To study the correlation between the levels of environmental pollutants and the number of paediatric consultations related to respiratory disease in Primary Health Care.
Patients and methodsAn ecological study is performed, in which the dependent variable analysed was the number of paediatric consultations in an urban Primary Health Care centre in Madrid over a 3 year period (2013–2015), and specifically the consultations related to bronchiolitis, recurrent bronchospasm, and upper respiratory diseases. The independent variables analysed were the levels of environmental pollutants. Coefficients of correlation and multiple lineal regressions were calculated. An analysis has been carried out comparing the average of paediatric consultations when the levels of nitrogen dioxide (NO2) were higher and lower than 40μg/m3.
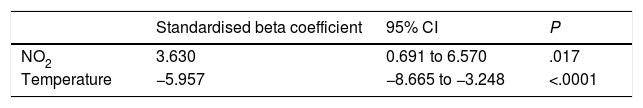
ResultsDuring the period of the study, there were a total of 52,322 paediatric consultations in the health centre, of which 6,473 (12.37%) were related to respiratory diseases. A positive correlation was found between SO2, CO, NOx and NO2 and benzene levels and paediatric consultations related to respiratory diseases, and a negative correlation with temperature. The number of consultations was significantly higher when NO2 levels exceeded 40μg/m3. In the multiple lineal regression (P=.0001), the correlation was only positive between consultations and NO2 levels (3.630, 95% CI: 0.691–6.570), and negative with temperature (−5.957, 95% CI: −8.665 to −3.248).
ConclusionsNO2 environmental pollution is related to an increase in respiratory diseases in children. Paediatricians should contribute to promote an improvement in urban air quality as a significant preventive measure.
Estudiar la relación existente entre los niveles de contaminantes ambientales y la demanda por enfermedad respiratoria en las consultas pediátricas de Atención Primaria.
Pacientes y métodosEstudio ecológico en el que la variable dependiente analizada ha sido la demanda en las consultas pediátricas de un centro de salud urbano de Madrid durante 3 años (2013-2015) por bronquiolitis, episodios de broncoespasmo y procesos respiratorios de vías altas. Como variables independientes se estudiaron los valores de contaminación ambiental. Se calcularon coeficientes de correlación y regresión lineal múltiple. Se comparó el promedio de consultas cuando los valores de dióxido de nitrógeno (NO2) eran superiores e inferiores a 40μg/m3.
ResultadosDurante el periodo de tiempo estudiado hubo un total de 52.322 consultas pediátricas en el centro de salud, de las cuales 6.473 (12,37%) lo fueron por procesos respiratorios. Se encontró correlación positiva entre los niveles de SO2, CO, NO2, NOx, benceno y el número de consultas por procesos respiratorios y negativa con la temperatura y el O3. El número de consultas por enfermedad respiratoria fue significativamente mayor cuando los niveles de NO2 superaban los 40μg/m3. En la regresión lineal múltiple (p<0,0001) solo se mantuvo la relación positiva de las consultas con los niveles de NO2 (3,630; IC 95%: 0,691-6,570) y negativa con la temperatura (−5,957; IC 95%: −8,665 a −3,248).
ConclusionesLa contaminación ambiental por NO2 está relacionada con el aumento de la enfermedad respiratoria en la infancia. Los pediatras deberíamos contribuir a propiciar la mejora de la calidad del aire como una importante medida preventiva.
The World Health Organization (WHO) has been warning for years of the deleterious effects of environmental pollution on human health.1 Global climate change is an indisputable fact, and human activity (industrial, commercial, residential, etc.) is a significant contributor to this change.2 International organisations such as the European Environment Agency disseminate data periodically and warn that southern Europe will be one of the regions that will be most affected by the consequences of climate change.3 Environmental factors and weather are determinants of the health of living organisms,4–6 so it is exceedingly worrisome that seasons that used to be cold are now warm, that air quality regulations are often overlooked,7,8 that a high percentage of vehicles in circulation are highly polluting and, ultimately, that pollution in cities has become the subject of press and broadcast news headlines.9
The paediatric population is particularly vulnerable to environmental conditions10 due to social factors, as children spend long periods of time outdoors and are thus significantly exposed to pollution. Furthermore, they have distinct anatomical and physiological characteristics, and poorly developed defence mechanisms. More specifically, their respiratory tract and immune system are immature, the calibre of their airways is smaller and their respiratory rate greater compared to adults, so they inhale larger volumes of air per kilogram of body weight, all of which amplifies the effects of pollutants in their bodies and overwhelms their capacity to neutralise and eliminate these environmental pollutants. Despite the importance of this issue, few studies have analysed the impact on children's health11 of exposure to high levels of pollutants, such as particulate matter smaller than 2.5microns (PM2.5) and 10microns (PM10), nitrogen dioxide (NO2), nitric oxide (NO), ozone (O3), carbon monoxide (CO), sulphur dioxide (SO2), hydrocarbons such as benzene or nonmethane hydrocarbons (NMHCs).12
Considering the importance of air quality in our health and the considerable economic burden of the care provided for pollution-related diseases, we aimed to analyse the impact of environmental pollution in the number of paediatric primary care (PC) visits due to upper respiratory tract infections, bronchospasm and bronchiolitis.
