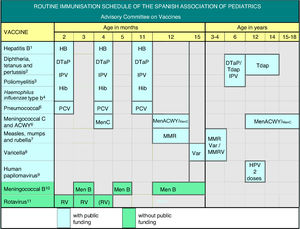
The Advisory Committee on Vaccines of the Spanish Association of Paediatrics annually publishes the immunisation schedule considered optimal for children resident in Spain, according to available evidence on current vaccines.
As regards funded immunisations, the 2+1 strategy (2, 4, 11 months) with hexavalent (DTPa-IPV-Hib-HB) and 13-valent pneumococcal vaccines are recommended.
Administration of the 6-year booster dose with DTPa is recommended, with a poliomyelitis dose for children who had received the 2+1 scheme, as well as Tdap vaccine for adolescents and pregnant women in every pregnancy between 27 and 32 weeks gestation.
The 2-dose scheme should be used for MMR (12 months and 3–4 years) and varicella (15 months and 3–4 years). MMRV vaccine could be applied as the second dose.
Vaccination against HPV is recommended in both genders, preferably at 12 years of age. A stronger effort should be made to improve vaccination coverage. The new 9-valent vaccine is now available, expanding the coverage for both genders.
Tetravalent meningococcal vaccine (MenACWY) is recommended at 12 months and 12-14 years, with a catch-up up at 19 years of age. It is also recommended in infants older than 6 weeks of age with risk factors, or travellers to countries with high incidence of ACWY meningococcal serogroups.
As regards non-funded immunisations, meningococcal B vaccination is recommended, with a 2+1 schedule, and requests that it be included in the National Immunisation Programme. Vaccination against rotavirus is recommended in all infants.
El Comité Asesor de Vacunas de la Asociación Española de Pediatría publica anualmente el calendario de vacunaciones que estima idóneo para los niños residentes en España, teniendo en cuenta la evidencia disponible.
En cuanto a las vacunas financiadas, se recomienda emplear el esquema 2+1 (2, 4 y 11 meses) con vacunas hexavalentes (DTPa-VPI-Hib-HB) y con antineumocócica conjugada 13-valente.
Se aconseja un refuerzo a los 6 años, preferentemente con DTPa, junto con una dosis de polio para aquellos que recibieron esquemas 2+1, así como vacunación con Tdpa en adolescentes y en cada embarazo, entre la semana 27 y la 32.
Se emplearán esquemas de 2 dosis para triple vírica (12 meses y 3-4 años) y varicela (15 meses y 3-4 años). La segunda dosis se podría aplicar como vacuna tetravírica.
Se recomienda vacunación sistemática universal frente al VPH, tanto a chicas como a chicos, preferentemente a los 12 años, debiéndose realizar un mayor esfuerzo para mejorar las coberturas. La nueva vacuna de 9 genotipos amplía la cobertura para ambos sexos.
Se recomienda que la vacuna antimeningocócica conjugada tetravalente (MenACWY) se introduzca en el calendario financiado a los 12 meses y a los 12-14 años, aconsejándose un rescate hasta los 19 años. Igualmente, se recomienda en los mayores de 6 semanas de edad con factores de riesgo o que viajen a países de elevada incidencia de estos serogrupos.
Respecto a las vacunas no financiadas, se recomienda la antimeningocócica B, con esquema 2+1, solicitando su entrada en el calendario. Es recomendable vacunar a todos los lactantes frente al rotavirus.
The Advisory Committee on Vaccines of the Spanish Association of Paediatrics (CAV-AEP) annually updates its immunisation schedule based on the current evidence (see Fig. 1). Its aim is to promote adherence to official immunisation schedules and to offer health professionals involved in the care of children and adolescents alternatives for catch-up immunisation and for expanding protection with vaccines currently not included in official schedules, always taking into account the specific epidemiological context of Spain and with safety as the key consideration. Table 1 lists the vaccines that are available at present.
