Different postoperative prognostic markers have been identified in patients that have undergone congenital heart defect surgery, such as venous oxygen saturation and lactate levels.1 Cardiac surgery with extracorporeal circulation (ECC) produces an inflammatory response consisting of hyperglycaemia and elevated C-reactive protein (CRP) and troponin (Tp) levels. The purpose of this study was to determine the impact of these parameters on postoperative morbidity.
We conducted a prospective observational study of a cohort of 101 patients in a paediatric intensive care unit (ICU). The inclusion criteria were: (a) age more than 1 month and (b) surgery with ECC. The exclusion criteria were: (a) refusal to give informed consent and (b) use of corticosteroids or insulin.
The preoperative variables were type of heart defect and surgical risk (RACHS-1). The postoperative variables were glycaemia (mg/dL), CRP (mg/L), and Tp (ng/L). Four venous blood samples were collected in order to measure these variables, at admission, at 4 and 8h from admission, and at 8 am the following morning. Troponin was determined with the high sensitivity cardiac troponin T assay, and a level above 100ng/L was considered pathological. We also measured other variables, such as duration of mechanical ventilation and length of ICU stay.
We classified the patients according to the RACHS-1 scoring system,2 and attributed to them a high surgical complexity (HSC) when their RACHS-1 score was higher than or equal to 3. We defined sustained hyperglycaemia (SHG) as glycaemia higher than 126mg/dL3 in all four measurements. We defined prolonged mechanical ventilation (PMV) as a duration higher than or equal to 72h; and a prolonged stay (PS) as a length of stay higher than or equal to 5 days.
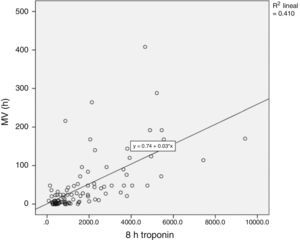
A total of 22 children (22%) presented SHG associated with a PS (chi square=7.3; P<.05). The patients with the highest levels of Tp were the ones that had PMV (Mann–Whitney=161; P<.001) and a PS (Mann–Whitney=518; P<.001). We also found a direct correlation between Tp levels and duration of mechanical ventilation (r=0.7; P<.01) (Fig. 1) and length of stay (r=0.5; P<.01).
The most frequent mean value of the RACHS-1 was category 3 (42%). The RACHS-1 score was correlated with the duration of mechanical ventilation (r=0.5; P<.01), and HSC was associated with PS (chi-square=5.2; P<.05). The levels of CRP had no statistical significance.
The variables that influenced PMV in our multivariate analysis were age and weight (P<.01), duration of ECC and aortic clamping (P<.05), the RACHS-1 score (P<.05), and levels of Tp (P<.01). The variables associated with PS were age and weight (P<.01), duration of ECC (P<.01) and of aortic clamping (P<.05), the RACHS-1 score (P<.01) and levels of Tp (P<.01).
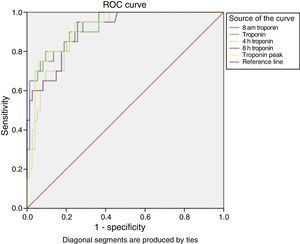
We proceeded to perform a multivariate analysis to predict PMV, in which only Tp reached statistical significance (P<.01). When we dichotomised the variable, we observed that every Tp determination was a significant predictor of PMV (Fig. 2).
The significant variables in the predictive model for PS were weight, duration of ECC and aortic clamping, and Tp level at 8 am. Among them, Tp at 8 am was the only variable with an area under the ROC curve of more than 0.75. After dichotomisation, all Tp determinations were significant predictors of PS.
The ECC technique produces a systemic response consisting of adrenergic stimulation4 and uncontrolled activation of inflammation leading to hyperglycaemia and the release of inflammatory mediators. The relationship between hyperglycaemia and a poor prognosis is not clearly established, although in our study SHG was associated with PS (P<.05).
Elevation of Tp levels has been associated with postoperative complications,5 and a decreasing trend is a marker of favourable prognosis. In this study, elevated Tp was associated with long durations of mechanical ventilation and lengths of stay, and could predict PMV (Fig. 2) as well as PS. The RACHS-1 score was correlated with the duration of mechanical ventilation; and patients with a HSC were the patients that had a PS.
The conclusions of this study are that Tp is the best predictor of postoperative morbidity and that a multifactorial assessment is a useful tool to identify children at risk, as demonstrated by other authors.6
Please cite this article as: García-Hernández JA, Fernández-Elías M, Martínez-López AI, Cayuela-Domínguez A, Cano-Franco J. Evaluación de la respuesta sistémica en el postoperatorio de las cardiopatías congénitas. An Pediatr (Barc). 2015;82:435–436.