The aim of the study was to investigate the impact of different complementary feeding methods on the prevalence of functional constipation symptoms in infants at 12 months of age.
Material and methodsRandomized clinical trial in mother–infant dyads that underwent the intervention at 5.5 months post birth, randomly allocated to one of three complementary food introduction methods: PLW (parent-led weaning), Baby-led Introduction to SolidS (BLISS) and a mixed approach. The symptoms of constipation were assessed at 12 months with an online questionnaire based on the Rome IV diagnostic criteria and adapted to our sample. The data were summarised as absolute frequencies and percentages and compared by means of the χ2 test. The project was approved by the ethics committee of the Hospital de Clínicas de Porto Alegre under number 2019-0230.
ResultsWe analysed data corresponding to 135 infants, 45 allocated to PLW, 48 to BLISS and 42 to the mixed approach. The prevalence of constipation symptoms was 49.6% in the overall sample (n = 67), 60% (n = 27) in the PLW group, 47.9% (n = 23) in the BLISS group and 40.5% (n = 17) in the mixed approach group. We found no association between functional constipation symptoms and the method used to introduce complementary foods (P = .183).
ConclusionsThe prevalence of functional constipation symptoms was high in the study population. The presence of constipation symptoms was not associated with the complementary feeding approach.
El objetivo del estudio fue investigar el impacto de diferentes métodos de alimentación complementaria en la prevalencia de síntomas de estreñimiento funcional en lactantes a los 12 meses de edad.
Materiales y métodosEnsayo clínico aleatorizado realizado en díadas madre-lactante sometidas a intervención a los 5,5 meses del nacimiento, con asignación aleatoria a uno de los tres métodos de introducción de sólidos: destete dirigido por la madre, o parent-led weaning (PLW), método Baby-Led Introduction to SolidS (BLISS) dirigido por el lactante, y mixto. Los síntomas de estreñimiento se evaluaron a los 12 meses mediante un cuestionario en línea basado en los criterios diagnósticos de Roma IV y adaptado a la muestra. Los análisis se realizaron mediante la prueba χ2 y los datos se expresaron como frecuencias absolutas y porcentajes. El proyecto fue aprobado por el comité de ética del Hospital de Clínicas de Porto Alegre con el número 2019-0230.
ResultadosSe analizaron los datos de 135 lactantes, 45 asignados al método PLW, 48 al BLISS y 42 al método mixto. La prevalencia de síntomas de estreñimiento fue del 49,6% en la muestra global (n = 67), siendo del 60% (n = 27) en el método PLW, 47,9% (n = 23) en el BLISS y 40,5% (n = 17) en el mixto. No hubo asociación entre los síntomas de estreñimiento funcional y el método de introducción de la alimentación complementaria (p = 0,183).
ConclusionesLa prevalencia de estreñimiento y sus síntomas fue alta en la población estudiada. La prevalencia de los síntomas de estreñimiento funcional no se asoció con el método de alimentación complementaria.
Functional constipation (FC) is defined as the delay or difficulty in stool evacuation that cannot be explained by another medical condition.1 According to the Rome IV criteria, the diagnosis of FC requires the presence of 2 or more of the following symptoms for at least a month: fewer than 3 bowel movements per week, one or more episodes of faecal incontinence per week, faecal retention, painful defecation or hard stools or presence of a large faecal mass in the rectum.2
There are disagreements regarding the prevalence of constipation in children in the literature; however, it is estimated that up to 30% of the children suffer from this type of gastrointestinal disorder.3 Functional constipation accounts for more than 90% of cases of constipation in children4 and several factors interact to protect or promote the onset of symptoms, such as the type of birth,5 breastfeeding6 or the consumption of cow’s milk7 or infant formula.7
Dietary factors also play an important role in the pathophysiology of FC.1 The introduction of complementary foods is an important milestone in the establishment of healthy eating habits and the prevention of gastrointestinal disorders, including constipation. Current guidelines recommend starting to introduce solid foods at age 6 months.8,9 The Ministry of Health of Brazil advises a slow and gradual introduction of complementary feeding, starting with a variety of pureed foods fed with a spoon with progressive changes until reaching the texture consumed by the family.10 Other approaches for the introduction of complementary foods have been proposed to date, such as the baby-led weaning (BLW) method and the Baby-led Introduction to SolidS (BLISS).11 Both methods recommend the introduction of food in strips or sticks, allowing the child to hold them and bring them to the mouth independently under adult supervision.11,12
A review of the benefits of infant-guided introduction to solids found that infants fed by these methods were at lower risk of consuming salt and sugar between ages 25 and 36 months13 and of having a high body mass index (BMI) for age.14 However, none of them evaluated the prevalence of constipation symptoms in infants fed with these approaches.
