPP and other neonatal complications associated with SD in deliveries managed in our university hospital between January 2017 and December 2020 after the implementation of a simulation-based training that was offered to be taken on a voluntary basis to all the health care staff involved in managing childbirth in the obstetric unit.
Material and methodsWe conducted a retrospective observational study in a university hospital in Madrid, Spain. The study was approved by the ethics committee for research with medicines of the hospital on June 21, 2021 (file: PI90/21).
Our hospital implemented a standardised training programme similar to the PROMPT, between 2017 and 2020. The instructors were accredited by the PROMPT Foundation or trained through the multi-professional obstetric simulation group in programmes developed by the Sociedad Española de Simulación Clínica y Seguridad del Paciente (Spanish Society of Clinical Simulation and Patient Safety). Shoulder dystocia workshops were held to train obstetricians, midwives, medical interns/residents (MIR programme) and nursing interns/residents of the hospital.
Later on, we reviewed the health records of patients born in the labour and delivery unit of our hospital between January 2017 and December 2020 (both included) to obtain data on the SD cases that occurred during that period and the complications associated with this emergency, paying particular attention to cases of OBPP and humerus and clavicle fractures. We also included cases of patients delivered in the hospital without a postpartum diagnosis of OBPP or SD but who received care for either of them at a later time in the paediatric rehabilitation unit or paediatric neurology unit of our hospital. We excluded children with OBPP delivered in other hospitals, even if the infant was later managed in any of the paediatric unites in our hospital.
We collected data in an Excel spreadsheet with the aim of determining the incidence of SD and other postpartum complications and to investigate the follow-up of both mother and child. The information collected in the spreadsheet had been originally recorded in three different care settings:
- 1
Delivery room: labour and childbirth records, completed by health care professionals managing deliveries in forms available in the delivery room (custom form: Appendix B) and signed by the on-call physician in charge.
- 2
Neonatal unit/maternity ward: for cases in which SD was not documented in the delivery room but the neonatologist diagnosed OBPP, clavicle fracture or humerus fracture in an examination of the infant.
- 3
Paediatric neurology clinic: for cases of infants delivered in our hospital who were eventually referred back from primary care after detection of the complication.
We collected data on the following variables: labour onset and type of delivery (in the case of assisted vaginal delivery, we differentiated between the use of Thierry spatulas, vacuum extractor and forceps), maternal age, gestational diabetes, parity (nulliparous/multiparous), detection of SD and associated complications (permanent/temporary OBPP, clavicle fracture, humerus fracture), the manoeuvre used to resolve SD, the initial provider managing the situation and the provider that resolved the SD. In the case of OBPP, clavicle fracture or humerus fracture, in addition to the previous information we recorded the birth weight, 1- and 5-min Apgar scores, umbilical cord blood pH, the need of neonatal resuscitation and the management of the complication (did not require treatment, rehabilitation or surgery), in addition to other maternal complications (tearing, postpartum haemorrhage).
We performed a descriptive analysis of the data, using absolute frequencies and percentages to summarise categorical variables and the mean and standard deviation to summarise continuous variables.
The study was divided in 2 periods: 2017−2018, corresponding to the first 2 years following the introduction of the training and the specific documentation of SD in the delivery room, and 2019−2020, when most of the staff had already participated in at least 1 training on SD. Thus, to assess for potential differences between both periods in the incidence of neonatal complications associated with SD, we compared the data with the χ2 test or the Fisher exact test. All statistical tests were bilateral and we considered results significant if the P value was less than 0.05. The analyses were performed with the software SPSS, version 20 (IBM Inc, Chicago, IL, USA).
In addition, we investigated and retrieved data on cases of obstetric trauma (OBP and/or fractures) before the study period, specifically from 2008 (when the hospital opened) to 2016 (before the protocol for the documentation of SD was introduced in the hospital) by reviewing historical health records of the hospital and the department of paediatrics and rehabilitation.
ResultsBetween January 2017 and December 2020, there were 125 documented cases of SD in our hospital, with a cumulative incidence of 1.38% of the total vaginal births.