(1) Hepatitis B vaccine (HB). 3 doses of hexavalent vaccine at 2, 4 and 11 months of age. Children of HBsAg-positive mothers will also be given one dose of monovalent HB vaccine at birth along with 0.5mL of hepatitis B immune globulin (HBIG), all within 12h of birth. When maternal serological status is unknown, the neonatal dose should be administered and maternal serology tested immediately, and, in case of a positive result, HBIG should be administered to the newborn as soon as possible, and in the first week of life. The administration of 4 doses of HB vaccine is generally acceptable and mandatory in children of HBsAg-positive mothers with birth weights of <2000 g vaccinated from newborns, as the neonatal dose in these cases should not be counted. Unvaccinated children and adolescents should be given three doses of monovalent vaccine or the combined hepatitis A and B vaccine on a 0, 1 and 6 month schedule, at any age.
(2) Diphtheria, tetanus and acellular pertussis vaccine (DTaP/Tdap). 5 doses: primary vaccination with 2 doses, at 2 and 4 months, of DTaP (hexavalent) vaccine; booster at 11 months (third dose) with DTaP (hexavalent) vaccine; at 6 years (fourth dose) with the standard load vaccine (DTaP-IPV), preferable to the low diphtheria and pertussis antigen load vaccine (Tdap-IPV), and at 12–14 years (fifth dose) with Tdap.
(3) Inactivated poliovirus vaccine (IPV). 4 doses: primary vaccination with 2 doses, at 2 and 4 months, and booster doses at 11 months and 6 years.
(4) Haemophilus influenzae type b conjugate vaccine (Hib). 3 doses: primary vaccination at 2 and 4 months and booster dose at 11 months.
(5) Pneumococcal conjugate vaccine (PCV). 3 doses: the first two at 2 and 4 months, with a booster dose starting at 11 months of age. The vaccine recommended in Spain by the CAV-AEP continues to be the PCV13.
(6) Meningococcal C conjugate vaccine (MenC) and meningococcal ACWY conjugate vaccine (MenACWY). One dose of monovalent MenC conjugate vaccine at 4 months of age. MenACWY conjugate vaccine is recommended at 12 months and 12-14 years, and a progressive catch-up vaccination schedule to be completed by age 19 years. Vaccination is still recommended in children and adolescents that are to live in countries where the vaccine is administered at this age, such as the United States, Canada, UK, Austria, Greece, Netherlands, Italy or Switzerland, and for children aged more than 6 weeks travelling to countries with a high incidence of IMD caused by vaccine serogroups or with risk factors for IMD: anatomic or functional asplenia, complement component deficiency, treatment with eculizumab, prior episode of IMD caused by any serogroup, and contacts of an index case of IMD caused by serogroup A, W or Y in the context of an outbreak.
(7) Measles, mumps and rubella vaccine (MMR). 2 doses of measles–mumps–rubella vaccine (MMR). The first at age 12 months and the second at age 3–4 years. The tetravalent MMRV vaccine may be administered for the second dose. Susceptible patients outside the specified ages will be vaccinated with 2 doses of MMR at least 1 month apart.
(8) Varicella vaccine (Var). 2 doses: the first at age 15 months (age 12 months is also acceptable) and the second at age 3–4 years. The tetravalent vaccine (MMRV) may be used for the second dose. Susceptible patients outside the specified ages will be vaccinated with 2 doses of Var at least 1 month apart.
(9) Human papillomavirus vaccine (HPV). Universal routine vaccination of all girls and boys, preferably at age 12 years, to prevent oncological diseases associated with this virus. All 3 HPV vaccines are authorised for use in male individuals, although there is little data on the use of the HPV2 vaccine in this sex. Administration of 2 doses at age 11–12 years. The vaccination schedule depends on the vaccine used: for the tetravalent vaccine, a 2-dose series (at 0 and 6 months) for girls aged 9 to 13 years and a 3-dose series (at 0, 1 and 6 months) in those aged ≥14 years; for the 2-valent and 9-valent vaccines, a 2-dose series (at 0 and 6 months) in girls aged 9–14 years and a 3-dose series (at 0, 1–2 and 6 months) in those aged ≥15 years. The HPV vaccine may be administered at the same time as the MenC, hepatitis A and B and Tdap vaccines. There are no data on its coadministration with the varicella vaccine, although it should not cause any problems.