The aim of our study was to investigate the prevalence of different approaches to the introduction of solid foods and their impact on the prevalence of FC symptoms at age 12 months.
Material and methodsStudy designThe study was a 3-arm controlled trial on mother-infant dyads randomly allocated to one of the following groups: (A) parent-led weaning (PLW); (B) baby-led BLISS approach; (C) mixed method designed exclusively for this research, combining the PLW and BLISS approaches.15
Sample selectionParticipants were recruited through social media, websites and groups for mothers in addition to informational posters in health care settings. Mothers living in the Porto Alegre metropolitan region of healthy singleton infants born to term with birth weights of 2500 g or greater and who had not yet started introducing solids were considered eligible to participate. We excluded infants with any form of dietary restriction indicated by their doctor. The inclusion criteria were verified at the time of recruitment and before randomization.
Once they had expressed interest in the study and the inclusion criteria had been verified, candidates considered eligible were provided with an informational form explaining the details, risks, and benefits of the study, and researchers answered any questions by phone or email. When candidates confirmed interest in the study, a link to the online consent form was sent to them by email. Once the online consent form had been submitted, the names of participants were entered in a 3-block randomization list generated electronically (http://www.randomization.com) by a blinded researcher. Mothers were informed of the group they had been assigned to at the time of intervention.
InterventionWhen their infants turned 5.5 months of age, mothers participated in a workshop about the introduction of solid food in a private nutrition clinic. The clinic had an experimental kitchen, where trained nutritionists taught parents how to initiate complementary feeding according to the group they had been allocated to, preparing samples of meals in real time.
Regardless of the allocated method, mothers were instructed to breastfeed, exclusively through age 6 months and complemented with solid foods through age 2 or more years. In addition, mothers received support materials created specifically for the study that varied depending on the group they had been allocated to as described below.
In the PLW group, parents were instructed to start offering solid foods from age 6 months, introducing them slowly and gradually, spoon-fed by the adult. The family was directed to offer the child complementary foods (cereals, tubers, meat, legumes, fruits or vegetables) 3 times a day, without strict schedules and respecting the infant’s appetite, increasing the offer as months went by. The initial consistency of the food should be a paste, mashed with a fork (from 6 to 8 months in the form of porridge and purees), with a gradual progression so that the infant would consume the food with the same consistency as the family by age 12 months, with a variety of colours and food groups consumed in every meal, without blending or sieving the food. Furthermore, the prepared foods should be offered separately, so that the infant could assimilate the flavour and characteristics of each of them. Parents were advised to avoid low-energy preparations, such as soups or broths, as well as sugar, coffee, canned food, fried foods, soft drinks, juices, candies, snacks and other sweets in the first 2 years of life; with salt used in moderation.10
In the BLISS group, parents were instructed to encourage the infant to self-feed, although always assisted by an adult and during family meals. The consistency of the food offered from age 6 months should be firm, in shapes that allowed the infant to grab food with the hands and chew them, cut into elongated shapes, such as strips or sticks, to facilitate grasping and prevent choking. Parents were advised not to rush the child during the meal, allowing time to explore flavours and textures, and to offer 3 types of food at each meal: a source of iron (for example, red meat), a source of energy and a source of fibre, such as fruits or vegetables.12
When it came to the mixed method, which is the approach proposed by our research group, parents were instructed to initiate complementary feeding with the BLISS approach. Training and printed materials were provided on how to identify signs of satisfaction in the child. If the child was not satisfied or showed no interest in the food presented with the BLISS technique, parents were advised to offer food with the PLW approach in the same meal.
