Sunburn, immunodepression, photoaging, and photocarcinogenesis, are some of the most significant adverse effects of solar radiation in humans. Children are a population group of special vulnerability, due to the fact that exposure to the sun has more pronounced biological effects compared to adults. Furthermore, childhood is a critical period for promoting the development of photo damage and photocarcinogenesis in the later stages of life if adequate measures are not put into place. This is because it is estimated that between 18 and 20 years of age 40–50% of the accumulative exposure to ultraviolet radiation up to 60 years of age is received. The most important strategy for the photoprotection of children is changes in behaviour and habits associated with exposure to the sun at all levels (school, society, family, etc.). Resorting to the shade, reduction in overall time of exposure to the sun, and physical protection (clothes, hats, and sunglasses) are the best and least costly photoprotection strategies. The photoprotectors must be incorporated into the daily routine of children in the same way as adults, and must complete a series of requirements in order to make them effective, safe, and in line with the environment.
Las quemaduras solares, la inmunodepresión, el fotoenvejecimiento y la fotocarcinogénesis son algunos de los efectos adversos más importantes de la radiación solar en el ser humano. Los niños son un grupo poblacional de especial vulnerabilidad debido a que en ellos la exposición solar tiene efectos biológicos más pronunciados en comparación con los adultos. Por otro lado, la infancia es un periodo crítico para promover el desarrollo de fotodaño y fotocarcinogénesis en etapas más tardías de la vida si no se ponen las medidas adecuadas, ya que se estima que entre los 18 y 20 años de edad se recibe del 40-50% de la exposición acumulativa a la radiación ultravioleta hasta la edad de 60 años. La estrategia más importante para la fotoprotección de los niños son las modificaciones de comportamiento y hábitos relacionados con la exposición al sol a todos los niveles (colegio, sociedad, familia, etc.). El recurso de la sombra, la reducción del tiempo global de exposición al sol y la protección física (ropa, sombreros y gafas de sol) representan las mejores y menos costosas estrategias de fotoprotección. Los fotoprotectores deben incorporarse a la rutina diaria de los niños, de la misma manera que los adultos, y deben cumplir una serie de requisitos que los hagan eficaces, seguros y comprometidos con el medio ambiente.
The sun is a large source of energy that makes life possible on Earth. But the effects of solar radiation on humans may have a significant impact on health.
Sunburns,1 photosensitivity, photodermatoses, immunosuppression, photoaging and photocarcinogenesis are some of the most important adverse effects. According to the World Health Organisation, skin cancer is the most frequent type of cancer worldwide and the incidence of melanoma is increasing faster than the incidence of any other type of malignant tumour.
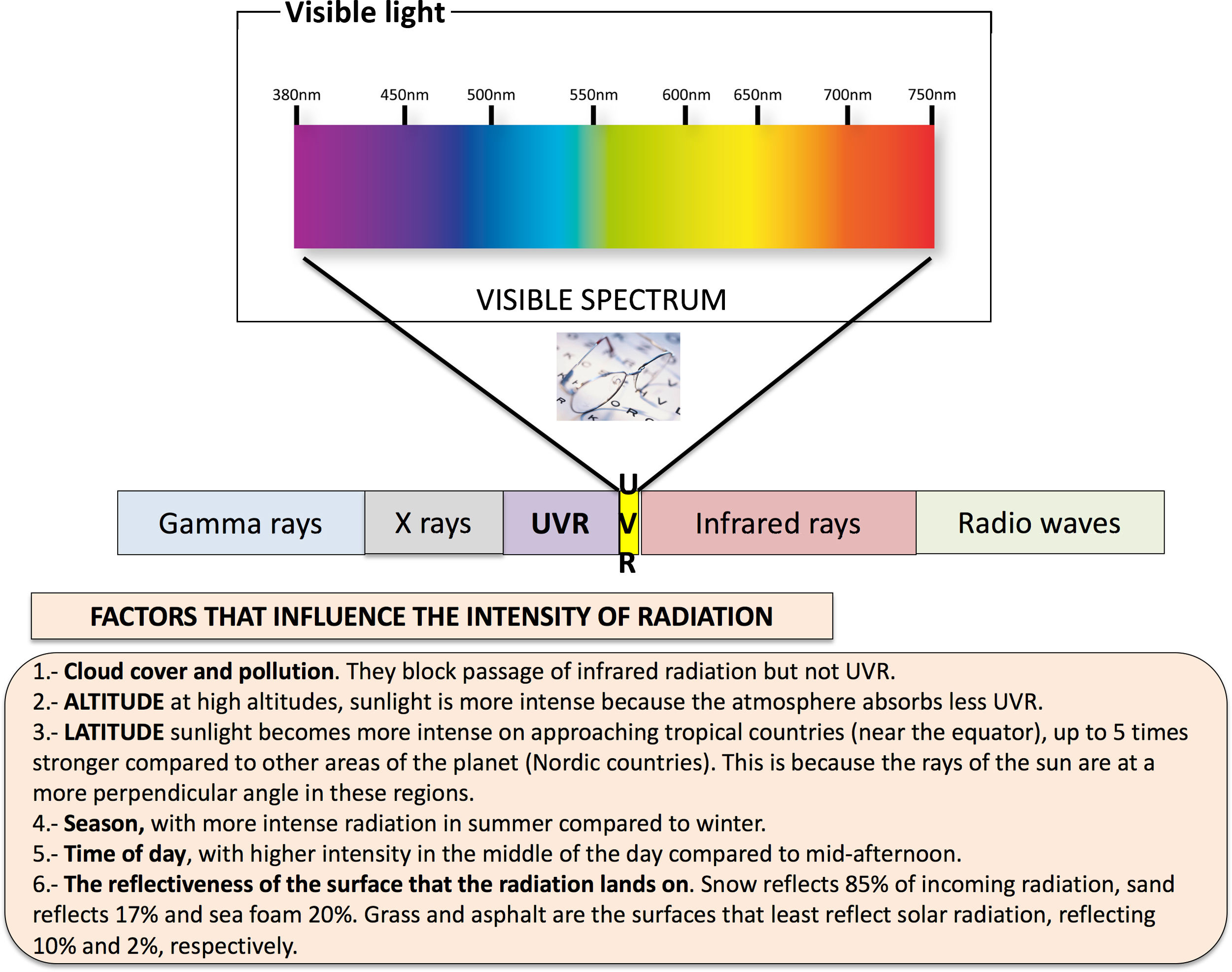
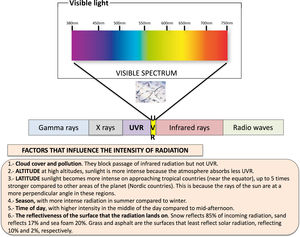