(10) Meningococcal B vaccine (MenB). 3 doses: if vaccination starts at age 3 months, 2 doses at least 2 months apart with a booster starting at age 12 months and at least 6 months after the last dose in the primary vaccination series. If vaccination starts at 2 months, 4 doses are needed. Administration at least 15 days apart from other injectable inactivated vaccines is recommended up to age 18 months to minimise potential reactogenicity and avoid coadministration with the MenC vaccine conjugated with tetanus toxoid. The separation by a 15-day interval is not necessary for the varicella, MMR and rotavirus vaccines.
(11) Rotavirus vaccine (RV). 2 or 3 doses of rotavirus vaccine: at 2 and 3 months or at 2 and 4 months with the monovalent vaccine or at 2, 3 and 4 months or 2, 4 and 5–6 months with the pentavalent vaccine. It is very important to start vaccination between 6 and 12 weeks of life in order to minimise risks, and to complete it before 24 weeks for the monovalent vaccine or 32 weeks for the pentavalent vaccine. Doses must be given at least 4 weeks apart. Both doses may be given at the same time as any other vaccine.
Acronyms and brand names of vaccines.
| Acronym | Vaccine | Brand name (Laboratory) |
|---|---|---|
| DTaP-IPV-Hib-HB | Hexavalent | Hexyon (Sanofi Pasteur) |
| DTaP-IPV-Hib-HB | Hexavalent | Infanrix hexa (GSK) |
| DTaP-IPV-Hib-HB | Hexavalent | Vaxelis (MSD) |
| DTaP-IPV | Standard load diphtheria, tetanus toxoid, standard load acellular pertussis and injectable poliovirus vaccine | Not distributed in Spain |
| Tdap-IPV | Reduced diphtheria toxoid, tetanus toxoid, reduced load acellular pertussis and injectable poliovirus | Boostrix-polio (GSK) |
| Tdap | Reduced diphtheria toxoid, tetanus toxoid, reduced load acellular pertussis | Boostrix (GSK) |
| Tdap | Reduced diphtheria toxoid, tetanus toxoid, reduced load acellular pertussis | Triaxis (Sanofi Pasteur) |
| PCV10 | Pneumococcal conjugate vaccine, 10 serotypes | Synflorix (GSK) |
| PCV13 | Pneumococcal conjugate vaccine, 13 serotypes | Prevenar 13 (Pfizer) |
| MenC | Meningococcal C conjugated with tetanus toxoid | NeisVac-C (Pfizer) |
| MenACWY | Meningococcal A, C, W and Y conjugated with CRM197 | Menveo (GSK) |
| MenACWY | Meningococcal A, C, W and Y conjugated with tetanus toxoid | Nimenrix (Pfizer) |
| MMR | Measles, mumps, rubella | MMR Vaxpro (MSD) |
| MMR | Measles, mumps, rubella | Priorix (GSK) |
| MMRV | Measles, mumps, rubella and varicella | Priorix tetra (GSK) |
| MMRV | Measles, mumps, rubella and varicella | Proquad (MSD) |
| Var | Varicella | Varilrix (GSK) |
| Var | Varicella | Varivax (MSD) |
| HPV2 | Human papillomavirus 2 genotypes | Cervarix (GSK) |
| HPV4 | Human papillomavirus 4 genotypes | Gardasil (MSD) |
| HPV9 | Human papillomavirus 9 genotypes | Gardasil 9 (MSD) |
| 4CMenB | Meningococcus B | Bexsero (GSK) |
| MenB-FHbp | Meningococcus B | Trumenba (Pfizer) |
| RV | Monovalent rotavirus | Rotarix (GSK) |
| RV | Pentavalent rotavirus | RotaTeq (MSD) |
This year, having already established the 2+1 schedule with hexavalent vaccines for immunisation in the first year of life,1 the main change concerns the vaccination with the MenACWY vaccine, which is now recommended at 12 months and in adolescents.
