Urban air pollution (UAP) is one of the main environmental health (EH) challenges in paediatrics in our era, and possibly the most neglected one. Indoor air quality has been improving while outdoor air quality has worsened as a result of the expansion of megacities (motor vehicles and residential use of fossil fuels), the globalization of industry, power plant activity, intensive farming and waste production. The mortality attributable to UAP has been increasing worldwide since 1990, especially in rapidly developing countries.
UAP caused the premature death of 6.4 million people worldwide in 2015, including 400000 in Europe and 23000 in Spain. Pollution is responsible for 19% of deaths due to cardiovascular disease (24% of cardiac arrests), 21% of deaths due to stroke, 51% of deaths due to chronic obstructive pulmonary disease and 23% of lung cancers. Seventy percent of deaths result from non-notifiable diseases.1,2
Many preventable diseases that are caused by UAP in adults start asymptomatically in the first two decades of life. Children are more vulnerable to UAP because they breathe larger volumes of air per kilogram of body weight than adults due to the immaturity of their developing lung parenchyma and their shorter stature. One percent of the deaths associated with acute respiratory tract infections in children can be attributed to UAP. It can have an adverse impact on pregnancy outcomes before conception (gametogenesis) and during gestation (via the transplacental route, resulting in preterm birth and low birth weight) and is associated with increased perinatal morbidity and mortality.1
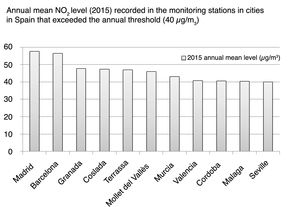
The World Health Organization (WHO) periodically publishes air quality guidelines that constitute the main reference for establishing global standards. The last update is from 2006, and the next one is planned for 2018.3 The WHO also offers data on air quality in more than 3000 cities in 103 countries (http://breathelife2030.org/). This is a powerful tool for adequate surveillance and for the development of models to improve air quality in our countries. In 2015, half of the population in Spain was exposed to levels of air pollutants in excess of European standards (14.7% to nitrogen oxides and 31.5% to ozone).2Fig. 1 shows the Spanish cities whose monitoring stations have exceeded the European annual mean NO2 level threshold.
Annual mean NO2 levels (2015) recorded by monitoring stations throughout cities in Spain that exceeded the annual mean level threshold.2 In many monitoring stations in Madrid and Barcelona, levels exceeded the annual mean level threshold.
Scientific associations and societies must advocate cleaner air for children. The Spanish Association of Paediatrics (AEP in spanish) recently promoted the institution of the EH Committee, and UAP constitutes one of the 7 main challenges identified in the pursuit of improved EH in Spanish children and adolescents (climate change, pollution [air and soil], desertification–deforestation, legal and illegal drugs, drinking water quality, limited exposure to nature, and sea and ocean health).
All components of UAP have adverse effects on health, although particulate matter smaller than 2.5μm and nitrogen oxides have been studied most extensively and have been associated with increased morbidity and mortality in individuals with acute and chronic diseases, especially respiratory diseases (in children, with an increased incidence of coughing, nasal discharge, expectoration and wheezing, increased incidence and severity of lower respiratory tract infections and asthma exacerbations, and loss of pulmonary function; in adults, with an increased incidence of chronic obstructive pulmonary disease and lung cancer), cardiovascular diseases (arrhythmias, congestive heart failure, hypertension and acute myocardial infarction) and neurologic diseases (in children, cognitive impairment, attention-deficit hyperactivity disorder and autism, and in adults, cerebrovascular events and neurodegenerative diseases). There is also evidence of their association with dyslipidaemia, atherosclerosis, endothelial dysfunction and changes in blood coagulation. Emerging evidence suggests a causal relationship with diabetes mediated by oxidative stress, which promotes insulin resistance.1
Simple and easily reproducible methods were used in the work of Martin-Martin and Sanchez-Bayle in the city of Madrid, and found that the incidence of respiratory diseases increased with increasing NO2 levels.4
The good news is that UAP can be controlled, preventing the diseases that it causes. Many countries and cities have achieved successful results with feasible and affordable measures. Among such effective and powerful measures are: (a) the enactment of air quality standards; (b) the reduction of emissions from coal-fired power plants and other sources of combustion/waste-to-energy solutions and mandated transitioning to cleaner fuels; (c) promotion of renewable energies; (d) ban on the use of petroleum products in urban centres; (e) improved access to public transportation; (f) fuel efficiency standards for automobiles, trucks and buses; and (g) Urban access restrictions for private vehicles.
Urban planning initiatives to increase green spaces, improve walkability (widening of sidewalks) and bicycle transit (building bicycle lanes, public bicycle rental programmes) and create car-free shopping districts are other strategies that are aesthetically pleasing, clean and inexpensive. In addition to decreasing UAP, they promote aerobic exercise and therefore reduce the risk of obesity, cancer, diabetes and cardiovascular disease.
As paediatricians, we have a scientific and ethical capability to get involved in defense of community-based EH for numerous reasons: (a) we understand the particular anatomical and physiological vulnerability of children and adolescents to environmental risk factors; (b) we diagnose environmental diseases; (c) we contribute to the prevention of chronic diseases in adulthood; and (d) ultimately, we are the professionals entrusted with the education of parents and society regarding the impact of UAP in the health of their children. Thus, we have significant work ahead of us in multiple areas: (1) leading the creation of multidisciplinary paediatric EH teams; (2) advocating for the individual and collective adoption in our work settings of exemplary measures to decrease UAP; and (3) promoting methodologically appropriate research to assess the impact of UAP on health to help improve policy decisions that impact children. Therefore, we welcome the work of Martín-Martín and Sánchez-Fraile and would like to reinforce it by urging for the promotion of these type of studies and their extension to all other neighbourhoods and cities in Spain.
A global reduction of UAP will require courageous leadership, additional and substantial resources from the international community and wide-ranging social changes. In addition to the aforementioned changes in cities, countries will need to favour a cleaner and more sustainable circular economy model, distancing themselves from the economic growth model based on the “culture of waste,” which requires intensive use of resources. These changes will not be easy. Countries will have to overcome the opposition of powerful lobbies. But thankfully, the technological advances, the policies and institutions required to control air pollution are currently accessible. Models have been developed and their efficacy tested in countries at every level of development.
The growing social awareness of the relationship between health and environment is the main driving force of change. The cooperation of government, community and the collective of health professionals that work with the paediatric population can constitute a powerful tool to control air pollution and improve the health of children and youth.
Please cite this article as: Ortega-García JA, Sánchez-Solís M, Ferrís-Tortajada J. Contaminación atmosférica y salud de los niños. An Pediatr (Barc). 2018;89:77–79.