Data collectionAfter signing the consent form, mothers received an online questionnaire used to collect data on the sociodemographic characteristics of the family (maternal age, family income, maternal education) and the characteristics of the child (birth weight, birth length, type of breastfeeding).
When infants turned 12 months of age, mothers received a new online questionnaire asking about the duration of breastfeeding (exclusive and overall), iron supplementation, age at initiation of complementary feeding, adherence to the method for introducing complementary feeding, food consumption markers and bowel habits. The presence of FC symptoms was assessed based on the Rome IV diagnostic criteria (stool frequency, straining during defecation, stool consistency, crying or pain when passing stools, blood in the stool, abdominal cramps and use of laxatives) and the Bristol stool scale was used to illustrate stool consistency. Functional constipation was defined as the child exhibiting at least 2 of the described symptoms.
Exclusive breastfeeding was defined as the child receiving no liquid or solid (including water) other than human milk, with the exception of oral rehydration solution, or drops/syrups of vitamins, minerals or medications. Breastfeeding at 12 months was defined as receiving any amount of human milk by bottle, cup or breast; formula feeding at 12 months was defined as the infant receiving any amount of modified cow’s milk; cow’s milk consumption at 12 months was defined as the infant receiving any amount of cow’s milk.
The assessment of fibre intake was performed through food consumption markers, mainly by the consumption of vegetables, greens and beans the day before the questionnaire was completed, based on the guidelines of the Food and Nutrition Surveillance System (SISVAN).16
Statistical analysisWe created a database with the Statistical Package for the Social Sciences (SPSS) software, version 21.0, with double entry and subsequent validation. Parametric data were summarised as mean and standard deviation (SD) and nonparametric data as median and interquartile range. We used the χ2 test to detect differences between proportions, the Kolmogorov–Smirnov test to assess whether quantitative data followed a normal distribution, and the Kruskal Wallis test to detect differences between medians. Poisson regression was performed to calculate prevalence ratios (PRs) with the corresponding 95% confidence intervals (CIs) for FC symptoms comparing the complementary feeding methods. For all analyses, we established a level of significance level of 5% (P < .05) and a 95% confidence interval.
Ethical considerationsThe study was approved by the Ethics Committee of the Hospital de Clínicas de Porto Alegre (HCPA) (file number 2019-0230, CAAE: 1537018500005327) and registered in the Brazilian Registry of Clinical Trials (ReBEC) with the identification code RBR-229scm. The study adhered to bioethical guidelines, as per Resolution No. 466 of December 12, 2012, of the National Health Council of Brazil.17 Further information about the randomized trial can be found in the published study protocol.15
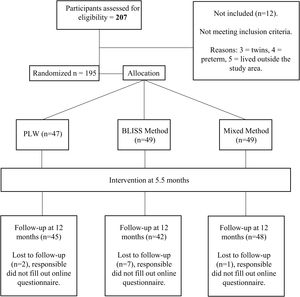
ResultsIn the initial recruitment, 207 mothers expressed interest in participating in the study, of who 12 did not meet the inclusion criteria. Thus, 195 were considered eligible and randomized to the 3 methods to introduce complementary feeding. A total of 139 mothers attended the intervention, of who 135 completed the questionnaire when the infant was 12 months of age. Fig. 1 presents a flowchart of the sample selection process.
Table 1 summarises the characteristics of the sample. In the overall sample, the maternal educational attainment in most families was of 15 years or more (76.9%). The total household income ranged from 3 to 10 times the minimum wage (59.8%). The minimum wage in Brazil is R$ 1212.00 and is the most widely used measure of income. As regards the birth characteristics, 84 (62.2%) of participants had a caesarean section and 72 (53.3%) of the infants were female. The percentage of infants breastfed exclusively until 6 months post birth was 54.1%, and at 12 months, 101 (74.8%) were still breastfeeding and 55 (40.7%) were fed infant formula. The median age at which solids started to be introduced was 180 days (180;180) days. At the 12-month time point, most infants did not consume cow’s milk (91.9%), were receiving iron supplementation (72.6%) and were not enrolled in day care (71.1%). We did not find significant differences in any of the analysed characteristics based on the method used for introducing complementary foods (P > .05).