We recommend consulting the expanded version of this document published online in the CAV-AEP website, which explains in detail the grounds for these recommendations. Furthermore, the recommendations for special situations and risk groups can also be found in the Manual de Vacunas en línea de la AEP (AEP Vaccine Manual online, https://vacunasaep.org/documentos/manual/manual-de-vacunas), most of whose contents were updated in 2018.
While the immunisation schedules of the different autonomous communities (ACs) are quite similar, efforts should be made to establish uniform ages for the administration of the different vaccines throughout Spain.
We also propose working towards the following goals: (1) the design and development of new structures for the investigation and development of immunisation recommendations, supplementing the leadership of the Interterritorial Council of the Spanish National Health System (Consejo Interterritorial del Sistema Nacional de Salud [CISNS]) with the direct contributions of scientific societies and families; (2) for the Spanish National Health System (Sistema Nacional de Salud [SNS]) to consider possible formulas for the shared funding (copays, as done with other medicines) of vaccines not included in the official schedules; (3) and to evaluate and start working on the necessary establishment of a system to compensate for the rare, although possible, damages caused by vaccination.
If we are to avoid the resurgence of vaccine-preventable diseases, we must continue to strive to maintain high vaccination coverage rates, address the gaps in coverage in specific age groups, and adopt a collaborative, holistic and multidisciplinary approach to the persuasion of parents who refuse vaccination or have doubts about it.
Hepatitis B vaccination2019 recommendation:We recommend the vaccination of infants with 3 doses of hexavalent vaccine at 2, 4 and 11 months of age. Previously unvaccinated older children and adolescents will receive 3 doses of the monovalent vaccine in a 0, 1 and 6 months schedule.
In Spain, the annual incidence of hepatitis B remains under 2 cases per 100,000 inhabitants. In 2015, a total of 561 cases of hepatitis B were reported, corresponding to an incidence of 1.21 cases/100,000 inhabitants.2
Since 2018, the primary vaccination series for hepatitis B starts at 2 months of age with the hexavalent vaccine in every autonomous community.
Vaccination at birth should continue to be performed in newborns of mothers who are HBsAg positive or of unknown serological status, regardless of birth weight, always with the monovalent vaccine. Newborns of HBsAg-positive mothers should also be given hepatitis B immune globulin in the first 12h of life. In newborns of mothers unknown status, administration of immune globulin can be delayed for a maximum of 1 week while awaiting the results of maternal serological testing. In cases where a neonatal dose is given, the complete series will consist of 4 doses.
Diphteria, Tetanus, Pertussis, Poliomyelitis and Haemophilus influenzae type b vaccination2019 recommendation: We recommend a 2+1 schedule with the hexavalent vaccine at 2, 4 and 11 months. Children that have received the 2+1 series should be given DTaP-IPV, preferably, or Tdap-IPV at age 6 years and Tdap at age 12–14 years. We recommend vaccination with Tdap of all pregnant women in each pregnancy between 27 and 32 weeks of gestation, as early as possible within this interval.
Despite vaccination, the incidence of pertussis has been increasing worldwide. Infants aged less than 3 months are most vulnerable and are the main group that needs protection.3
Vaccination of pregnant women with Tdap in each gestation is safe, efficacious and the most effective and efficient means of preventing pertussis in infants.4 Vaccination in the second trimester of gestation increases antibody levels in infants, widens the immunisation opportunity window and confers protection to preterm newborns.5 Countries such as the United Kingdom recommend administration of the vaccine starting at 20 weeks’ gestation.6
There is evidence in the literature of a potential maternal antibody interference with the immune response to various vaccine antigens in infants of mothers vaccinated against pertussis during pregnancy,7 with the immune response usually normalising after administration of the booster dose, and no evidence up to date of an association of this phenomenon with a negative impact in epidemiology.8
The 2+1 schedule is used in many European countries, it is sufficiently immunogenic and optimises the use of available doses. Early administration of the first dose at 6 weeks post birth is acceptable.
