Functional gastrointestinal disorders (FGIDs) are a very common pediatric disease, with strong implications for children and their families. We aimed to determine their frequency in our environment (per Rome IV criteria) and to establish if there is seasonal variability in diagnosis.
MethodsDescriptive, prospective study. For 12 months, children under 16 years of age with suspected FGIDs who had a first pediatric gastroenterology consultation were included and classified according to Rome IV criteria. Statistical analysis was done with SPSS v22.
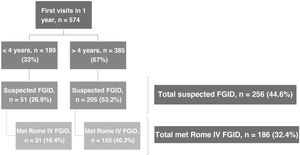
Results574 children received consultations, 67% were >4 years of age. FGIDs were suspected in 44.6% of the patients, 32.4% were diagnosed according to Rome IV criteria (16.4% <4 years, 40.3% >4 years). 51.1% were female, average age of 8.4 ± 4.2 years and mean of 7 months of symptoms until diagnosis (range 3–150). In patients <4 years, the most common disorders were functional constipation (48.4%), regurgitation (22.5%) and functional diarrhea (16.1%); in patients >4 years of age, functional abdominal pain (29%), functional dyspepsia (28.4%) and functional constipation (16.8%) were most frequent. We didn’t discern seasonal variations in diagnosis in the global study population (p = 0.96) or by age group (<4 p = 0.51; >4 p = 0.57).
ConclusionsFGIDs account for one third of our patients’ consultations. While the Rome IV criteria are more inclusive than before, almost 30% of patients with suspected FGIDs don’t meet said criteria. Although a seasonal difference regarding diagnosis was observed, it wasn’t statistically significant either in the sample group as a whole or by age group.
Los trastornos funcionales gastrointestinales (TFGI) son una patología común en pediatría, con fuertes implicaciones para el niño y su familia. Nuestro objetivo es determinar su frecuencia en nuestro medio según criterios Roma IV y la posible variación estacional al diagnóstico.
Material y métodosEstudio descriptivo con recogida de información prospectiva. Durante un año se incluyeron menores de (<) 16 años que acudieron a primera consulta de Gastroenterología Pediátrica con sospecha de TFGI, a los que se clasificó según Roma IV. Análisis estadístico mediante SPSS v22.
ResultadosAcudieron en total 574 niños, 67% mayores de (>) 4 años. Se sospechó TFGI en 44.6%, siendo diagnosticados según criterios Roma IV 32.4% (16.4% <4 años, 40.3% >4 años). 51.1% eran mujeres, edad media de 8.4 ± 4.2 años, y mediana de 7 meses de síntomas al diagnóstico (rango: 3–150). Por frecuencia, en <4 años destacan el estreñimiento (48.4%), la regurgitación (22.5%) y la diarrea funcional (16.1%); y en >4 años el dolor abdominal funcional no especificado (29%), la dispepsia funcional (28.4%) y el estreñimiento (16.8%). En el diagnóstico por trimestres no se objetivaron diferencias en el total (p = 0.96), ni por grupos de edad (<4 p = 0.51; >4 p = 0.57).
ConclusiónSegún Roma IV, los TFGI suponen un tercio de los pacientes de nuestra consulta. A pesar de ser más inclusivos que previamente, casi un 30% de los pacientes con sospecha no cumple criterios. Aunque existe cierta variación estacional en la frecuencia diagnóstica, no fue significativa ni en el total ni por grupos de edad.