The form used to document cases of SD includes fields to specify the manoeuvres used to resolve SD and the provider that achieved the resolution. We found that 72% (90/125) of SD cases were resolved within 2 min, and in 16% (20/125) of cases the head to body delivery interval was greater than 2 min. In 44% (55/125) of cases the first provider managing the emergency was a midwife, in 43.2% (54/125), an obstetrics medical resident and in 9.6% (12/125) and obstetrician. In 44.8% (56/125) of cases, SD was resolved by a midwife, in 45.6% (57/125) by an obstetrics medical resident and in 9.6% (12/125) by an obstetrician. In addition, 5.6% (7/125) were resolved with the McRoberts manoeuvre; 52% (65/125) combining the McRoberts manoeuvre and suprapubic pressure (total of 56.8% resolved with first-line manoeuvres) and 42.4% (53/125) with second-line manoeuvres. The usual second-line manoeuvre was the delivery of the posterior arm, and internal rotational manoeuvres were used in 5.6% (7/125) of the cases that required second-line measures. Manoeuvres that are currently discouraged, such as fundal pressure (Kristeller manoeuvre) or excessive non-axial traction were used in 10.4% (13/125) of the cases.
In the same period (2017–2020), there were 14 cases of OBPP secondary to SD (corresponding to 11.2% of SD cases), 8 of which resolved spontaneously by 48 h post birth. The remaining 6 cases of OBPP required follow-up: in 4 cases, observation in the neonatal unit was sufficient, and the palsy resolved before the infant reached age 1 month, while in the other 2, patients were followed up in the neurology and rehabilitation departments, with resolution within 6 months. Thus, none of the 14 cases of OBPP required treatment. There were no documented cases of OBPP that were not associated with dystocia.
When it came to fractures, there were 8 cases between January 2017 and December 2020: 7 were clavicle fractures and 1 a humerus fracture. The 7 clavicle fractures were managed with immobilization and resolved without complications (with follow-up at the primary care level), discharging the infant without need of rehabilitation, and the patient with a humerus fracture was referred to the traumatology department for rehabilitation and discharge at age 2 months.
The distribution by type of delivery of the 21 cases of complications associated with SD described above (14 of OBPP and 7 fractures) was as follows: 11 normal vaginal delivery, 10 operative delivery (8 with spatulas and 2 with forceps). Of these 21 infants, 7 were admitted to the neonatal unit at birth: 1 due to the humeral fracture (with no OBPP), 3 due to respiratory distress syndrome (with good outcomes in 2 h), and the remaining 3 due to neonatal depression (2 of who required resuscitation with tracheal intubation). One of the latter patients also developed mild hypoxic-ischaemic encephalopathy. In this subset of 7 infants, the mean birth weight was 3936 g (range, 3384–4526) and the 1-min Apgar was less than 4 points in 42.9% (3/7), 4–6 points in 42.9% (3/7) and greater than 7 in 14.28% (1/7); however, none of the 7 (0.0%) had a 5-min Apgar score of less than 7 and the mean pH value was 7.22. When it came to the measures taken to stabilise the newborn, 1 of them did not require any, 4 required ventilation with intermittent positive pressure and 2 required resuscitation with tracheal intubation.
Table 2 presents the distribution by period (2017−2018 vs 2019−2020) of SD cases and the associated complications.
Characteristics of the deliveries and cases of should dystocia registered in the 2017–2020 period.
| 2017−2018 | 2019−2020 | Total study period | ||
|---|---|---|---|---|
| Number and type of deliveries | Number of deliveries | 5766 | 5425 | 11 191 |
| Caesarean deliveries | 1146 | 964 | 2110 | |
| Vaginal deliveries | 4620 | 4461 | 9081 | |
| Complications | Shoulder dystocia | 56 | 69 | 125 |
| Incidence of SD | 1.21% | 1.55% | 1.38% | |
| Permanent OBPP | 0 | 0 | 0 | |
| OBPP < 12 months | 12 | 2 | 14 | |
| Clavicle fracture | 5 | 2 | 7 | |
| Humerus fracture | 1 | 0 | 1 | |
| Characteristics of cases of SD | Induced deliveries | 22/56 (39.3%) | 29/69 (42.1%) | 40.8% |
| Uncomplicated deliveries | 34/56 (60.7%) | 40/69 (57.9%) | 59.2% | |
| Spatulas | 15/56 (26.7%) | 12/69 (17.4%) | 21.6% | |
| Forceps | 8/56 (14.2%) | 18/69 (26.1%) | 20.8% | |
| Nulliparous | 41/56 (73.2%) | 52/69 (75.4%) | 74.4% | |
| Multiparous | 15/56 (26.8%) | 17/69 (24.6%) | 25.6% | |
| Gestational diabetes | 18/56 (32.1%) | 14/69 (20.3%) | 25.6% |
OBPP, obstetric brachial plexus palsy; SD, shoulder dystocia.