Children that received a 2+1 primary vaccination series with hexavalent vaccine as infants must receive a polio booster at age 6 years, preferably with the DTaP-IPV vaccine.
Infants vaccinated with a 2+1 schedule of hexavalent vaccine must receive a booster at age 6 years, preferably with DTaP combined with a component against polio (DTaP-IPV).
Pneumococcal vaccination2019 recommendation:Vaccination against pneumococcal disease is recommended for all children younger than 5 years and children that are at risk due to underlying disease at any age. A 2+1 series (2, 4 and 11–15 months) is recommended for routine vaccination of infants. On account of the current epidemiology of pneumococcal infections in Spain, the CAV-AEP continues to recommend the use of the 13-valent pneumococcal conjugate vaccine (PCV13).
The evidence on the reduction in the burden of invasive pneumococcal disease (IPD) and non-invasive pneumococcal disease (pneumonia and acute otitis media) continues to grow; this effect is due not only to the direct protection of vaccinated individuals, but also, and to a greater extent, to the indirect protection of unvaccinated children and adults. While the reduction in IPD has been close to the estimations of efficacy studies, the reduction in the incidence of pneumonia and otitis media has exceeded expectations.
The ultimate impact of a vaccine depends to a great extent on its coverage of the serotypes circulating in a given area, and its potential to produce herd immunity against specific serotypes. The CAV-AEP considers that the PCV-13 vaccine is the one that offers the best coverage against the serotypes circulating in Spain. After the introduction of the PCV-13 vaccine in the immunisation schedule of Madrid, there have been decreases of 68% in the incidence of IPD by any serotype and 93% in the incidence of IPD by vaccine serotypes.9 Considering the incidence in all age groups, the reductions have been of 33% and 75%.10
The emergence of non-vaccine serotypes after the introduction of the PCV-10 and PCV-13 vaccines has varied between countries.11–15 In Madrid, there has been no increase in the incidence of disease by these serotypes in children aged less than 15 years,9 but analysing every age group, there have been increases in some serotypes, such as 8, 9N, 10A, 23B, 24F and 33.10 Most countries using the PCV-10 vaccine have experienced an increase in the incidence of cases of IPD by non-vaccine serotypes, especially 19A.13–15
Meningococcal A, C, W and Y vaccination2019 recommendation:We continue to recommend vaccination against meningococcus C at 4 months. Due to the increasing incidence of disease by serogroups W and Y in Spain, the CAV-AEP recommends vaccinating at 12 months of age and adolescents by the introduction in the routine immunisation schedule of the tetravalent meningococcal conjugate vaccine (MenACWY), with progressive catchup of unvaccinated individuals through age 19 years. Vaccination is also recommended in children aged more than 6 weeks with risk factors for invasive meningococcal disease (IMD) or travelling to endemic regions.
There is ample evidence of the effectiveness of the monovalent MenC vaccine. The incidence of IMD by serogroup C in Spain remained very low in the 2016–2017 season (0.06 cases/100,000 inhabitants).
Since 2000, there has been a marked increase in the incidence of IMD by a particularly virulent serotype of serogroup W (ST-11CC) in several countries throughout the world.16 This has prompted the inclusion of the MenACWY vaccine in the immunisation schedules of several countries in Europe, such as the United Kingdom, Austria, Greece, the Netherlands and Italy, and in America, such as United States, Canada, Chile and Argentina.