Functional gastrointestinal disorders (FGIDs) are symptoms involving the digestive tract that are recurrent and chronic but cannot be explained by structural or biochemical abnormalities.1–5 These diseases are very common in the paediatric age range and are important due to their impact on the quality of life of the patient as well as the family, which translates to an increased use of health care services.3,4,6 They are associated with a poor quality of life, psychological stress and decreased school attendance, physical activity and social life.7,8 Motivated by the absence of objective biological markers that would allow a certain diagnosis, the Rome criteria were first developed2,7 to advance knowledge on these disorders and approach their diagnosis appropriately, avoiding the performance of excessive diagnostic tests, thus helping the patient and the family to accept the diagnosis despite the absence of verifiable organic disease.2,3
The original Rome criteria were published in 1990 and applied exclusively to adults with gastrointestinal (GI) symptoms that could not be explained by an organic disease.3,6 It was not until 1999, when the second version was published, that they addressed FGIDs in paediatric patients independently, despite the scarcity of the literature supporting the proposed criteria.3,6 In 2006, the Rome III criteria were published, and this version was the first that provided a classification by age range (infants and children aged less than 4 years, and children aged 4 or more years) and defined FGIDs based on the presenting symptoms.3 They were followed by the Rome IV criteria, published in 2016, which were based on prevalence studies that applied the Rome III criteria and a more detailed knowledge of the aetiopathogenesis of these disorders.1,3,5–7,9,10 It is this last classification that labelled them as “disorders of gut-brain interaction” involving a myriad of factors, such as genetic predisposition, environmental factors, psychological stress, infections or traumatic events in the early stages of development, personality, regulatory systems, pain thresholds, etc.3,4,8,9,11 There is a bidirectional communication between brain and gut through neuropeptides that plays a key role in the perception of pain and that can also be modified by the autonomic, limbic and endocrine systems.3,8,9,11 In addition, in recent years, the emerging knowledge of the intestinal microbiota suggests that there may be a causal relationship between changes in the microbiota and the development of FGIDs, and there are even references to a “microbiome-gut-brain axis”.11
The Rome IV criteria classify FGIDs based on the presence of GI symptoms and dictate that the diagnosis of these disorders requires an appropriate medical evaluation to determine that the symptoms cannot be attributed to another disease.3,6,9
In children aged less than 4 years, FGIDs are associated with GI, intellectual and affective immaturity and occur in the context of physiological development (infant regurgitation) or as maladaptive responses (constipation in the context of toilet training).3,5,8,9 The diagnosis of FGIDs in this age group relies on parental reporting and interpretation of symptoms, since children this young are unable to express themselves clearly, and it is important to consider the anxiety that symptoms create in parents and caregivers.3–5
A novelty in the Rome IV criteria is the classification of disorders in the group of children aged more than 4 years into 3 broad groups: 1) functional nausea and vomiting disorders, new diagnoses that already existed in the adult classification and that have been found to occur in older children; 2) functional abdominal pain disorders and 3) functional defecation disorders.3,7,9
Since they are a frequent reason for consultation and there hardly any studies have been conducted in Spain to assess their frequency in children, our aim was to determine the frequency of FGIDs in our region applying the new Rome IV criteria and determine whether there is seasonal variation in the time of diagnosis. As a secondary objective, we analysed the diagnostic tests and treatments used at the primary care (PC) and speciality care (SC) levels.
Material and methodsWe conducted a prospective descriptive study with the primary objective of establishing the frequency of FGIDs in the caseload of a paediatric gastroenterology clinic of a secondary level hospital in the Community of Madrid, Spain.
The study included every patient with possible FGID who underwent an initial evaluation in the paediatric gastroenterology clinic in a period of 12 months (September 2018 to August 2019). We collected epidemiological, clinical and demographic data through history-taking and completion by parents of a demographic data form at the clinic. The gastroenterologist in charge of the patient classified the disorder based on the Rome IV criteria for the applicable age group (<4 years and >4 years).
The study variables were sex, trimester of the year when the initial evaluation took place, the duration of symptoms, diagnostic tests, treatments and clinical setting (PC or SP).
We analysed the collected data with the software IBM SPSS Statistics® version 22 for Windows. In the descriptive analysis, we obtained frequencies, percentages (absolute and cumulative), mode and range for nominal variables, and the mean and standard deviation (SD) or median and interquartile range for ordinal variables, depending on their distribution. We assessed the normality of the distribution by means of the Kolmogorov–Smirnov test, as all groups were larger than 30 individuals, with the exception of the group aged less than 4 years that did not meet the Rome criteria, for which we used the Shapiro–Wilk test, finding a normal distribution. Subsequently, we compared nominal variables to assess for potential associations between any 2 variables using the chi-square test or the Fisher exact test if the expected value in any of the cells was less than 5. We used the Student t test to compare qualitative and quantitative variables after applying checking the homogeneity of variance assumption by means of the Levene test.
ResultsIn the period under study, 574 patients aged less than 16 years made an initial visit to the paediatric gastroenterology clinic of our hospital. Of this total, 44.6% had a clinical presentation compatible with a FGID, but only 32.4% met the Roma IV criteria. Fig. 1 presents the distribution of the total group of patients managed in the clinic based on the suspicion of FGIDs and the confirmation based on the Rome IV criteria by age group.
Table 1 summarises the demographic characteristics and the duration of symptoms at the time of diagnosis in the group of patients with suspected FGIDs and the subset that met the Rome IV criteria. We did not find statistically significant differences in the frequency of FGIDs based on the Roma IV criteria between male and female patients, but we did find a significantly higher probability of receiving a FGID diagnosis in the group aged more than 4 years compared to younger patients (P = .04).