Characteristics of the sample, overall and by method of introduction of complementary feeding (Porto Alegre, Rio Grande do Sul, Brazil).
| Total sample | PLW method | BLISS method | Mixed method | P | |
|---|---|---|---|---|---|
| N = 135 | n = 45 | n = 48 | n = 42 | ||
| Maternal educational attainment [N = 134] | |||||
| 1–14 years | 31 (23.1%) | 15 (34.1%) | 10 (20.8%) | 6 (14.3%) | .084 |
| ≥15 years | 103 (76.9%) | 29 (65.9%) | 38 (79.2%) | 36 (85.7%) | |
| Household income* [N = 132] | |||||
| <3 × minimum wage | 27 (20.5%) | 10 (22.2%) | 9 (19.6%) | 8 (19.5%) | .214 |
| 3–10 × minimum wage | 79 (59.8%) | 30 (66.7%) | 23 (50.0%) | 26 (63.4%) | |
| >10 × minimum wage | 26 (19.7%) | 5 (11.1%) | 14 (30.4%) | 7 (17.1%) | |
| Type of delivery | |||||
| Vaginal delivery | 51 (37.8%) | 12 (26.7%) | 19 (39.6%) | 20 (47.6%) | .125 |
| Caesarean delivery | 84 (62.2%) | 33 (73.3%) | 29 (60.4%) | 22 (52.4%) | |
| Infant sex | |||||
| Female | 72 (53.3%) | 25 (55.6%) | 26 (54.2%) | 21 (50.0%) | .865 |
| Male | 63 (46.7%) | 20 (44.4%) | 22 (45.8%) | 21 (50.0%) | |
| Feeding modality | |||||
| Exclusive breastfeeding at 6 months | 73 (54.1%) | 27 (60.0%) | 24 (50.0%) | 22 (52.4%) | .431 |
| Breastfeeding at 12 months | 101 (74.8%) | 36 (80.0%) | 36 (75.0%) | 29 (69.0%) | .500 |
| Formula at 12 months | 55 (40.7%) | 21 (46.7%) | 17 (35.4%) | 17 (40.5%) | .544 |
| Age at initiation of CF | |||||
| Median age (days) | 180 (180–180) | 180 (171–180) | 180 (180–180) | 180 (180–180) | .152 |
| Cow’s milk consumption at 12 months | |||||
| Yes | 11 (8.1%) | 4 (8.9%) | 3 (6.3%) | 4 (9.5%) | .853 |
| No | 124 (91.9%) | 41 (91.1%) | 45 (93.8%) | 38 (90.5%) | |
| Iron supplementation at 12 months | |||||
| Yes | 98 (72.6%) | 33 (73.3%) | 34 (70.8%) | 31 (73.8%) | .943 |
| No | 37 (27.4%) | 12 (26.7%) | 14 (29.2%) | 11 (26.2%) | |
| Daycare attendance at 12 months | |||||
| Yes | 39 (28.9%) | 18 (40.0%) | 12 (25.0%) | 9 (21.4%) | .123 |
| No | 96 (71.1%) | 27 (60.0%) | 36 (75.0%) | 33 (78.6%) | |
| Median age at enrolment (days) | 210 (180−306) | 225 (180−286) | 210 (180−333) | 180 (165−277) | .593 |
BLISS, Baby-led Introduction to SolidS; CF, complementary feeding; PLW, parent-led weaning.
Statistical tests: Pearson’s χ2 for proportions for qualitative variables, Kruskal Wallis test for quantitative variables.
