Dysphagia is very common in children with neurological disabilities. These patients usually suffer from respiratory and nutritional problems. The videofluoroscopic swallowing study (VFSS) is the most recommended test to evaluate dysphagia, as it shows the real situation during swallowing.
ObjectivesTo analyse the results obtained in our centre after one year of the implementation of VFSS, the clinical improvement after confirmation, and the prescription of an individualised treatment for the patients affected.
Material and methodsVFSS performed in the previous were collected. The following variables were analysed: age, pathology, degree of neurological damage, oral and pharyngeal and/or oesophageal dysphagia and its severity, aspirations, prescribed treatment, and nutritional and respiratory improvement after diagnosis. A statistical analysis was performed using SPSS v21.
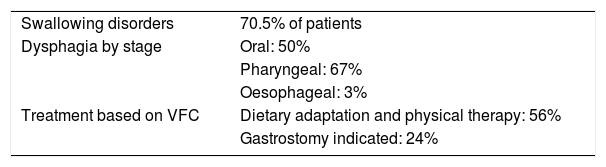
ResultsA total of 61 VFSS were performed. Dysphagia was detected in more than 70%, being moderate-severe in 58%. Aspirations and/or penetrations were recorded in 59%, of which 50% were silent. Adapted diet was prescribed to 56%, and gastrostomy was performed on 13 (21%) patients. A statistical association was found between neurological disease and severity of dysphagia. The degree of motor impairment is related to the presence of aspirations. After VFSS evaluation and treatment adjustment, nutritional improvement was found in Z-score of weight (+0.3SD) and BMI (+0.4SD). There was respiratory improvement in 71% of patients with dysphagia being controlled in the Chest Diseases Department.
ConclusionsAfter implementation of VFSS, a high percentage of patients were diagnosed and benefited from a correct diagnosis and treatment. VFSS is a fundamental diagnostic test that should be included in paediatric centres as a diagnostic method for children with suspected dysphagia.
La disfagia es muy frecuente en niños con discapacidad neurológica. Estos pacientes suelen presentar problemas respiratorios y nutricionales. El estudio de la deglución por videofluoroscopia (VFC) suele ser el más recomendado, ya que revela la situación real durante la deglución.
ObjetivosEstudiar los resultados obtenidos en la evaluación diagnóstica tras un año desde la implantación de la VFC en nuestro centro, y analizar la mejoría clínica tras la confirmación por VFC y la prescripción de un tratamiento individualizado en los niños con disfagia orofaríngea.
Material y métodosSe recogen las VFC realizadas en el último año. Se analizan las siguientes variables: edad, enfermedad, grado de afectación neurológica, tipo de disfagia (oral, faríngea y/o esofágica), gravedad, aspiraciones y/o penetraciones, tratamiento prescrito y mejora nutricional y/o respiratoria tras el diagnóstico. Se realiza análisis estadístico mediante SPSS v21.
ResultadosSe realizaron 61 VFC. Se detectó disfagia en más del 70%, siendo moderadas-graves en el 58%. Se visualizaron aspiraciones y/o penetraciones en el 59%, siendo silentes el 50%. Se prescribió dieta adaptada al 56% y gastrostomía en 13 pacientes (21%). Se encontró asociación estadística entre enfermedad neurológica y la gravedad de la disfagia, existiendo relación según el grado de afectación motora y la presencia de aspiraciones. Tras la evaluación por VFC y la adecuación del tratamiento se encontró una mejoría nutricional en Z-score de peso (+0,3DE) e IMC (+0,4DE) y una mejoría respiratoria en un 71% de los pacientes disfágicos controlados en Neumología.
ConclusionesTras la implantación de la VFC se ha diagnosticado a un alto porcentaje de pacientes, que se han beneficiado de un diagnóstico y un tratamiento correctos. La VFC es una prueba diagnóstica fundamental que debería ser incluida en los centros pediátricos, como método diagnóstico de los niños con sospecha disfagia.