Demographic characteristics and duration of symptoms of the patients included in the study, overall and based on whether they did nor not meet the Rome IV criteria for diagnosis of FGIDs.
| Total patients | Rome IV met | Rome IV not met | |
|---|---|---|---|
| n | 256 | 186 | 70 |
| Female, n (%) | 130 (50.8%) | 95 (51.1%) | 53 (50%) |
| Mean age in years (SD) | 8.08 ± 4.3 | 8.4 ± 4.2 | 7.23 ± 4.5 |
| Median duration in months (range) | 7 (0.5-150) | 7 (1-150) | 5 (0.5-36) |
FGID, functional gastrointestinal disorder; SD, standard deviation.
In the period under study, 189 children under 4 years made a first visit to the clinic. A FGID was suspected in 26.9%, but only 16.4% met the Rome IV criteria. Thus, the annual frequency of FGIDs based on the Roma IV criteria in this age group was 16.4%.
Table 2 presents the frequency of each disorder in the group aged less than 4 years, overall and by sex (female).
Frequency of FGIDs based on Rome IV criteria in children under 4 years in our region.
| Frequency of FGID Total (%) | Sex distribution of FGIDs Female (%) | |
|---|---|---|
| G1. Infant regurgitation | 7 (22.5%) | 3 (42.8%) |
| G2. Rumination | 1 (3.2%) | 1 (100%) |
| G3. Cyclic vomiting syndrome | 0 | 0 |
| G4. Infant colic | 1 (3.2%) | 0 (0%) |
| G5. Functional diarrhoea | 5 (16.1%) | 2 (40%) |
| G6. Infant dyschezia | 2 (6.5%) | 2 (100%) |
| G7. Functional constipation | 15 (48.4%) | 10 (66%) |
| Total | 31 |
In the group with a FGID diagnosis based on the Rome IV criteria, 58.1% of patients were female and the mean age was 1.5 years (SD, 1.1). The time elapsed from the onset of symptoms to diagnosis was 4 months (range, 1–24).
The most frequent FGID was functional constipation, diagnosed in 15 patients (48.4%), followed by infant regurgitation in 7 (22.5%) and functional diarrhoea in 5 (16.1%). None of the patients in the series had cyclic vomiting syndrome.
Patients aged more than 4 yearsThe annual frequency of FGIDs based on the Rome IV criteria in this age group was 40.3%, although these disorders were suspected in 53.2%. This group of patients constituted a majority in the overall sample (67%) and in the total group of patients with a FGID diagnosis based on the Rome IV criteria (83.3%)
In this age group, 49.7% of the patients (n = 77) were female and the mean age was 9.8 years (SD, 3). The median time elapsed from onset to the diagnosis was 7 months (range, 1–150 months).
The most frequent FGID was functional abdominal pain not otherwise specified (29%), followed by functional dyspepsia (28.4%), functional constipation (16.8%) and irritable bowel syndrome (16.1%). None of the patients met the criteria for aerophagia or abdominal migraine.
Table 3 presents the frequency of each disorder in the group aged more than 4 years, overall and by sex (female).
Frequency of FGIDs based on Rome IV criteria in children older than 4 years in our region.
| Frequency of FGID Total (%) | Sex distribution of FGIDs Female (%) | |
|---|---|---|
| H1a. Cyclic vomiting syndrome | 1 (0.6%) | 0 (0%) |
| H1b1. Functional nausea | 4 (2.6%) | 2 (50%) |
| H1b2. Functional vomiting | 2 (1.3%) | 1 (50%) |
| H1c. Rumination syndrome | 2 (1.3%) | 1 (50%) |
| H1d. Aerophagia | 0 | |
| H2a. Functional dyspepsia | 44 (28.4%) | 28 (63%) |
| H2b. Irritable bowel syndrome | 25 (16.1%) | 7 (28%) |
| H2c. Abdominal migraine | 0 | |
| H2d. Abdominal pain not otherwise specified | 45 (29%) | 24 (53%) |
| H3a. Functional constipation | 26 (16.8%) | 10 (38%) |
| H3b. Nonretentive faecal incontinence | 6 (3.9%) | 4 (66%) |
| Total | 155 |
We assessed for seasonal patterns in the frequency of diagnosis of these disorders, grouping initial visit dates by trimester of the year (Table 4).