Only part of the broad electromagnetic radiation spectrum emitted by the sun reaches the surface of the Earth (Fig. 1).2 Nearly 5% correspond to ultraviolet A (UVA) radiation and 0.5% to ultraviolet B (UVB) radiation. Most of the radiation that reaches us from the sun is in the infrared (IR) spectrum. Lastly, there is an increasing awareness of the importance of visible light, especially its high-intensity blue light component, present in electronic devices.
Electromagnetic spectrum represented from the shortest wavelengths, such as gamma rays and X rays, through ultraviolet radiation, visible light and infrared radiation to the longest wavelengths, such as radio waves. The electromagnetic radiation from the sun that reaches the Earth includes ultraviolet UVA and UVB rays, infrared radiation and visible light. Summary of factors that influence the intensity of radiation.
Ultraviolet radiation in sunlight is composed of UVA (315–400nm), UVB (280–315nm) and UVC (100–280nm) radiation, classified according to wavelength. Since the ozone layer in the stratosphere completely blocks UVC radiation and radiation at wavelengths of less than 295nm, most of the UVR that reaches the Earth is UVA or UVB radiation.
Between 5% and 10% of the UVR that reaches the surface of the planet is high-energy radiation. It can penetrate the epidermis and part of the dermis (only 10%), but it cannot reach as deep into the skin as UVA radiation.
Between 90% and 95% of the UVR that reaches the surface is lower-energy light compared to UVB radiation, but it can penetrate deeper into the dermis (50%). It is further subdivided into short-wavelength UVA, or UVA II (320–340nm) and long-wavelength UVA, or UVA I (340–400nm). It is not filtered by glass, exhibits little temporal fluctuation and is hardly affected by altitude or weather conditions.
The intensity of UVR varies depending on several factors (Fig. 1) and is measured with the ultraviolet index (UVI),3 which can be consulted any time at the Agencia Estatal de Meteorología (State Meteorological Agency of Spain, AEMET) or even with the use of mobile applications such as UVIMate that not only provides the UVI for the specified location, but also offers UVI forecasts by the hour, explains the potential consequences of sunlight exposure and sunburn and has an alarm feature to warn the user when it is time to reapply sunscreen.
Effects and consequences of exposure to solar radiation in childrenThe effects of solar radiation on the skin are well known (Table 1), but its biological effects on the skin of children4 are more pronounced compared to adults,5 making the paediatric population a particularly vulnerable group.
- 1.
The skin of children, especially those aged less than 3 years, has a lower concentration of protective melanin and a thinner stratum corneum,6 which allows UVR to penetrate deeper and promotes photoimmunosuppression.
- 2.
The basal layer is relatively rich in stem cells, which are susceptible to the mutations induced by UVR.
- 3.
Children tend to get sunburnt more easily than adults due to their thinner skin and its greater percutaneous absorption and transepidermal water loss.