Dysphagia is defined as difficulty swallowing solid or liquid foods, and varies in severity depending on the underlying disease of the patient. In the paediatric age group, it is usually a functional disorder due to abnormalities in the motor actions of swallowing in children with neurologic impairment.1 Swallowing is a complex process that requires the coordination of the cranial nerves, brainstem and cortex as well as 26 muscles in the mouth, pharynx and oesophagus. Its function is the ingestion and transport of nutrients through the digestive tract as well as protection of the upper airway. Swallowing may be negatively affected by any abnormality in the nervous system or anatomical abnormalities in the mouth or pharynx. The action of swallowing can be divided into three stages: oral, pharyngeal and oesophageal. Thus, swallowing disorders can occur in any of these three stages and manifest clinically as dysphagia.2,3
The incidence of dysphagia may be as high as 80% in children with cerebral palsy and other developmental disorders, and dysphagia may lead to complications such as growth delay, recurrent respiratory infections, malnutrition, immune disorders, chronic disease and even death.4,5 Most children with cerebral palsy have some degree of dysphagia, usually oropharyngeal.6 Other health conditions may also cause oropharyngeal dysphagia, such as preterm birth, neuromuscular disorders, anatomical abnormalities of the oral cavity, orofacial surgery, presence of a feeding tube, mucositis and cardiorespiratory diseases, among others.7 The conditions associated with oesophageal dysfunction are mainly gastrointestinal, such as history of surgical correction of oesophageal atresia, achalasia or gastroesophageal reflux disease. The incidence of paediatric dysphagia has been gradually increasing due increases in the incidence of preterm birth and survival in children with cerebral palsy,8 two of the conditions in which the prevalence of dysphagia is highest.9,10
Dysphagia is diagnosed through a clinical evaluation and the use of diagnostic tools. Clinical feeding evaluations take into account objective parameters such as oxygen saturation, but also parameters whose assessment is more subjective and may vary between observers. Thus, there is a need for more accurate methods for diagnosis of dysphagia that can provide information on the involved stages and severity and guide the development of an individualised treatment plan.
Videofluoroscopy has emerged as a diagnostic technique and is currently considered the gold standard for diagnosis of oropharyngeal dysphagia. Several studies have highlighted the relevance of videofluoroscopy in the diagnosis and management of dysphagia in the paediatric population.11 It is a dynamic imaging technique that provides serial lateral views of the swallowing process as the patient ingests a contrast solution, which is delivered in boluses of different volumes and in three viscosities (thin liquid, nectar-thick and pudding-thick). The videofluoroscopic swallowing exam (VFSE) assesses the safety and effectiveness of swallowing, as well as signs of abnormalities in the three stages of swallowing. The following areas where swallowing problems may manifest are evaluated: labial seal, bolus formation, lingual-palatal seal, tongue movement, aspiration in the airway and presence of residues in the glottis. This technique can also be used to assess the effectiveness of the oral-motor therapy used to remedy identified swallowing problems and to adjust the management based on the recommended positioning or utensils.12
Patients received dietary recommendations and were offered speech therapy based on the severity of dysphagia observed during the test. Performance of gastrostomy was considered in cases of severe abnormalities where oral intake seemed unsafe.
The aim of our study was to analyse our experience in the diagnostic evaluation of dysphagia one year after the introduction of the VFSE in our hospital, and to assess clinical improvement in children with oropharyngeal and oesophageal dysphagia after the diagnosis was confirmed by videofluoroscopy as oral, pharyngeal and in some cases oesophageal and their management adjusted accordingly.
Patients and methodsWe conducted a cross-sectional descriptive study in 61 children with suspected dysphagia assessed by means of videofluoroscopy a year after this technique was introduced in the Hospital Infantil Miguel Servet of Zaragoza. Patients with suspected dysphagia were referred to the Paediatric Gastroenterology clinic for performance of a VFSE.