Table 2 describes the associations between the bowel habits of infants and the method of introduction of complementary feeding. Half of the sample (49.6%) exhibited FC symptoms. Out of the total sample, 117 (86.7%) infants passed stools daily, and 9 (6.7%) had type 2 stools on the Bristol stool scale. Most infants (54.1%) exhibited straining during defecation once a week or less, and 114 (84.4%) did not cry or express pain during bowel movements. Laxatives were never used by 85.9% of the sample, and, in the subset that used them, 8 (5.9%) used them once and 11 (8.2%) twice or more. Anal fissures were detected in 6 infants (4.4%), just over half the sample (54.1%) suffered from colic, and most infants (91.1%) had never had bloody stools. We did not find a statistically significant association between FC (P = .183) or gastrointestinal symptoms related to constipation and the method used to introduce complementary foods.
Presence of symptoms of functional constipation at 12 months of life based on Rome IV diagnostic criteria, overall and by complementary feeding introduction method (Porto Alegre, Rio Grande do Sul, Brazil).
| Total sample | PLW method | BLISS method | Mixed method | P | |
|---|---|---|---|---|---|
| N = 135 | n = 45 | n = 48 | n = 42 | ||
| n (%) | |||||
| Stool frequency | |||||
| Daily | 117 (86.7%) | 38 (84.5%) | 43 (89.6%) | 36 (85.7%) | .692 |
| 3−6 a week | 15 (11.1%) | 5 (11.1%) | 4 (8.3%) | 6 (14.3%) | |
| ≤2 a week | 3 (2.2%) | 2 (4.4%) | 1 (2.1%) | 0 (0.0%) | |
| Stool consistency | |||||
| Type 2 | 9 (6.7%) | 4 (8.9%) | 4 (8.3%) | 1 (2.4%) | .461 |
| Straining during defecation | |||||
| Absent | 38 (28.1%) | 8 (17.8%) | 15 (31.3%) | 15 (35.7%) | .404 |
| Once a week or less | 73 (54.1%) | 27 (60.0%) | 25 (52.1%) | 21 (50.0%) | |
| ≥2 times a week | 24 (17.8%) | 10 (22.2%) | 8 (16.7%) | 6 (14.3%) | |
| Crying or pain during defecation | |||||
| Absent | 114 (84.4%) | 37 (82.2%) | 42 (87.5%) | 35 (83.3%) | .936 |
| Once a week or less | 17 (12.6%) | 6 (13.3%) | 5 (10.4%) | 6 (14.3%) | |
| ≥2 times a week | 4 (3.0%) | 2 (4.4%) | 1 (2.1%) | 1 (2.4%) | |
| Use of laxatives | |||||
| Never | 116 (85.9%) | 36 (80.0%) | 41 (85.4%) | 39 (92.9%) | .396 |
| Only once | 8 (5.9%) | 4 (8.9%) | 2 (4.2%) | 2 (4.8%) | |
| ≥2 times | 11 (8.2%) | 5 (11.1%) | 5 (10.4%) | 1 (2.4%) | |
| Presence of anal fissure | |||||
| Yes | 6 (4.4%) | 2 (4.4%) | 2 (4.2%) | 2 (4.8%) | 1.000 |
| No | 129 (95.6%) | 43 (95.6%) | 46 (95.8%) | 40 (95.2%) | |
| Colic | |||||
| Yes | 62 (45.9%) | 21 (46.7%) | 22 (45.8%) | 19 (45.2%) | .991 |
| No | 73 (54.1%) | 24 (53.3%) | 26 (54.2%) | 23 (54.8%) | |
| Blood in stools | |||||
| Yes | 12 (8.9%) | 6 (13.3%) | 4 (8.3%) | 2 (4.8%) | .418 |
| No | 123 (91.1%) | 39 (86.7%) | 44 (91.7%) | 40 (95.2%) | |
| Constipation | |||||
| Yes | 67 (49.6%) | 27 (60.0%) | 23 (47.9%) | 17(40.5%) | .183 |
| No | 68 (50.4%) | 18 (40.0%) | 25 (52.1%) | 25 (59.5%) | |
PLW, parent-led weaning; BLISS, Baby-led Introduction to SolidS; Statistical test: Pearson’s χ2 test for proportions.