Patients and methodsWe conducted an ecological study in which we analysed data obtained from the software applications Seguimiento de Objetivos de Atención Primaria (Primary Care Objectives Followup [e-SOAP]) and Consult@web. These applications are available in the digital network available to PC professionals in the Community of Madrid and allow access to patient health records. The indicators we consulted through e-SOAP provided us with information regarding the population served and health care delivery, that is, the monthly number of visits and number of patient consultations per provider per day at different points in time. Consult@web is an online platform that allows health professionals to access the medical records of patients. The data we retrieved from Consult@web referred to upper respiratory tract infection, bronchiolitis and bronchospasm episodes documented in the electronic health records. We searched both databases to retrieve information on the care delivered to the catchment population of 3 paediatrics clinics in a primary care centre in the centre of the city of Madrid between January 1, 2013 and December 31, 2015. We obtained the data pertaining to environmental pollution from the website of the City Council of Madrid13 (Department of Environment and Transportation), Directorate General of Sustainability and Transportation Planning, Department of Air Protection. We collected data for the levels of the following pollutants in the months under study: NO2, NO, PM2.5 and PM10, O3, CO, benzene, SO2, methane (CH4), NMHCs and temperature.
We performed the statistical analysis of the data with the software SPSS version 15.0. We summarised the basic data, expressed as mean and standard deviations in case of quantitative variables and as absolute frequencies and percentages in case of qualitative variables. We calculated 95% confidence intervals (CIs).
We compared quantitative variables by means of the Mann–Whitney U test after checking the normality assumption with the Kolmogorov–Smirnov test. We compared qualitative variables by means of the chi square test. We defined statistical significance as a P-value of less than .05 in any of the tests.
We compared all the quantitative variables under study, calculating the Spearman correlation coefficient.
Subsequently, we performed a multivariate analysis by means of multiple linear regression, starting with the full model and with backward elimination of variables that were not statistically significant (P<.05).
ResultsDuring the period under study, the primary care centre received a total of 52,322 paediatric visits. Of these, 6473 (12.37%) corresponded to respiratory problems. The reasons for the visits due to respiratory problems were bronchiolitis in 827 visits, upper respiratory tract disease in 5125 and bronchospasm episodes in 521. The age of the patients ranged from 0 to 14 years, with a mean of 4.31 years, a standard deviation (SD) of 2.97 and a median of 3. The mean annual temperature in the years under study was: 15.93°C in 2013 (SD, 7.84), with a maximum of 28.10°C in June and a minimum of 6.8°C in January; 16.95°C in 2014 (SD, 9.94), with a maximum of 26.9°C in August and a minimum of 8°C in February; 16.98°C in 2015 (SD, 7.56), with a maximum of 30°C in June and a minimum of 6.9°C in January.
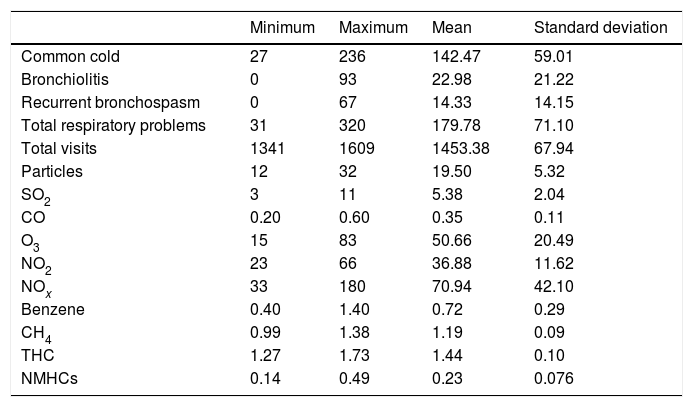
Table 1 shows the descriptive analysis of the variables under study. The mean number of visits per month was 1453.38. There was significant variation between months in the number of visits and level of pollutants (as evinced by the difference between the maximum and minimum values in all of these variables).