The VFSEs were performed with a Siemens AXIOM Iconos R200 series 4501 system, which can be used to obtain lateral views. During the assessment, patients remained seated on a chair positioned at 90° or, where necessary, on the lap of the mother or legal guardian. Patients received the contrast solution at the volumes and with the textures prescribed by the paediatrician, with every effort made to improve the comfort of the patient and the quality of the test. The VFSEs involved administration of boluses that contained a water-soluble contrast (Visipaque®), in 3 different textures achieved by mean of thickeners (thin liquid, nectar-thick and pudding-thick), and in 3 increasing volumes (3–5–10mL). Whenever aspiration was detected during the test, progression to a greater volume or a thicker texture was halted. We asked the families to bring the utensils that the child used to eat at home, as well as toys that may help soothe the child during the test.
Videofluoroscopy was performed under the ongoing supervision of a radiologist physically present in the room during the exam in order to minimise exposure to radiation, which has a significant impact on paediatric patients.
We classified dysphagia as oral, pharyngeal and in some cases oesophageal based on the effectiveness and safety of swallowing observed at each stage for each volume and texture administered during the test. We recorded every test with an external recorder to be able to review them later. Given the poor reliability reported in relation to the interpretation of VFSEs,13,14 we discussed our conclusions with the radiologist to improve the accuracy and validity of our results. To standardise the interpretation of results, we developed an evaluation form that was filled out for each VFSE.
We analysed data on the following variables: age, disease, nutritional assessment and anthropometric measurements, referring department, level of neurologic impairment assessed by means of the Gross Motor Function Classification System (GMFCS), type of dysphagia (oral, pharyngeal and/or oesophageal), severity of dysphagia, presence of aspiration and/or penetration, type of aspiration (silent or with a cough reflex), type of nutritional support after diagnosis, prescription of dietary adaptations, rehabilitation through speech therapy techniques and/or gastrostomy. We defined severe dysphagia as difficulty swallowing that made swallowing ineffective or unsafe with aspiration and/or penetration in the pharyngeal stage.
We collected anthropometric data for those patients that were followed up in the departments of paediatric gastroenterology and nutrition, whose weight and BMI, expressed as z-scores, were recorded before performance of the VFSE and 1 year after confirmation of the diagnosis by videofluoroscopy. We also collected data on respiratory manifestations for those patients followed up in the pulmonology clinic (36 patients), specifically the number of exacerbations and visits to the emergency department in the 6 months pre test and the 6 months post test.
We performed the statistical analysis with the software SPSS version 21. We assessed the normality of the variables under study by means of the Shapiro–Wilk and Kolmogorov–Smirnov tests. In the bivariate statistical analysis, we compared the categorical exposure variable (2 categories) with continuous outcome variables by means of the Student t test if the variable was normally distributed or otherwise by means of the Mann–Whitney U test. We analysed associations between 2 continuous variables by the nonparametric Spearman rank-order correlation test.
ResultsIn the 12 months since the introduction of videofluoroscopy, a total of 61 VFSEs were performed. Sixty-six percent corresponded to patients with neurologic disease (cerebral palsy or hypotonia), 13% to patients with respiratory complaints of a non-neurologic aetiology, such as pulmonary dysplasia or severe asthma with suspected choking or dysphagia, and 21% to children referred for gastrointestinal problems at the level of the oesophagus, such as oesophageal atresia or severe gastroesophageal reflux with episodes of choking. Most of the patients were referred from the departments of paediatric gastroenterology (36%) and pulmonology (33%), as the digestive and respiratory systems are the systems most affected by the nutritional and respiratory consequences of swallowing disorders. The rest of the patients were referred from the paediatric neurology, neonatal and otorhinolaryngology units. Table 1 summarises the most relevant characteristics of the patients.
The VFSE detected swallowing disorders in more than 70% of the patients, of moderate to high severity in 58%.
We found abnormalities in the oral stage in half of the patients, with changes in the labial seal, chewing and/or bolus formation; pharyngeal dysphagia in 67% of patients, with impaired closure of the larynx and/or velopharyngeal port or impaired opening of the upper oesophageal sphincter, which pose a risk of aspiration; and oesophageal dysphagia with abnormal oesophageal motility in 3% of patients.