In the first 2 years following the introduction of training (2017–2018) there were 56 documented cases of SD (1.21% of vaginal deliveries), associated with 12 cases of temporary OBPP (21.4% of cases of SD) and no cases of permanent OBPP, 5 clavicle fractures and 1 humerus fracture.
In the following 2 years (2019−2020), when most health care staff had already undergone at least 1 training, there were 69 documented cases of SD (1.55% of vaginal deliveries), 2 cases of temporary OBPP (2.90% of SD cases) and no cases of permanent OBPP, and 2 clavicle fractures.
The difference in the incidence of SD and of fractures between the 2 periods (2017−2018 vs 2019−2020) was not statistically significant (P = .162 and P = .138, respectively); but the risk of OBPP following SD was significantly lower in the second period (P = .001).
Table 2 presents the results on the other characteristics of the deliveries and SD cases documented in each period.
On the other hand, the review of records from the 2008–2016 period revealed 8 cases of OBPP managed in the paediatric neurology unit of the hospital, 3 of which turned out to be permanent, with referral of the patient to the tertiary care hospital for surgical management, and 5 were temporary (3 required rehabilitation, with a favourable outcome and discharge before 6 months, and 2 resolved without treatment). We did not find any records of clavicle or humerus fractures associated with birth. We were not able to obtain a record of the number of cases of SD that occurred in these years, as there was no register of cases before the simulation-based training for the management of SD was introduced.
DiscussionTo our knowledge, this is the first study on the incidence of SD and OBPP in a Spanish hospital.
One of the strengths of the study is that we collected data from three different units to avoid any loss of information. In addition, this is the first study that has described the health care professionals that managed and resolved SD in the delivery room in Spain, and believe that this information is relevant for the purpose of choosing the professionals that lead training programmes on the management of this obstetric emergency.
As noted above, in the 4 years that followed the introduction of this training programme, 14 cases of OBPP have been documented, of which 8 resolved spontaneously within 48 h of birth, 4 within 1 month of birth, and only 2 required referral to the departments of neurology and rehabilitation, from which the patients were discharged before 6 months post birth. None of the cases of OBPP was permanent. These cases of OBPP corresponded to 11.2% of the total of 125 cases of SD documented out of the 9081 vaginal deliveries managed during the study period. In contrast, in the years preceding health care staff training on SD (2008–2016), there were 8 documented cases of OBPP, of which 3 were permanent and another 3 (out of the 5 temporary cases) required rehabilitation.
The absence of cases of permanent OBPP and of cases of OBPP requiring treatment or rehabilitation beyond 6 months post birth in our hospital after the introduction of the training programme was consistent with the evidence published by the research groups of Croft and Draycott, who also found a reduction in the frequency of permanent OBPP after training the majority of the staff in the delivery room using the PROMPT approach,17,19,21 and also with the results reported by Inglis et al.,7 whose methodology did not follow the PROMPT approach but was similar to it.
The literature does not only describe a reduction in the incidence of complications associated with SD with the implementation of training programmes for delivery room staff, but also shows that PROMPT trainings have an impact on liability costs, as evinced by Weiner et al. in Kansas, United States, and the Victorian Managed Insurance Authority of Victoria, Australia, in addition to the findings at the Hospital North Bristol Trust.22
It is worth adding that when we compared the incidence of OBPP in 2017−2018 (first years after introduction of the trainings) and 2019−2020 (a period when most health care professionals had participated in at least 1 training), we found that the risk of OBPP following SD had decreased by nearly 90% in the second period compared to the first.