Descriptive statistics.
| Minimum | Maximum | Mean | Standard deviation | |
|---|---|---|---|---|
| Common cold | 27 | 236 | 142.47 | 59.01 |
| Bronchiolitis | 0 | 93 | 22.98 | 21.22 |
| Recurrent bronchospasm | 0 | 67 | 14.33 | 14.15 |
| Total respiratory problems | 31 | 320 | 179.78 | 71.10 |
| Total visits | 1341 | 1609 | 1453.38 | 67.94 |
| Particles | 12 | 32 | 19.50 | 5.32 |
| SO2 | 3 | 11 | 5.38 | 2.04 |
| CO | 0.20 | 0.60 | 0.35 | 0.11 |
| O3 | 15 | 83 | 50.66 | 20.49 |
| NO2 | 23 | 66 | 36.88 | 11.62 |
| NOx | 33 | 180 | 70.94 | 42.10 |
| Benzene | 0.40 | 1.40 | 0.72 | 0.29 |
| CH4 | 0.99 | 1.38 | 1.19 | 0.09 |
| THC | 1.27 | 1.73 | 1.44 | 0.10 |
| NMHCs | 0.14 | 0.49 | 0.23 | 0.076 |
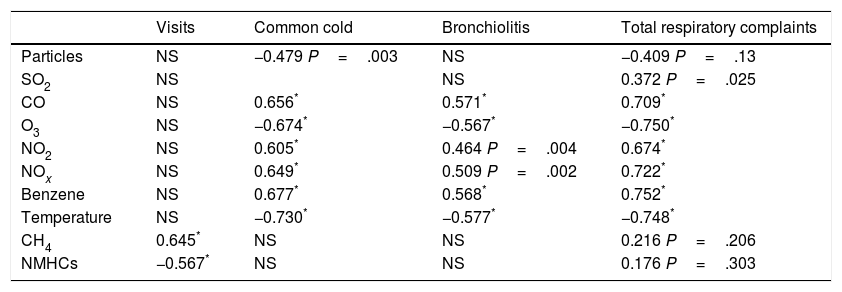
Table 2 presents the Spearman correlation coefficients obtained in the analysis. The number of visits due to respiratory problems was the variable for which we found a significant correlation with temperature and all the environmental pollutant variables under study. The total number of visits was the variable with the fewest significant correlations with specific pollutants.
Spearman correlation coefficients for the comparison of the variables under study (showing only those for statistically significant correlations).
| Visits | Common cold | Bronchiolitis | Total respiratory complaints | |
|---|---|---|---|---|
| Particles | NS | −0.479 P=.003 | NS | −0.409 P=.13 |
| SO2 | NS | NS | 0.372 P=.025 | |
| CO | NS | 0.656* | 0.571* | 0.709* |
| O3 | NS | −0.674* | −0.567* | −0.750* |
| NO2 | NS | 0.605* | 0.464 P=.004 | 0.674* |
| NOx | NS | 0.649* | 0.509 P=.002 | 0.722* |
| Benzene | NS | 0.677* | 0.568* | 0.752* |
| Temperature | NS | −0.730* | −0.577* | −0.748* |
| CH4 | 0.645* | NS | NS | 0.216 P=.206 |
| NMHCs | −0.567* | NS | NS | 0.176 P=.303 |
NS: not significant.
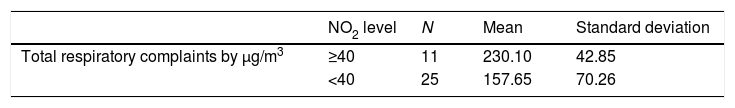
When we analysed the impact of NO2 levels greater than 40μg/m3, we found that the number of visits due to respiratory problems was significantly greater in months in which levels exceeded this threshold, as can be seen in Table 3 (the months with NO2 levels >40μg/m3 were: December and October in all 3 years under study, January and November in 2 years, and March in 1 year).
Table 4 shows the beta coefficients with their corresponding 95% confidence intervals, P-values and coefficients of determination (R2) of the multiple regression model of the visits due to respiratory disease.