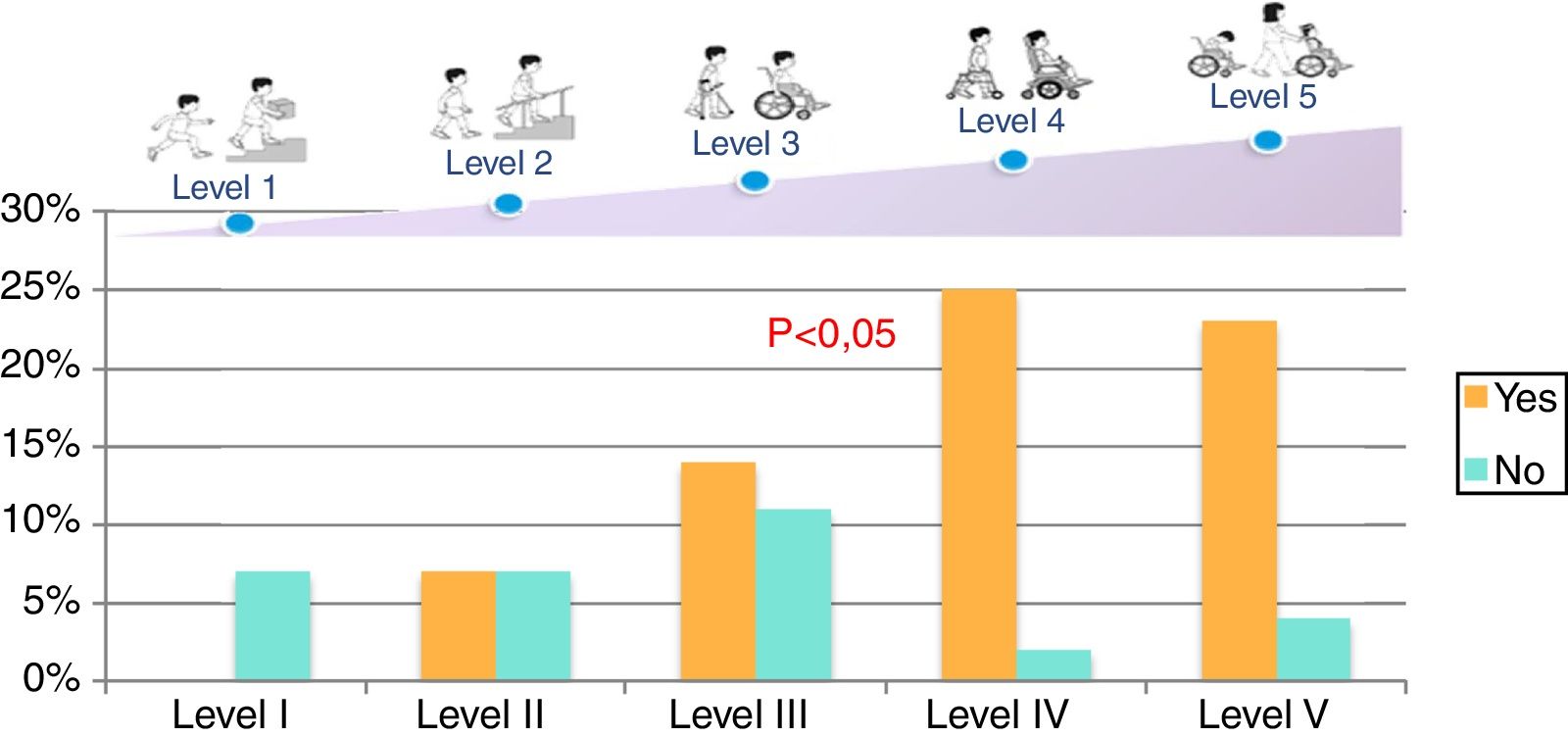
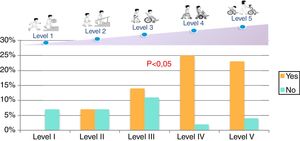
One of the most important elements of the VFSE is the visual assessment of aspiration or penetration, which were detected in 59% of the patients. Of these patients, half presented with silent aspiration that could only be detected by VFC, as it was not accompanied by coughing or choking. All patients with silent aspiration had moderate to severe cerebral palsy (GMFCS IV and V).