Since 2015, the United Kingdom has replaced the MenC dose administered at age 12 years by a dose of MenACWY at age 14 years, with catchup vaccination in older adolescents. Although vaccine coverage rates have not reached 90%,17 there has been a significant reduction in the cases by serogroup W compared to the expected frequency.18
In Spain, there has been a progressive increase in IMD caused by serogroups W and Y since 2015. In the 2016–2017 season, there were a total of 17 reported cases by serogroup W and 16 by serogroup Y (incidence, 0.04/100,000 inhabitants). However, the latest data reported to the Centro Nacional de Epidemiología (National Epidemiology Centre) through week 37 of 2018 show a clear increasing trend: 39 cases of IMD by serogroup W (incidence, 0.10/100,000) and 31 by serogroup Y (incidence, 0.08/100,000).19
The sale in pharmacies of two MenACWY vaccines was authorised in Spain in September 2017.20 In light of the current epidemiology of IMD in Spain, the CAV-AEP recommends the use of the MenACWY for routine vaccination of all adolescents and for vaccination of children aged more than 6 months with risk factors for IMD or travelling to regions with a high prevalence of these serogroups.
Due to this epidemiological situation, the inclusion of Men-ACWY vaccination in the routine calendar is recommended at the age of 12 months for individual protection and in adolescents with the intention to act on the population with the highest rate of nasopharyngeal colonisation by meningococcus. A progressive catchup immunization is recommended for unvaccinated adolescents until age 19 years.
In the meanwhile, this Committee recommends continuing using the meningococcal vaccine selected by each autonomous community to obtain optimal coverage. MenC vaccination at 4 months of age is recommended until MenACWY can be administered in a single dose at this age.
Measles, Mumps and Rubella (MMR) vaccination2019 recommendation: We recommend the administration of a first dose of MMR vaccine at 12 months of age, with a second dose given between 3 and 4 years of age. The tetravalent vaccine (MMRV) may be used for the second dose.
The MMRV vaccine carries an increased risk of febrile seizure, especially following the first dose and in children aged less than 2 years, so it is recommended that the MMR and varicella vaccines be administered separately before that age.21
The prevalence of measles in the European Region of the WHO has increased in recent months,22 partly due to suboptimal vaccination coverage in some countries. There are also still outbreaks of mumps. Maintenance of high vaccination coverage rates and rigorous epidemiologic surveillance are essential for the purpose of eradicating these diseases.
One dose at 12 months achieves seroconversion rates of 95% or higher for all three viruses, which reach nearly 100% after the second dose. The second dose is absolutely essential to achieve adequate herd immunity and remedy potential primary vaccine failures.
Varicella vaccination2019 recommendation:We recommend vaccination of all children against varicella with 2 doses administered at ages 15 months and 3–4 years (the second dose with the MMRV vaccine). We also recommend catch-up vaccination with a 2-dose series for all children and adolescents that did not have the disease (or completion of the 2-dose series when applicable).
Since 2016, vaccination against varicella has been included in the immunisation schedule of every AC with a 2-dose series (at 15 months and 3–4 years).1 There are two monovalent and two tetravalent vaccines with evidence of a high effectiveness (92–97.3%) on the vaccinated and the unvaccinated populations,23 and excellent safety profiles.24 In 2018, several ACs introduced the use of the MMRV vaccine for the second dose, which facilitates adherence to the immunisation schedule.
After 20 years of use in the United States, there is evidence of a sustained decline in the incidence of disease, with no shift of disease towards older ages25 or changes in the incidence of herpes zoster,26 a decisive factor in the cost-effectiveness of childhood immunisation against varicella.24
Human Papillomavirus (HPV) vaccination2019 recommendation:Routine vaccination against HPV is recommended in both girls and boys, preferably at age 12 years, as a means to prevent oncological diseases associated with this virus. This measure has been proven to achieve a significant reduction in the burden of disease associated with HPV in both sexes.
The optimal age for vaccination is 12 years, with administration of a 2-dose series, with the aim of maximising immunogenicity and its possible benefits prior to sexual debut and pursuing the broadest possible vaccination coverage. The recommendation also extends to older ages if vaccination has been delayed, given the benefits that it may continue to provide.