Thus, based on our results, we consider that training on SD to reduce the morbidity associated with this emergency should be offered at regular intervals and be mandatory, in situ, multi-professional and free, as is in other countries such as the United Kingdom, Denmark and the United States.17,23,24 For instance, in the United Kingdom, the Royal College of Obstetricians and Gynaecologists recommends periodic multi-professional training4 and the Clinical Negligence Scheme for Trusts considers it a mandatory standard to reduce neonatal complications,25 and this training is funded by health care institutions. Thanks to this programme, the United Kingdom has not registered any case of permanent OBPP in the late training period, which corresponds to 9–12 years after the introduction of these courses.
The main limitation of our study is the lack of reliable data for the period preceding the introduction of the training and the SD register. The hospital opened in October 2008, but the SD register started in 2017, once the simulation-based training for the management of SD was introduced. As a result, we do not have data for the cases of SD or other forms of obstetric trauma in the hospital between 2008 and 2016, which precluded us from calculating the incidence of complications associated with SD in that period and comparing it with the incidence recorded after the introduction of the training (from 2017 on). Similarly, we ought to highlight that we were also unable to recover the clavicle and humerus fractures that occurred in the 2008–2016 period, although these fractures are not always associated with SD.
The absence of these data (prior to 2017) is itself a relevant result, as it evinces the previous lack of awareness of this obstetric emergency and the need for a formal register of SD to be able to understand what we are facing in clinical practice. This is the reason that our group started a register of the obstetric care provided in our hospitals and the adverse events that occur, so that reliable data will be available in the future, as there is currently nothing of this nature in Spain.
However, we were able to find records on the most severe cases of OBPP that required referral for management in the 2008–2016 period, which allowed us to make comparisons with care delivery from 2017. The identification, follow-up and referral of patients with severe OBPP has not changed since 2007, nor has the referral hospital that these patients are sent to, so we are fairly confident that we identified all cases of severe OBPP in both periods.
Other limitation of the study is that we did not do a follow-up of the skills acquired by staff in the training, and therefore we could not establish the extent to which they were retained over time. The study by Draycott et al. and the PROMPT team determined that skills were retained between 6 and 12 months,25 but this is an aspect that needs to be evaluated in our setting. We also do not know how the suspension of trainings caused by the COVID-19 pandemic may have affected these skills.
Based on our findings and evidence published by teams from different parts of the world, such as the United States (Dallas), Australia (Victoria) or the United Kingdom (Bristol), it seems that multi-professional clinical simulation is a useful tool to reduce obstetric morbidity associated with SD17,19,25 and that further studies in Spain are not required to recommend the generalised implementation of this type of training.
Simple training programmes that address manual clinical skills delivered by experienced personnel with local resources and low-fidelity simulation (the approach used in PROMPT) are the key to success in reducing the incidence of obstetric brachial plexus palsy.
ConclusionAlthough we did not have reliable data predating the introduction of the training, our findings indicate that there was a reduction in the incidence of complications associated with SD with the implementation of the training programme, as there was a decrease of nearly 90% in the incidence of OBPP comparing the 2017−2018 period (the first years training was offered) to the 2019−2020 period (when most of the clinical staff had participated in at least one training), in addition to a complete absence of permanent cases of OBPP after the implementation of the programme (from 2017 on), in contrast to what had been documented in the past (2008–2016). This local evidence, combined with evidence from other countries, seems sufficient to encourage the creation of registers for the systematic documentation of obstetric emergencies and the implementation of local simulation-based workshops on their resolution with the aim of determining the current morbidity in delivery rooms in Spain and providing safer care.
Conflicts of interestThe authors have no conflicts of interest to declare.
Rita Salvador López, Sara Cruz Melguizo, Amelia Sanz Lorenzana, Gema Iglesias Escalera, Ana Malalana Martínez, Blanca Diez de los Ríos Quintanero, María Luisa de la Cruz Conty, Begoña Encinas Pardilla and Oscar Martínez Pérez.