The most frequent type of dysphagia detected in our study was pharyngeal, with presence of residues in the epiglottic vallecula and piriform fossae associated with abnormalities that affected safety (aspiration and/or penetration) in 60.5% of the sample.
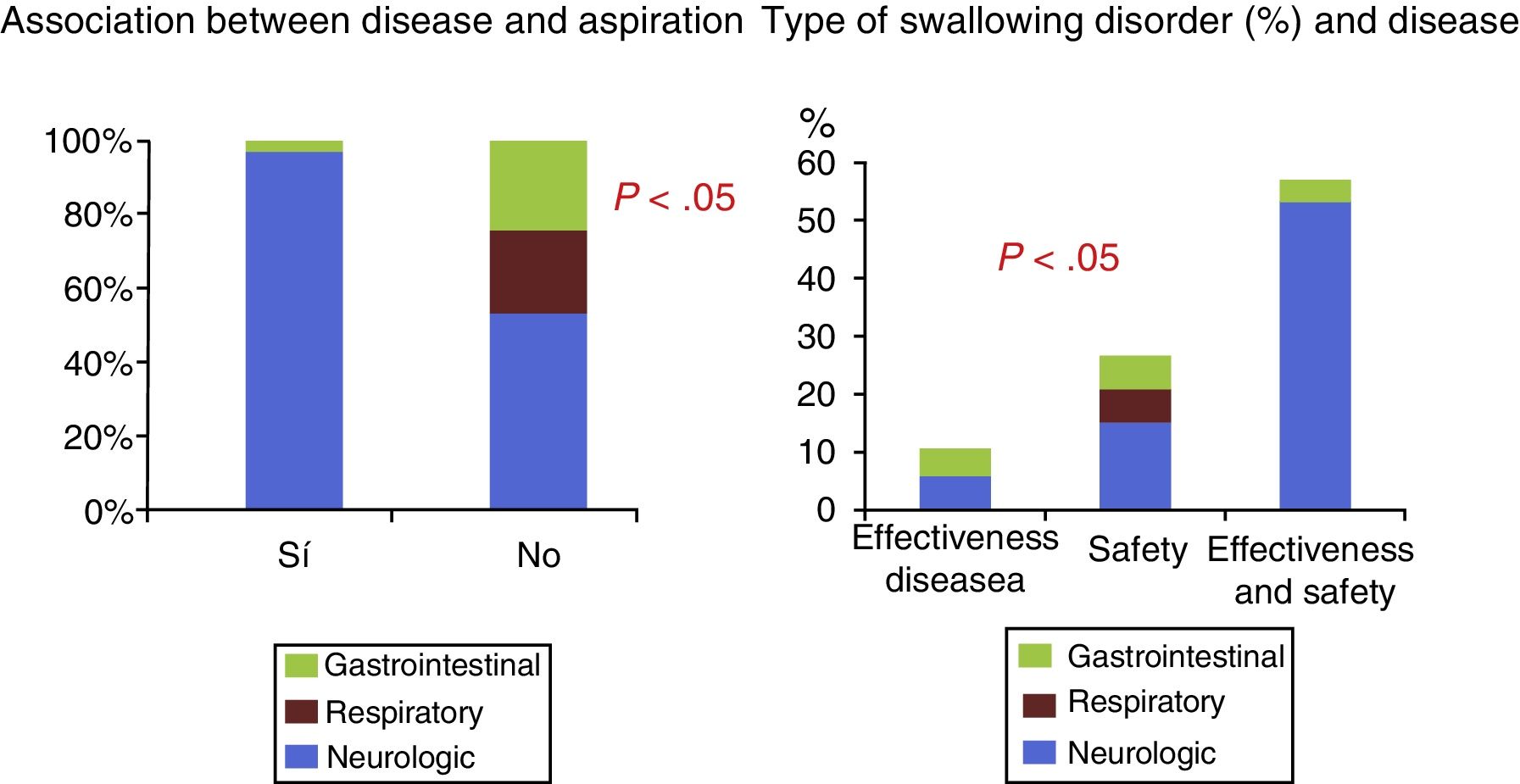
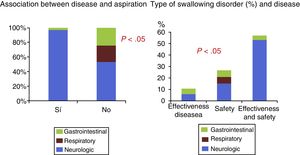
We assessed the association between aspiration and the disease that led to referral of the patient, and found a significantly greater proportion of dysphagia in patients with neurologic impairment compared to patients referred for assessment of gastrointestinal or respiratory problems (P<.05).