In girls, the evidence on the efficacy and effectiveness of this vaccine in preventing persistent HPV infection, genital warts and precancerous cervical lesions continues to grow, with a reduction of up to 85% in the incidence of high-grade dysplasias, even 10 years after vaccination.27
When it comes to male individuals, there is evidence that the efficacy of the vaccine is greater in those that receive it prior to their sexual debut.28 In a few years, data will probably be available on the actual prevention of cervical cancer and other types of cancer associated with HPV.
With more than 300 million doses having been administered worldwide, these vaccines have proven to be safe and to have a very favourable risk–benefit ratio.27 Research has ruled out an association between these vaccines and the development of autoimmune and neurologic diseases.27 Still, the average coverage in Spain continues to be considerably low compared to all other vaccines in the routine immunisation schedule.29 All health professionals must have adequate knowledge of its effectiveness and safety and reinforce the positive messages regarding this vaccine.
Vaccination of male individuals is already included in the schedules of several countries, with the recent addition of Germany and the United Kingdom.30 There are relevant data on the role of HPV in the aetiology of certain types of cancer affecting both sexes but with a higher incidence in males, such as rectal cancer and head and neck cancer.30 For all the above reasons, the CAV-AEP recommends vaccinating male adolescents, preferably starting at age 12 years.
The 9-valent HPV vaccine (6/11/16/18/31/33/45/52/58 [HPV9]) has been available in Spain since 2017.20 It is safe and effective, increases the overall prevention of HPV-related cervical malignancies from 70% to 90% and may also prevent 85% to 95% of HPV-related vulvar, vaginal and anal cancers,31 making it the best available option for both sexes, although this Committee recommends administration of whichever HPV vaccine has been selected by each AC for girls.
Meningococcal B vaccination2019 recommendation:This vaccine exhibits the profile of a routine vaccine to be administered to all children starting at 3 months of age with a 2+1 schedule. For the rest of the paediatric population, including adolescents, the CAV-AEP advocates for vaccination on a case-by-case basis.
At present, two vaccines are available for the prevention of IMD by group B meningococcus (MenB): the 4CMenB vaccine and the MenB-FHbp vaccine. Both contain subcapsular protein antigens. Since IMD by serogroup B is rare, conventional cost-benefit analyses of vaccination against MenB are unfavourable. However, given that IMD is a devastating disease and that we have efficacious and safe vaccines at our disposal, the CAV-AEP continues to consider that the 4CMenB exhibits the profile of a routine vaccine to be administered to children aged less than 5 years and especially those aged less than 2 years, the group with the highest incidence of IMD.
In 2015, the United Kingdom introduced the 4CMenB in its official immunisation schedule with a 2+1 series (off-label use). The results of the first 10 months of vaccination showed an effectiveness of 83% against all serotypes of MenB and 94.6% against vaccine serotypes, with a reduction of 50% in the incidence of disease in the target population.32 In the second year since its introduction, the overall incidence of IMD by MenB decreased by 11%. In the 2016–2017 period, there were 47 reported cases of IMD by MenB in infants aged less than 1 year, compared to 83 in the 2015–2016 period.33 Andorra, Ireland, Italy and Lithuania have also included the 4CMenB vaccine in their immunisation schedules.
The available data have confirmed that a 2+1 series of 4CMenB is sufficiently immunogenic,34 which led the European Medicines Agency to allow a modification of its summary of product characteristics in 2018, authorising its use from 3 months of age.
Since 2018, the MenB-FHbp vaccine is approved in Europe for administration to individuals from 10 years old. Due to the low incidence of IMD by MenB in the Spanish adolescent population and the lack of evidence of the impact of this vaccine on nasopharyngeal carriage35 (the main epidemiological reason to vaccinate at this age), the CAV-AEP recommends the use of either vaccine in adolescents on a case-by-case basis to optimise individual protection against IMD.
Rotavirus vaccination2019 recommendation:Vaccination against rotavirus (RV) is an advisable health intervention for all infants.