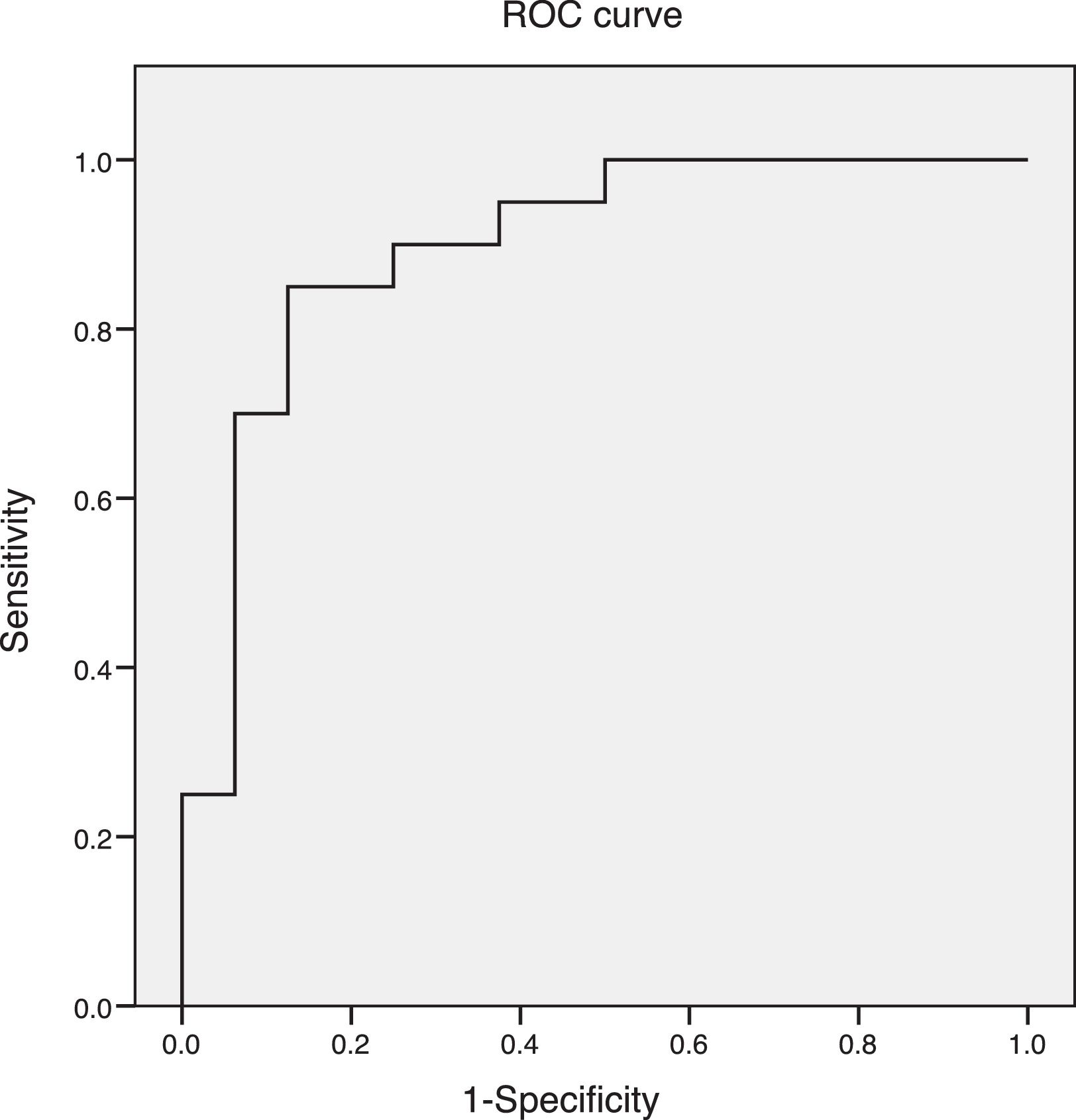
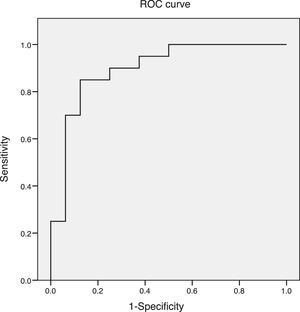
Fig. 1 shows the ROC curve of the values obtained through multiple linear regression of the number of visits for respiratory problems exceeding the monthly average in our study.
