Every year, there are more than 200000 new cases of viral encephalitis worldwide, and enteroviruses (EVs) are the main causative agents. Traditionally, a diagnosis of infection by EV, such as herpangina or hand, foot and mouth disease (HFMD) was a source of relief in the evaluation of children with aseptic meningoencephalitis due to its generally good prognosis.
This perspective has changed after several epidemics by EV in different parts of the world evinced that a significant number of patients develop neurologic manifestations, with a mortality and incidence of sequelae that are far from insignificant. Enteroviruses are single-stranded RNA viruses that belong to the Picornaviridae family. There are more than one hundred serotypes that exhibit variable degrees of neurotropism, as demonstrated by the damage inflicted by poliomyelitis, which has been eradicated in most of the world at this point. Enterovirus infections, including those by poliovirus, are asymptomatic in most cases. They spread by the faecal–oral route and by respiratory droplets. There are two main serotypes that can cause neurologic complications and have caused public alarm in Spain in the past year: enterovirus 71 (EV-71) type A71, and enterovirus D68 (EV-D68).
Enterovirus 71 was identified in 1969, and in four decades it has given rise to outbreaks in Eastern Europe, Asia, Oceania and the United States, leading to considerable mortality in all instances. Suffice it to say that of the 130000 cases of infection by EV-71 in Taiwan in 1998, 405 led to severe neurologic complications and 78 to death in children, and that more than seven million cases of HFMD were diagnosed in China between 2008 and 2012, with 2457 cases resulting in death.1 There is a reason that EV-71 is referred to as “the polio of the 21st century.”
Enterovirus D68 is an emerging pathogen worldwide. First identified in 1962, the incidence of respiratory infection by EV-D68 has increased in recent years, and the virus has been associated with cases of acute flaccid paralysis in the United States and Canada.2 While EV-71 primarily affects children aged 1–2 years (approximate range, 3 months–5 years),3 EV-D68 affects older children and adults, who in many cases suffer from asthma.
Neurologic disease associated with enterovirus 71There are four clinical stages of infection by EV-71: 1) HFMD/herpangina, 2) central nervous system involvement, 3) cardiopulmonary failure and 4) convalescence. Most cases resolve during stage 1, some progress to stage 2, few progress to stage 3 and, if the latter patients survive, they may suffer permanent sequelae, which would correspond to stage 4. The typical presentation is brainstem encephalitis with or without myelitis, or, in some cases, pure myelitis (acute flaccid paralysis). In addition to manifesting with fever, mild forms of brainstem encephalitis may be associated with drowsiness, myoclonus and/or tremors. Ataxia, when present, is mild and transient, as occurs in other acute post-infectious ataxias in children. Stretch reflexes are usually overactive. In moderate forms, patients also experience weakness and manifestations of bulbar involvement (dysarthria, dysphagia, hypopnoea) or involvement of other cranial nerves (VI, VII), while severe disease manifests with cardiopulmonary failure, acute haemorrhagic pulmonary oedema of neurologic origin and/or myocarditis. Given the rapid progression of the latter forms and that most deaths occur within the first 24h, it is crucial that brainstem encephalitis secondary to EV-71 infection is diagnosed early and followed by immediate initiation of monitoring and supportive care. It is important that providers recognise myclonic jerks, as they are an early sign of brainstem involvement.
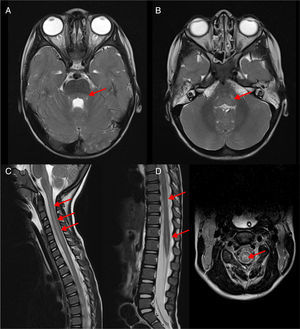
Neuroimaging tests show involvement of the dorsal region of the pons, medulla, midbrain and dentate nuclei, with hyperintense foci in T2-weighted and FLAIR images. Cases of flaccid myelitis manifest with hyperintensity in the anterior horn of the spinal cord. The presence of restriction patterns in diffusion-weighted images is associated with severe forms of disease and increased risk of sequelae.