Severe dysphagia was defined as abnormal swallowing with decreased effectiveness or safety and presence of aspiration and/or penetration in the pharyngeal stage. We also found a statistically significant association between the severity of dysphagia and the disease that led to patient referral, with greater frequency of severe dysphagia in neurologic patients (P<.05) (Fig. 1). When we studied the type of swallowing abnormality—ineffective swallowing, unsafe swallowing or both—we found that patients with neurologic impairment frequently had both problems at once (P<.05).
We also found a significant and positive association between the level of motor impairment (GMFCS) and the risk of aspiration (P<.05) (Fig. 2).
When it came to treatment following the VFSE, dietary adaptations with use of safer textures was prescribed to 56% of the patients. Gastrostomy tube feeding was recommended to children with severe dysphagia that precluded safe feeding regardless of food consistency (13 patients; 21%); 2 patients already had feeding tubes in place before testing (24% of gastrostomies), and we found a statistically significant association between the indication of gastrostomy and the severity of dysphagia (Table 2).
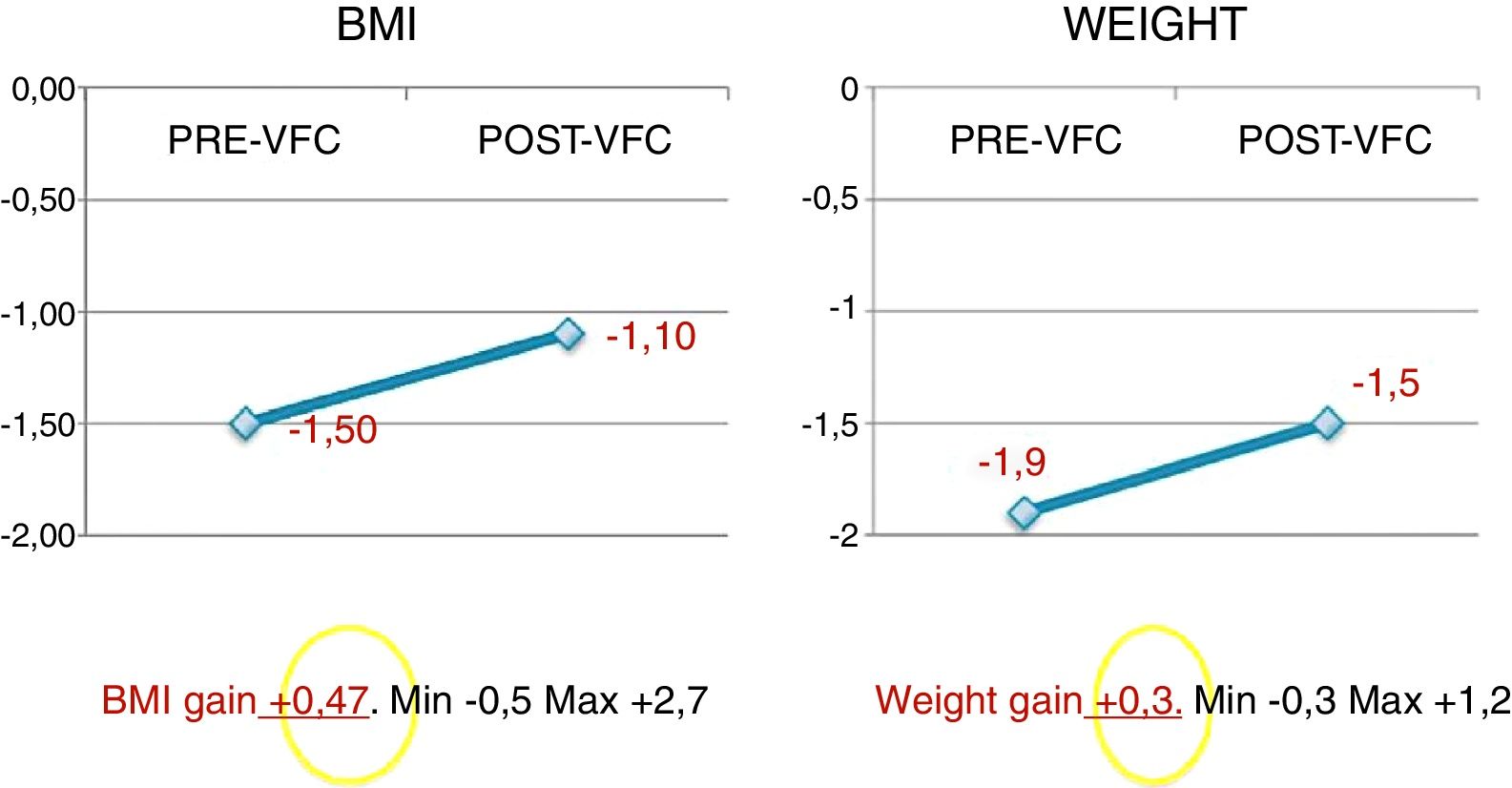
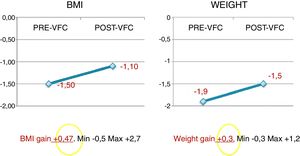
In the 21 patients that received a diagnosis of dysphagia for which we had pre-test anthropometric data, the assessment at 12 months after diagnostic confirmation by videofluoroscopy revealed improvements in weight (0.3 increase in the mean weight z-score) and BMI (0.4 increase in mean BMI z-score) (Fig. 3). In the patients that had been followed up in the paediatric pulmonology department (n=36), we found improved respiratory outcomes in 76%, with improvement defined as a decrease in the number of exacerbations and visits to the emergency department in the 6 months post test compared to the 6 months pre test.
DiscussionIn the paediatric age group, swallowing disorders may result in clinically severe complications and affect overall growth and development.15 The prevalence of cerebral palsy in children has increased in recent years, mostly due to the increased survival in neonatal units. Our study found a significantly greater prevalence of dysphagia in patients with neurologic impairment compared to patients with other diseases and suspected swallowing disorders, as well as more severe dysphagia in neurologic patients. An epidemiological study of 1357 children with cerebral palsy found dysphagia of varying severity in 43% of the children,16 and Prasse and Kikano3 noted that children with developmental abnormalities are at high risk of developing dysphagia. The prevalence of aspiration in our study was 59%, similar to the data reported in the literature,17 with some studies reporting a prevalence of up to 70% in children with severe forms of cerebral palsy.18,19 Thus, oropharyngeal dysphagia should be suspected and assessed in children with cerebral palsy, especially those with GMFCS levels III, IV and V,20 an approach that was also supported by the data in our study.