DiscussionEnvironmental pollution refers to the presence in the air we breathe of a variety of chemical and biological components that are particularly deleterious to our health. The updated State of Global Air/2017,14 a special report on global exposure to air pollution, and other evidence gathered to date suggests that environmental pollution has contributed to the increase in the incidence of respiratory disease in children, among other problems.15 The WHO has established cut-off points for the level of each pollutant above which they pose a hazard to human health. The group Ecologistas en Acción16 has been producing an annual report since 2000 that includes data for the administrative subdivisions of the Community of Madrid established for the purpose of issuing NO2 alerts. In a recent study, Ortiz et al.17 presented updated data from 52 provinces in Spain on the fraction of mortality attributable to air pollutants, more specifically to particulate matter. In our study, the NO2 levels recorded in the air quality monitoring stations reached maximums of up to 66μg/m3, which exceed the annual maximum of 40μg/m3 considered acceptable by the WHO; we also found a strong correlation between NO2 levels (Table 3) and the number of visits due to bronchiolitis and upper respiratory tract infections. In Spain, levels of air pollutants have been recorded for only a few years, and our study also found a positive correlation between the levels of SO2, CO, NOx and benzene and the incidence of respiratory disease.
In the reviewed literature on this subject, Karr et al.18–20 concluded that infants exposed to high levels of NO2 in air are at higher risk of bronchiolitis; also, taking into account that vehicle emissions, especially from diesel vehicles, are the main source of NO2 in cities, some studies have also demonstrated an association between asthma exacerbations and levels of ground traffic.21–23 Mohamed et al.24 investigated the role of NO in the development of severe bronchiolitis requiring hospital admission. Our results were also statistically significant when it came to NO.
Overall, studies conducted in large cities such as Paris,25 London,26 Santiago de Chile27,28 and Ho Chi Minh (Vietnam)29 have found an association between climate-related factors and environmental pollution (as well as the presence of specific pollutants) and an increased risk of severe bronchiolitis. We did not find a significant association between respiratory diseases and the levels of PM2.5 and PM10. A study conducted in various cities in Brazil30 found an association between increasing levels of O3 and the increase in the incidence of respiratory infections in the paediatric population. In our study, we did not find a correlation with O3.
A study by Martinez31 found an association between exposure to high levels of pollutants in the early years of life and the development of chronic obstructive pulmonary disease many years later.
The magnitude of these effects becomes significant when we take into account that they affect a large number of children, since these risks are omnipresent.
The negative correlation of temperature with respiratory diseases evinced by linear regression is probably due to the fact that low temperatures facilitate transmission of certain viruses, including those that cause bronchiolitis, whose outbreaks occur in wintertime. Environmental pollution, like respiratory disease, exhibits seasonal trends. Two main factors contribute to pollution in large cities. The first one is traffic, which is essential, and whose levels are higher during the school year and are influenced by the economy (for instance, in Madrid, where we conducted our study, traffic decreased by 3% in the worst years of the economic crisis).32 The second factor that contributes to pollution is heating, as many heating systems involve the use of gas oil, gas or coal, which are predictably used most frequently in the winter or cold seasons. In other words, there is a seasonal component in pollution, too, especially in association with the use of fossil fuels (which corresponds to the levels of NO2 in our study).
Our study has the limitations intrinsic to ecological studies, in which the association between exposure and outcomes is observed in a specific group, which does not allow the identification of individual risk factors. Another limitation is the relatively high age range of the population under study.
Given the scarcity of the literature on the impact of exposure to environmental pollution in the early stages of life and that all the studies we reviewed had been based on the rate of hospital admission due to bronchiolitis and the records of paediatric emergency departments, our study contributes a new perspective by reporting data from PC clinics, where the majority of cases of bronchiolitis and upper respiratory infections in children, which usually resolve with outpatient care, are diagnosed and managed.
In conclusion, our findings corroborate the association between environmental pollution and the demand for health care related to respiratory disease in the paediatric population.
We believe that it would be useful to conduct new studies on this subject, and that it is essential to promote measures to regulate ground traffic in large cities while encouraging the use of public transportation, bicycle riding and walking. We also feel compelled to emphasise the need to establish strict regulatory policies to guarantee the quality of the air that we breathe.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martín Martín R, Sánchez Bayle M. Impacto de la contaminación ambiental en las consultas pediátricas de Atención Primaria: estudio ecológico. An Pediatr (Barc). 2018;89:80–85.