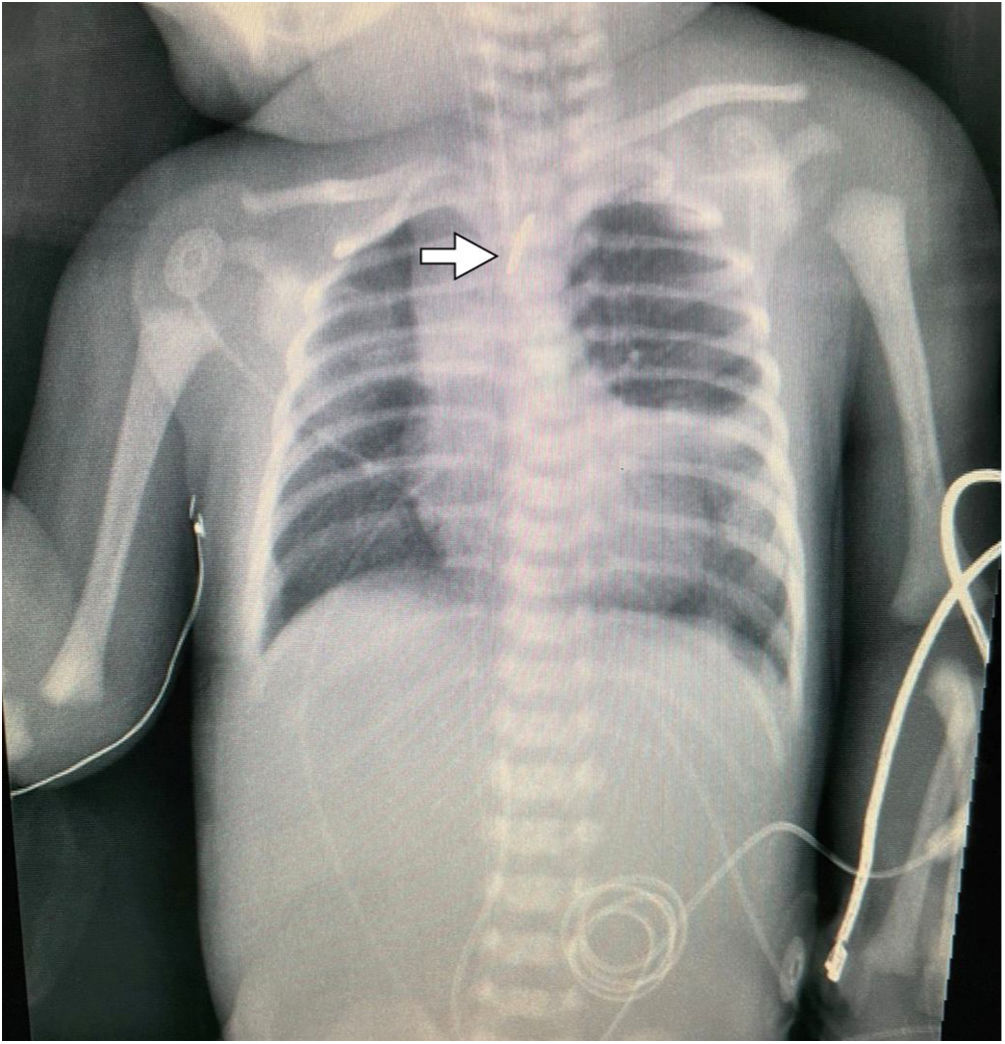
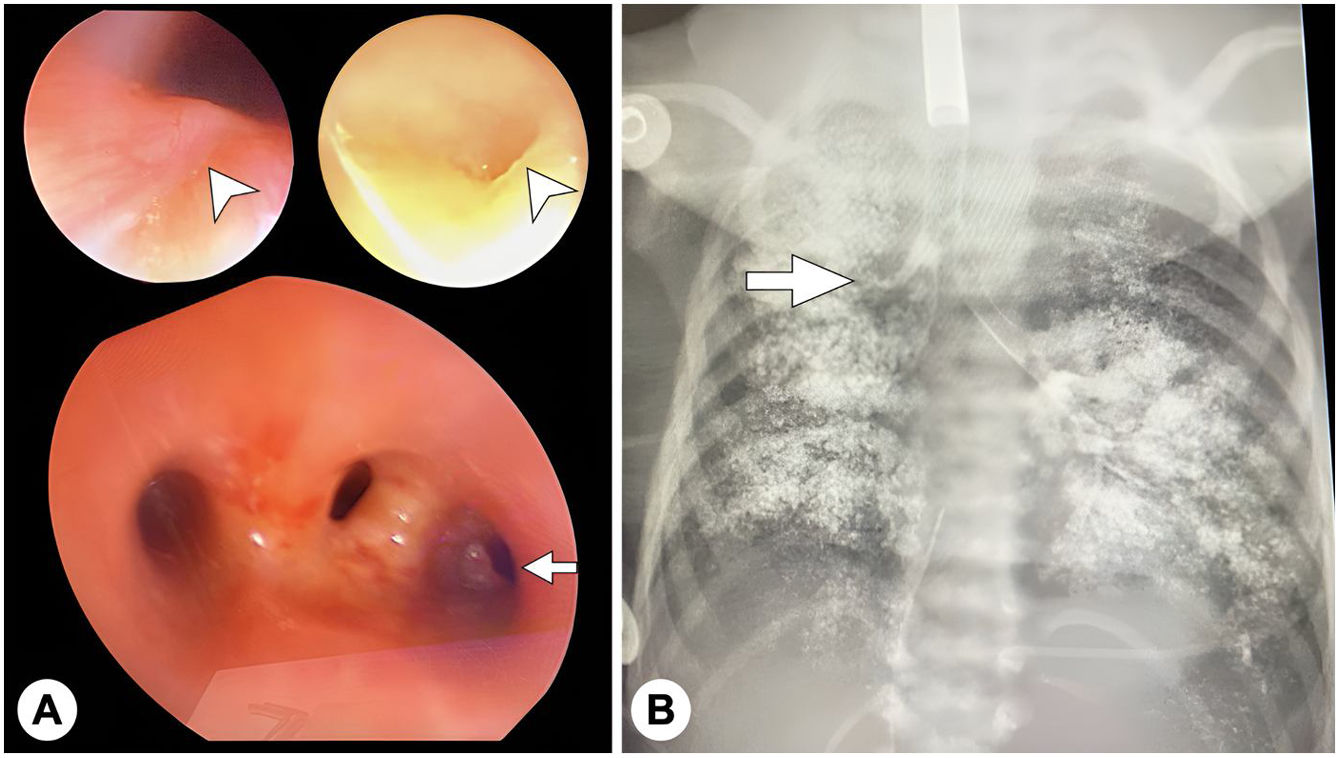
We present the case of a female term newborn aged 2 days with a history of severe polyhydramnios referred for management of oesophageal atresia (OA) (Fig. 1). Once additional malformations had been ruled out, a bronchoscopic examination was performed, revealing a diverticulum in the posterior wall of the trachea and a third opening next to the carina (Fig. 2A). Given the absence of air in the abdomen suggesting the presence of tracheo-oesophageal fistula (TOF), water-soluble contrast material was injected through the opening, leading to identification of a tracheal bronchus associated with OA type I (Fig. 2B; Appendix B video), followed by gastrostomy. The patient is currently awaiting oesophageal anastomosis, and has remained free of respiratory symptoms.
(A) Bronchoscopy images showing a subtle mucosal fold in the middle third and posterior wall of the trachea concealing a diverticulum measuring at least 1cm in diameter (arrowhead) and image showing tracheal trifurcation with an ectopic opening in the right lateral wall of the trachea (arrow). (B) The injection of contrast material evinced a tracheal bronchus that ended in the right upper lobe (arrow), ruling out tracheo-oesophageal fistula.
The incidence of OA is of 1 case per 4000 live births, and in 37% of cases OA is associated with intrathoracic malformations. In the respiratory tract, TOF is the most frequent anomaly (84%–90%), but OA may also be associated with lobar agenesis or pulmonary aplasia, among others.1 To date, few cases of tracheal bronchus in the context of OA have been reported in the literature (≈4%), and, to our knowledge, none associated with tracheal diverticulum.1,2 Tracheal bronchus can be confused with TOF in the bronchoscopic examination, so it is important to assess the severity of polyhydramnios and the presence of air in the abdominal cavity.3 Contrast-enhanced imaging may be useful in such cases. The usefulness of preoperative 3D computed tomography reconstruction has also been studied in these patients, as this technique could allow the identification of undetected malformations, but has not been found to have a significant impact in surgical planning while exposing the patient to high doses of ionising radiation (mean, 1.79 mSv).4
We thank Katherine Bautista (MD), María Lourdes Meléndez (MD), Miguel Astudillo (MD) and Alex Vásquez (MD) for their collaboration in image acquisition and the surgical management of the patient.