In a study that included 44 children with cerebral palsy, Field et al. found oral motor delays in 68% of these patients and suspected aspiration, based on the symptoms reported by caregivers, in 32%.21 Since our study found evidence of silent aspiration in 50% of patients with pharyngeal dysphagia, in agreement with the findings of previous studies,6 we believe that it is essential to substantiate any suspected diagnosis of dysphagia by an objective assessment of swallowing, such as a VFSE. This technique is considered the gold standard of diagnosis, but it is available in very few facilities. In addition to confirming the diagnosis, it can detect silent aspiration, which may go unnoticed because it does not produce symptoms or episodes of oxygen desaturation but may lead to respiratory tract infections in patients with neurologic impairment.22 Clinicians should be well acquainted with the technique and the different radiologic signs associated with dysphagia in order to make an accurate diagnosis and plan nutritional and speech therapy interventions.
The impact of swallowing disorders is variable. They may lead to malnutrition, dehydration, recurrent respiratory problems or chronic respiratory diseases, seriously impairing the health of the child, slowing down recovery and in extreme cases, posing a risk to the patient's life. In our study, we found improved nutritional and respiratory outcomes after confirmation of the dysphagia diagnosis. In cases where the patient cannot ingest enough calories by mouth or has severe dysphagia, gastrostomy is the first-line treatment.23 The volume and texture of the foods to be administered to the patient are determined based on the results of the VFSE,24 as are the speech therapy interventions for rehabilitation of patients with mild to moderate dysphagia.
Until 2014, no diagnostic methods were available in Aragón, and paediatric patients with swallowing disorders needed to seek resources outside this autonomous community. The implementation of the VFSE was difficult, as no device was available at our children's hospital to obtain lateral views, so the test was introduced by collaborating with the radiology facilities of the general hospital. To minimise radiation exposure in the patient, we recorded the tests with a privately-owned external device, as the budget did not allow the purchase of additional equipment.
However, despite the barriers to the implementation of the VFSE, we found evidence that in the year that followed its introduction, testing allowed the rehabilitation of a significant number of children, who showed improvement in nutritional and respiratory outcomes. This required the close collaboration of all the professionals involved in the management of these children. Although a gastroenterologist or nutritionist may be mainly responsible for the patient, the treatment plan should be developed by a multidisciplinary team including a paediatric neurologist, occupational therapist, speech therapist and dietitian, among others.25 Along the same lines, Lefton-Greif and Arvedson noted that the evaluations of children with feeding and swallowing disorders are performed by different specialists, such as pulmonologists, gastroenterologists, paediatricians, ear, nose and throat specialists and radiologists.26 At present, there is a paucity of data regarding the approach to dysphagia, for instance, in terms of the professionals that manage dysphagia, the procedures used in its evaluation, the different types of swallowing disorders and the professionals involved in rehabilitation. The approach to dysphagia may be different in each paediatric care setting. We believe that the role of the gastroenterologist in the multidisciplinary team is important in the identification of dysphagia, the confirmation of the diagnosis and the followup of nutritional complications with the purpose of ensuring an adequate oral intake of fluids and nutrients while minimising the risk of aspiration.
The main limitations of our study are its retrospective design, due to which we were unable to assess nutritional and respiratory improvement in all patients, as this was only possible in those that had been followed up previously in the nutrition and pulmonology clinics.
In conclusion, early detection and adequate management of swallowing disorders in children can prevent significant complications, which is not only important from a clinical or quality of life standpoint, but also from an economic standpoint, as this is associated with a decrease in hospital admissions and emergency department visits, as evinced by our review.
The training of health professionals in the diagnosis and treatment of paediatric dysphagia and its complications and the development of clinical screening tools, specific diagnostic tests and dietary measures to prevent aspiration and malnutrition are the key aspects that must be pursued to maximise recovery in paediatric patients with oropharyngeal dysphagia.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: García Romero R, Ros Arnal I, Romea Montañés MJ, López Calahorra JA, Gutiérrez Alonso C, Izquierdo Hernández B, et al. Evaluación de la disfagia. Resultados tras un año de la incorporación de la videofluoroscopia en nuestro centro. An Pediatr (Barc). 2018;89:92–97.