Trimestral frequency of diagnoses based on Rome VI criteria, overall and by age group.
| 1st trimester | 2nd trimester | 3rd trimester | 4th trimester | P | |
|---|---|---|---|---|---|
| Patients diagnosed based on Rome IV/total patients per trimester (%) | 57/168 (33.9%) | 45/149 (30.2%) | 35/109 (32.1%) | 49/148 (33.1%) | .96 |
| Children <4 years diagnosed based on Rome IV/total <4 years per trimester (%) | 6/43 (13.9%) | 11/47 (23.4%) | 6/33 (18.1%) | 8/66 (12.2%) | .57 |
| Children >4 years diagnosed based on Rome IV/total >4 years per trimester (%) | 51/125 (40.8%) | 34/102 (33%) | 29/76 (38.1%) | 41/82 (50%) | .51 |
We did not find significant differences in the frequency of visits between trimesters in the group of patients that received a FGID diagnosis based on the Rome IV criteria (P = .96) or between age groups (age <4 years, P = .57; age >4 years, P = .51). However, when we compared the frequency of visits in every possible pair of trimesters, we did find a significantly higher frequency of visits in the group aged more than 4 years in the last trimester compared to the second trimester (50% vs 33%; P = .014) and the third trimester (50% vs 38.1%; P = .048). In contrast, in the group aged less than 4 years the highest frequency of visits corresponded to the second trimester (23.4%) and the lowest to the last trimester (12.2%), a difference that neared statistical significance (P = .05).
Testing and treatmentAs regards performance of diagnostic tests, 51.5% of patients had undergone testing at the PC level, while tests were ordered in our clinic for 31%. Tests were only avoided at both levels of care in only 11.7% of patients. In the analysis by age group, we found that performance of tests was avoided altogether in 19.6% of patients aged less than 4 years and in 9.7% of patients older than 4 years (P = .049).
When it came to the treatment received by patients with a diagnosis of FGID based on the Rome IV criteria, 46.7% received it at the PC level and 64.5% through our clinic. By age, in the group of patients with a diagnosis of FGID based on the Rome IV criteria, 77.4% of those aged less than 4 years and 41.2% of those older than 4 years received treatment at the PC level (P = .02), and 75% of those under 4 years and 62.7% of those over 4 years at the speciality clinic (P > .05).
DiscussionThe annual frequency of FGIDs based on the Rome IV criteria in children under 16 years that made the initial visit to the paediatric gastroenterology clinic of our hospital was 32.4%. This percentage was larger than the percentages reported in studies of similar characteristics that applied the Rome IV criteria in patients aged less than 18 years in the United States (24.9%) and patients aged 8 to 18 years in Colombia (21.1%).7,10 The only study we found conducted in the Mediterranean region of Europe was based on the Rome III criteria and found a prevalence of 27.5% in patients aged 4 to 18 years.2
In children aged less than 4 years, we found a frequency of 16.4%, lower compared to the frequency reported by Robin et al in the United States (24.7%).10 The most frequent disorder was constipation, diagnosed in nearly half the patients (48.4%), followed by infantile regurgitation (22.5%), which was also the case in the study of Robin et al, although with lower frequencies (17.2% for constipation and 4.7% for regurgitation).10 It is worth noting that functional diarrhoea, which was the third most frequent disorder in our series (16.1%), was not represented at all in the study by Robin et al.10 Cyclic vomiting syndrome, which Robin et al found to be an infrequent disorder in the United States (2%), was not diagnosed in any of the patients in our study.
In the group aged more than 4 years, we found a frequency of FGIDs of 40.3%, which was also higher compared to the aforementioned studies that applied the Roma IV criteria: 21.2% in the study by Saps et al in Colombia and 25.0% in the study by Robin et al in the United States.7,10 In our study, the most frequent disorder was functional abdominal pain not otherwise specified (29%), followed by functional dyspepsia (28.4%). In the studies in Colombia and the United States, the most frequent disorder was functional constipation (with a prevalence of 10.7% and 14.1%, respectively), and the second most frequent FGID, as occurred in our patients, was functional dyspepsia (3% in the study of Saps et al, 7.6% in the study of Robin et al.).7,10 However, 42% of the patients that met the criteria for functional abdominal pain not otherwise specified and 47.8% of patients with dyspepsia had symptoms of constipation, but did not meet the full Roma IV criteria required to receive a diagnosis of functional constipation.