In 2016, more than 100 cases of EV-71 encephalitis were reported in Spain. Since the definition of a case is, as one would expect, quite strict (confirmation by virology testing and positive findings in neuroimaging, which in our experience can be subtle or even negative) it is likely that the actual number of cases is underestimated.
Of the 45 patients that received the diagnosis in our hospital between March and July 2016, all with rhombencephalitis experienced a complete or nearly full recovery, two out of four with acute flaccid paralysis suffer from monoparesis as a sequela, and a patient with fulminant brainstem failure and heart abnormalities suffers from severe sequelae. Only one patient died in the Autonomous Community of Catalonia, in September 2016.
Neurologic disease associated with enterovirus D68Neurologic disease associated to infection by EV-D68 is different and less frequent (5 confirmed cases since late 2015 in Spain). However, it has been widely covered by the media due to its severity, comparable to that of poliomyelitis. Its manifestations often complicate lower respiratory tract infections. The clinical presentation consists of acute flaccid paralysis and arreflexia. Neuroimaging (Fig. 1) reveals longitudinally extensive myelitis with predominant involvement of the anterior horn. Features of rhombencephalon involvement are indistinguishable from those caused by EV-71. Electromyography can confirm motor neuron damage at one week from onset and signs of denervation at three to four weeks. The prognosis is very poor, with a high mortality and variable degrees of flaccid tetraparesis and involvement of respiratory muscles.
Rhombencephalitis caused by EV-D68: T2-weighted brain and spinal cord MRI scans obtained during the acute phase of disease. The arrows point at dorsal involvement at the level of the pontine (A) and bulbar tegmentum (B) as well as the entire medulla oblongata (C) with grey matter predominance (D) (Courtesy of Ignacio Delgado, Radiology Dept.).
Early diagnosis is paramount. The pharynx must be assessed for the presence of EV within one week from the onset of symptoms, and the faeces two weeks or more later. The findings of cerebrospinal fluid examination are abnormal in only five to twenty percent of cases. Rapid detection of EV can be achieved by means of real time PCR and serotyping by sequencing of the 5′UTR region of the virus (VP1). CSF examination may reveal mild pleocytosis and elevated protein levels, or it may be normal. In fatal cases, the viral antigen has been detected in nerve roots, autonomic ganglia in the intestines, and nuclei of the brainstem and spinal cord.4 It is known that human cells have receptors for EV-71. Host-related factors (polymorphisms in interleukin genes) or certain serotypes that can evade innate immunity could contribute to the susceptibility to severe disease.
There is no specific treatment for EV. The good outcomes achieved with pleconaril in a clinical trial in newborn infants await replication. Administration of intravenous immunoglobulin may be somewhat beneficial by contributing neutralising antibodies, attenuating sympathetic activity and reducing cytokine production, but a recently published study did not find high-dose methylprednisolone to be effective in any way,5 which is consistent with our own experience. In cases with cardiac dysfunction, milrinone is the drug of choice due to its inotropic, vasodilatory and anti-inflammatory effects. Fluoxetine has exhibited an anti-EV activity in vitro and was used off-label in some of our patients, with no apparent effect (it has also been used for the treatment of enterovirus encephalitis in patients with sex-linked hypogammaglobulinaemia). In China, phase III clinical trials of inactivated whole-virus vaccines have been completed, demonstrating that the vaccines are efficacious against EV-71 but offer no cross-protection against other genotypes.
ConclusionsThe experience in other countries shows that EV epidemics can be protracted, and thus, as paediatricians, we must remain alert in the coming months and possibly years. Neuroimaging tests must be performed early in patients presenting with acute neurologic symptoms and on an urgent basis in cases of bulbar palsy or acute flaccid myelitis. All cases of acute flaccid paralysis must be reported by law, and the potential presence of EV must always be assessed. As long as a vaccine is not available, the early detection of outbreaks and the implementation of hygiene measures to stop the spread of EV are the key steps to limit the impact of outbreaks and the development of severe forms of disease. In this regard, educational campaigns on hygiene measures not only in the community, but also in the health field, are of utmost importance.
Please cite this article as: Macaya A, Felipe-Rucián A. Enterovirus y complicaciones neurológicas. An Pediatr (Barc). 2017;86:107–109.