Subglottic haemangiomas occur rarely but may be life-threatening if they become large enough to occlude the tracheal lumen. Given the difficulty of surgical access to these lesions and the high mortality they carry, the discovery of propranolol as a therapeutic agent1 has been promising.
We conducted a retrospective study of all pediatric patients with a diagnosis of subglottic haemangioma (11 in total) treated in a tertiary level hospital between 1997 and 2014. Three of the patients (27%) were male; and all were aged between 2 weeks and 2 years (mean, 4 months). All patients were followed up until resolution of the haemangioma.
The treatment received by each patient corresponded to the customary approach applied nationwide at the time the diagnosis was made, and could be thus distributed:
Between 1997 and 2000: There were three cases diagnosed in patients aged 1, 3 and 3 months, respectively. The first patient responded well to transoral CO2 laser microsurgery, with stridor resolving after the procedure. In the other two patients, stridor recurred a few weeks following surgery. They underwent a second CO2 laser resection, two months after the initial surgery in the first patient, and eight months after in the second.
Between 2001 and 2009: During this period, five cases were diagnosed, with three patients receiving oral corticosteroids and two remaining under observation until full spontaneous resolution of the haemangioma. Two of the three patients that received oral corticosteroids, aged 2 and 3 months at the time of diagnosis, responded well to oral corticosteroids at doses equivalent to 1mg/kg/day of methylprednisolone with progressive tapering off. Stridor resolved after two weeks of treatment in the first patient and after two months in the second patient. However, one patient developed iatrogenic Cushing syndrome at four months of treatment, and it was decided that she undergo CO2 surgery in order to discontinue oral corticosteroid treatment. Of the two patients that were monitored through the spontaneous involution of the haemangioma, one had needed a tracheotomy at age 2 months due to respiratory failure, followed by the diagnosis of subglottic haemangioma, and remained under observation for one year until the lesion had resolved in full. The second case corresponded to the incidental finding of haemangioma in a patient assessed for laryngomalacia at age 2 years, who remained under observation for 10 months until the lesion had resolved spontaneously.
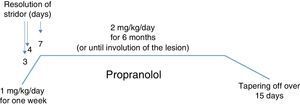
From 2010 on: during this period, three cases were diagnosed in patients aged 5, 3 and 2 months. All three patients responded well to treatment with oral propranolol, with resolution of stridor at three days, one week, and four days of treatment, respectively. None of the three experienced adverse effects associated with the use of beta-blockers. The lesions had become undetectable on examination by fibrolaryngoscopy at five months, one year and fifteen months, respectively.
Fig. 1 presents the treatment protocol used in patients managed with oral propranolol and marks the times at which complete resolution of symptoms with absence of stridor was observed.
Our study showed good initial outcomes of CO2 laser surgery in all patients, but also a high rate of recurrence, consistent with previous reports by other authors.2 We also observed that when oral corticosteroids were used as the first-line treatment in a later period, patients developed complications (Cushing syndrome).3
However, when a propranolol treatment protocol started to be implemented in pediatric patients with a diagnosis of subglottic haemangioma, stridor resolved in our patients at three, four and seven days after initiation of treatment, so that they could be discharged to outpatient follow-up care. This quick clinical response to propranolol has been observed by other researchers.4 The low incidence of subglottic haemangioma precludes the possibility of conducting studies with large sample sizes, and while we have observed promising results, there is not enough evidence to assert that treatment with propranolol will suffice in all cases.
To date, propranolol has allowed an effective and safe management with good disease control in the three patients treated with it. Although we have not observed any adverse effects in these three patients, we must remain alert to the potential development of adverse effects associated with beta-blockers, such as hypotension, bronchospasm and hypoglycaemia, which can be dangerous in the pediatric age group.
Please cite this article as: Krstulovic C, Ibañez-Alcañiz I, Alamar-Velázquez A, López-Andreu J, Evoli-Buselli M. Respuesta rápida de hemangiomas subglóticos a propranolol. An Pediatr (Barc). 2016;85:210–211.
Previous presentations: The results of this study were presented at the 65 Congreso Nacional of the SEORL-CCC under the title Evolución y resultados del tratamiento de hemangiomas subglóticos (Evolution and outcomes in the treatment of subglottic haemangiomas); October 18, 2014; Madrid, Spain.