We ought to remark on the presence of the disorders newly included in the fourth version of the Rome criteria, such as functional nausea and functional vomiting, found in 3.3% of patients in our series, a higher frequency compared to the one reported by Saps et al in Colombia (0.7%) and Robin et all in the United States (1.9%).7,10 On the other hand, we did not find any cases of aerophagia or abdominal migraine, which were detected in 2.6% and 1.1% of patients, respectively, in the United States study, and their frequency was nearly negligible in the Colombian study (0.5% for both).7,10 We ought to highlight that both of those studies compared the frequency of FGIDs applying the Rome III versus the Rome IV criteria, and both agreed that the prevalence of abdominal migraine decreased considerably with the change in criteria.7,10
Lewis et al carried out a previous to analyse FGIDs in children aged 4 to 18 years based on a questionnaire that applied the Rome III criteria, and found a prevalence of 23.1% based on the reports of 949 parents, with the most frequent disorders being functional constipation (13%), abdominal migraine (9.2%) and aerophagia (4.3%), which contrasts with the results we obtained applying the Rome IV criteria, as we already noted.1 In our study, we identified cases of all the contemplated disorders with the exception of rumination.1
Despite differences in methodology between our study, in which patients were categorised based on a medical criterion at the clinic, and the aforementioned studies of Saps et al and Robin et al, in which patients were classified based on data obtained through questionnaires completed by patients/parents, the results were quite similar.7,10
In our clinic, FGIDs account for nearly half of the initial visits conducted each year, and one third of patients meet the Rome IV criteria. Although the Rome criteria are increasingly inclusive, we found that 27.3% of patients with compatible manifestations did not meet the Rome IV criteria for diagnosis of a FGID (40% in the group <4 years and 24.3% in the group >4 years). This suggests the need to continue improving the diagnostic criteria to allow classification of the largest possible number of patients.
As regards seasonal variability in the diagnosis of these disorders, although we did not find overall differences between the different trimesters, in patients aged more than 4 years we found a higher frequency of consultation in the last trimester of the year compared to the second, and third. These trimesters with the lowest frequencies corresponded to the spring and summer, and one possible explanation of the lower frequency is a decrease in stressors such as attendance to school or the many extracurricular activities that patients usually engage in during the school year, which supports the hypothesis that psychosocial factors are associated with these disorders.
On the other hand, although the application of the Rome IV criteria is meant to help diagnose FGIDs using the fewest possible diagnostic tests, we found that a substantial number of diagnostic tests are still being performed (especially in the older age group) both in PC and in our clinic. The fact that the pathophysiology of these disorders has not been clearly elucidated and the persistence of symptoms may generate uncertainty in specialists regarding the lack of an organic aetiology and prompt them to perform tests to rule out this possibility. Also, despite these disorders being functional in nature, a large percentage of patients received treatment both in the PC system and in our clinic. One explanation is that in many instances, empirical treatment is offered to alleviate the symptoms of the patients and to reduce the anxiety of the family.
The main strengths of our study are that, to our knowledge, there are no other studies of these characteristics conducted in Spain, and the long follow-up period, which allowed us to analyse seasonal variations and to include a substantial number of patients.
As for its limitations, there is a risk of classification bias stemming from the observer, as disorders were classified based on how the paediatric gastroenterologist interpreted the symptoms evinced in the anamnesis. In addition, the symptoms were reported by patients or parents relying on their memory of specific events and their frequency, which carries a risk of recall bias, and therefore we are not able to guarantee the external validity of our findings.
The sample was obtained in a clinic in the south-east of the Community of Madrid, which manages most of the patients in the area, so it may not be representative of trends in the rest of the Community of Madrid or the overall paediatric population of Spain.
In conclusion, we confirmed that FGIDs are very prevalent in our region and that there are seasonal variations that would be interesting and relevant to investigate further. When we compared our findings to similar studies conducted in other countries, we found that the frequency of these disorders varied depending on the region where they were being evaluated and the criteria applied for the purpose, and that variations are even found when the same criteria are applied, which may be related to the idiosyncrasies of each culture. Further studies are required to help define FGIDs, their prevalence and relevant cultural differences in order to continue to finetune the classification of these diseases.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Alonso-Bermejo C, Barrio J, Fernández B, García-Ochoa E, Santos A, Herreros M, et al., Frecuencia de trastornos gastrointestinales funcionales según criterios Roma IV, Anales de Pediatría. 2022;96:441–447.
This study was presented as a poster at the I Digital Congress of the AEPED (November 2020)