Table 3 describes the association between the presence of FC symptoms with different risk and protective factors. Family, birth and infant characteristics were not significantly associated with the presence of FC symptoms. The PR of constipation symptoms based on the applied method of complementary feeding and using the PLW method as reference was 0.675 for the mixed method (95% CI, 0.436–1.045; P = .077) and 0.799 for the BLISS method (95% CI, 0.546–1.167; P = .245) (data not shown).
Associations between risk and protective factors and presence of constipation symptoms in infants at 12 months of age (Porto Alegre, Rio Grande do Sul, Brazil).
| Constipation symptoms present | Constipation symptoms absent | P | |
|---|---|---|---|
| Maternal educational attainment [N = 134] | |||
| 1–14 years | 15 (22.4%) | 16 (23.9%) | 1.000 |
| ≥15 years | 52 (77.6%) | 51 (76.1%) | |
| Household income* [N = 132] | |||
| <3 × minimum wage | 12 (18.5%) | 15 (22.4%) | .854 |
| 3–10 × minimum wage | 40 (61.5%) | 39 (58.2%) | |
| >10 × minimum wage | 13 (9.8%) | 13 (19.4%) | |
| Type of delivery | |||
| Vaginal delivery | 24 (35.8%) | 27 (39.7%) | .773 |
| Caesarean delivery | 43 (64.2%) | 41 (60.3%) | |
| Infant sex | |||
| Female | 36 (53.7%) | 36 (52.9%) | 1.000 |
| Male | 31 (46.3%) | 32 (47.1%) | |
| Feeding modality | |||
| Exclusive breastfeeding at 6 months | 35 (52.2%) | 38 (55.9%) | .801 |
| Breastfeeding at 12 months | 47 (70.1%) | 54 (79.4%) | .298 |
| Formula at 12 months | 29 (43.3%) | 26 (38.2%) | .673 |
| Age at initiation of CF | |||
| Median age (days) | 180 (179–180) | 180 (180–180) | .233 |
| Cow’s milk consumption at 12 months | |||
| Yes | 6 (9.0%) | 5 (7.4%) | .980 |
| No | 61 (91.0%) | 63 (92.6%) | |
| Iron supplementation at 12 months | |||
| Yes | 48 (71.6%) | 50 (73.5%) | .958 |
| No | 19 (28.4%) | 18 (26.5%) | |
| Daycare attendance at 12 months | |||
| Yes | 22 (32.8%) | 17 (25.0%) | .415 |
| No | 45 (67.2%) | 51 (75.0%) | |
| Median age at enrolment (days) | 210 (165−273) | 210 (180−358) | .416 |
CF, complementary feeding.
Statistical tests: Pearson’s χ2 for proportions for qualitative variables, Kruskal Wallis test for quantitative variables.
The analysis of fibre consumption revealed that out of the 135 infants in the sample, 121 (89.6%) had consumed vegetables, 28 (20.7%) greens and 115 (85.2%) beans the day before data collection. When we compared the approaches to the introduction of solid foods and the consumption of vegetables, greens and beans, we found no significant differences in consumption between the different methods (P = .639, P = .7,86, and P = .213, respectively) (data not shown).
DiscussionThe results of our study show that the prevalence of FC symptoms was high in the infants in the sample. However, we did not find an association between the method used to introduce complementary foods and constipation or its symptoms. The prevalence of FC symptoms found in our sample was higher compared to a randomized trial conducted in Brazil that found a prevalence of constipation of 15% in children who underwent an intervention that addressed feeding habits, such as breastfeeding and healthy introduction to solids.18 Contrary to our study, the researchers assessed for the presence of FC at age 6 years, which may have contributed to the differences in the results. In younger children, which made up our sample, it is harder to measure these symptoms accurately. In addition, there is a risk of selection bias, as including more mothers interested in the subject may have affected the outcomes and led to overestimation of the reported symptoms. Another particularity to take into consideration is that the questionnaire did not ask about the specific period the constipation symptoms occurred, which may have increased the reported frequency of constipation.