To date, more than 100 countries have included vaccination against RV in their immunisation schedules. The health benefits of this measure have been enormous, with a substantial decrease worldwide in the morbidity and mortality associated with rotavirus gastroenteritis in infants and young children.36
In Europe, vaccination programmes against RV have led to reductions of 60%–90% in the burden of disease in terms of both primary care and hospitalisation.37
The benefits of vaccination extend to both vaccinated infants and, indirectly, to the unvaccinated environment, significantly increasing its public health impact and efficacy.38 It is important to be particularly mindful of preterm infants, who may exceed the vaccination age before discharge from hospital,39 and children infected by HIV, who are at greater risk of developing severe disease due to RV.
The benefits of vaccination vastly exceed the risks of intussusception, the only associated serious adverse effect, which is very rare (between 1 and 5 cases per 100,000 vaccinated children).40
Two RV vaccines are available in pharmacies, a pentavalent and a monovalent vaccine.20
FundingThe development of these recommendations (analysis of the published data, debate, consensus and publication) has not been supported by any funding source outside of the logistic support provided by the AEP.
Conflicts of interest (last 5 years)DMP has collaborated in educational activities funded by Astra, Pfizer, GlaxoSmithKline, Sanofi Pasteur and MSD, as consultant on a GlaxoSmithKline advisory board and as a researcher in clinical trials by Novartis.
FJAG has collaborated in educational activities funded by GlaxoSmithKline, Novartis, Pfizer, Sanofi Pasteur and MSD, and as a consultant on GlaxoSmithKline, Novartis, Pfizer, Sanofi Pasteur and MSD advisory boards.
JAA has collaborated in educational activities funded by Astra, GlaxoSmithKline, Pfizer, Sanofi Pasteur and MSD, as a consultant on GlaxoSmithKline and Pfizer advisory boards, and as a researcher in clinical trials conducted by GSK.
MJCO has collaborated in educational activities funded by GlaxoSmithKline, Novartis, Pfizer, Sanofi Pasteur and MSD, as a researcher in clinical trials conducted by GlaxoSmithKline and Pfizer, and as a consultant on GlaxoSmithKline, Novartis, Pfizer, Sanofi Pasteur and MSD advisory boards.
MGS has collaborated in educational activities funded by Astra, GlaxoSmithKline, Pfizer, Sanofi Pasteur and MSD, as a consultant on GlaxoSmithKline and Novartis advisory boards, and as a researcher in clinical trials conducted by GlaxoSmithKline, Janssen, Sanofi Pasteur and MSD.
NGS has collaborated in educational activities funded by Sanofi Pasteur and MSD, and attended educational activities funded by Novartis and Pfizer.
AHM has received funding to attend domestic educational activities, and has participated in educational activities funded by Pfizer.
MMH has collaborated as a researcher in clinical trials conducted by GlaxoSmithKline, MSD and Novartis.
MMM has collaborated in educational activities funded by GlaxoSmithKline, Pfizer, Sanofi Pasteur and MSD, as a researcher in clinical trials conducted by GlaxoSmithKline, Pfizer, Sanofi Pasteur and MSD, and as a consultant on a Novartis advisory board.
AMM has received funding from Pfizer to attend educational activities in Spain and abroad, but stopped accepting any type of sponsoring from any pharmaceutical laboratories for any type of activity (as an educator or as a learner) since becoming a member of the CAV-AEP.
JRC has collaborated in educational activities funded by GlaxoSmithKline, Pfizer, Sanofi Pasteur and MSD, and as a researcher in clinical trials conducted by GlaxoSmithKline and Pfizer.
We thank Javier Arístegui, Jose María Corretger and Luis Ortigosa, for their inhouse advice in the development and writing of these recommendations.
Please cite this article as: Moreno-Pérez D, Álvarez García FJ, Álvarez Aldeán J, Cilleruelo Ortega MJ, Garcés Sánchez M, García Sánchez N, et al. Calendario de vacunaciones de la Asociación Española de Pediatría: recomendaciones. An Pediatr (Barc). 2019;90:56.