The complementary feeding methods used in these infants were safe from a micronutrient intake perspective,19 in addition to increasing exposure to vegetables and protein sources, thus contributing to an improved fibre intake.20,21 Contrary to previous publications, our analysis of the consumption of fibre-rich foods did not identify any statistically significant differences between the groups. This could be related to the fact that all 3 groups received nutritional guidance and may explain why different methods were not significantly associated with FC symptoms.
Breastfeeding is a protective factor for childhood gastrointestinal disorders.6,7,17 One of the mechanisms believed to contribute to the protection of infants against gastrointestinal diseases conferred by breastfeeding is the presence of human milk oligosaccharides (HMOs), abundant in breast milk, as they act as probiotics, nourishing and selecting bacteria in the gastrointestinal tract.22 Despite the high proportion of infants who were breastfed in the sample, we did not find an association between the absence of constipation symptoms and breastfeeding, which may have been due to the influence of complementary feeding, as solid foods had been introduced approximately 6 months before the assessment.
Unlike human milk, the consumption of cow’s milk by infants is a risk factor for constipation. A study conducted in Brazil that assessed the presence of constipation in preschool children found that those who received cow’s milk before age 6 months were up to 15 times more likely to have constipation.7 The consumption of cow’s milk at age 12 months in our sample was low compared to other studies in Brazil, probably due to the high educational attainment and socioeconomic status of the sample.23 However, despite the high prevalence of breastfeeding and infrequent consumption of cow’s milk, in addition to nutritional counselling, the presence of constipation symptoms in our sample was higher compared to the study in preschool children conducted in Brazil.7
Another factor that has been associated with FC symptoms is the mode of delivery. Vaginally delivered infants come in contact with a wide variety of microorganisms as they pass through the birth canal, whereas infants delivered by caesarean section are not exposed to the same microbiota.24 This difference in the colonization of the latter neonates may promote the development of diseases associated with immune system dysfunction.25 A cohort study based on data from the Japan Environment and Children’s Study that included 71 878 mother-infant pairs found an increased risk of FC at age 3 years in children born by caesarean section.5 In our sample, more than 60% of the children had been delivered by caesarean section, and the large proportion of caesarean delivery may have contributed to the high prevalence of FC symptoms observed in our study, although differences based on this variable were not statistically significant.
There are limitations to this study, such as the assessment of constipation symptoms at a single timepoint and the high socioeconomic status of the sample, which limits the generalization of the findings to the Brazilian population. The sample size may have been insufficient to obtain significant results in the tests performed to assess association. In addition, the fact that mothers were interviewed by a team of nutritionists and nutrition students may have kept them from disclosing nutritional problems. The analysis was made with the intention to treat, even though not all participants followed the assigned method. Divergence from the assigned method was most frequent in pairs assigned to the BLISS and PLW methods that ended up following the mixed method. More information about adherence can be found in another study in the same sample.26 The low adherence to the BLISS method may explain the results.
These limitations notwithstanding, our study is the first randomized clinical trial to analyse complementary feeding introduction methods in relation to the presence of constipation symptoms in infants in the Brazilian population. In addition, the mixed method was developed specifically for this research project. Studying the differences between the types of complementary feeding and their impact on infant health is very relevant in terms of giving families the autonomy to choose the most suitable method for them and to support more precise guidance and prescriptions in nutritional care.
In conclusion, we found a high prevalence of FC symptoms in the sample that was not associated with the methods of introduction of complementary feeding. More research is needed to investigate the association of the complementary feeding method with FC symptoms in infants, taking into account food intake and the timing of symptoms.
FundingThis study was funded by the Coordination for the Improvement of Higher Education Personnel and the Brazilian National Council for Scientific and Technological Development through master’s and doctorate’s scholarships; the budget for doctoral students and the Research and Events Incentive Fund at the Hospital de Clínicas de Porto Alegre.