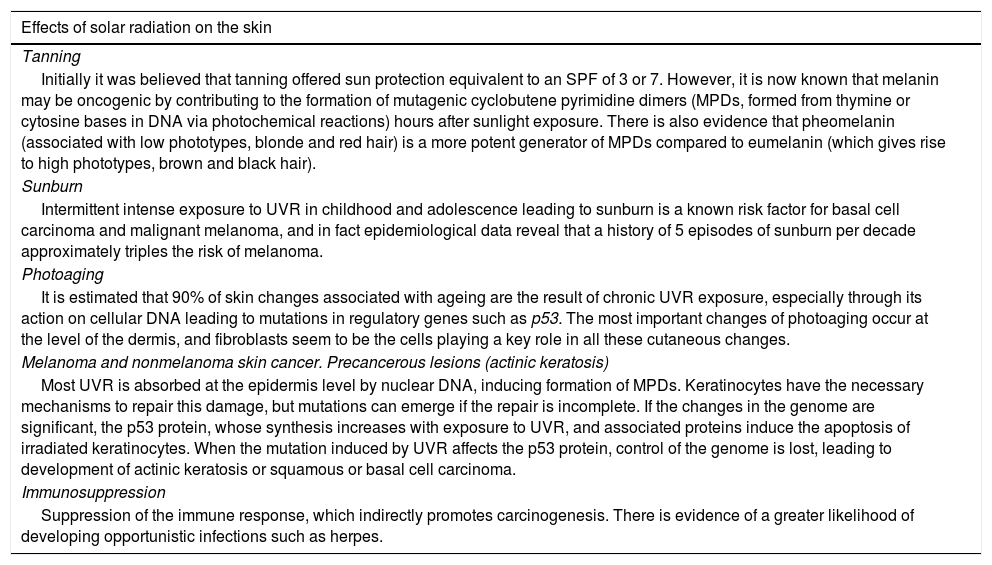
Summary of the effects of sunlight exposure on the skin.
| Effects of solar radiation on the skin |
|---|
| Tanning |
| Initially it was believed that tanning offered sun protection equivalent to an SPF of 3 or 7. However, it is now known that melanin may be oncogenic by contributing to the formation of mutagenic cyclobutene pyrimidine dimers (MPDs, formed from thymine or cytosine bases in DNA via photochemical reactions) hours after sunlight exposure. There is also evidence that pheomelanin (associated with low phototypes, blonde and red hair) is a more potent generator of MPDs compared to eumelanin (which gives rise to high phototypes, brown and black hair). |
| Sunburn |
| Intermittent intense exposure to UVR in childhood and adolescence leading to sunburn is a known risk factor for basal cell carcinoma and malignant melanoma, and in fact epidemiological data reveal that a history of 5 episodes of sunburn per decade approximately triples the risk of melanoma. |
| Photoaging |
| It is estimated that 90% of skin changes associated with ageing are the result of chronic UVR exposure, especially through its action on cellular DNA leading to mutations in regulatory genes such as p53. The most important changes of photoaging occur at the level of the dermis, and fibroblasts seem to be the cells playing a key role in all these cutaneous changes. |
| Melanoma and nonmelanoma skin cancer. Precancerous lesions (actinic keratosis) |
| Most UVR is absorbed at the epidermis level by nuclear DNA, inducing formation of MPDs. Keratinocytes have the necessary mechanisms to repair this damage, but mutations can emerge if the repair is incomplete. If the changes in the genome are significant, the p53 protein, whose synthesis increases with exposure to UVR, and associated proteins induce the apoptosis of irradiated keratinocytes. When the mutation induced by UVR affects the p53 protein, control of the genome is lost, leading to development of actinic keratosis or squamous or basal cell carcinoma. |
| Immunosuppression |
| Suppression of the immune response, which indirectly promotes carcinogenesis. There is evidence of a greater likelihood of developing opportunistic infections such as herpes. |
On the other hand, exposure to UVR in childhood plays a critical role in the development of photodamage and photocarcinogenesis later in life.7
A systematic review and meta-analysis of 51 studies concluded that a single instance of sunburn during childhood nearly doubles the risk of developing melanoma in adulthood.8
Studies of individuals that migrated to Australia have shown that moving to regions with more intense UVR in the first 10 years of life is associated with an increased risk of developing skin cancer with the same frequency as children born in Australia.9
When it comes to individuals that use tanning beds, there is evidence of an increased risk of developing basal cell carcinoma in those that started using them in the first and second decades of life compared to those that started using them between ages 25 and 35 years.10
It has been estimated that the regular use of sunscreen in the first 18 years of life can reduce the incidence of squamous cell carcinoma of the skin by 78%.11
Based on a systematic review of 29 studies conducted in Australia, Europe, Japan, Mexico, United Kingdom and the United States of America, children and adolescents spend an average of 1.5–5h outdoors each day.12 It is estimated that between ages 18 and 20 years, they will have undergone 40–50% of their cumulative exposure to UVR through age 60 years.
Several published studies on children have proven that the use of sunscreens can prevent the development of melanocytic nevi, which are strongly associated to the development of skin melanoma.13
Photoprotective measuresThe most important photoprotective measures14 for children are changes in behaviours and habits related to sunlight exposure at every level (school, society, family, …). Using shade as a resource, reducing the overall time of sunlight exposure, especially in the middle of the day (12:00 to 16:00) and physical barrier protection measures (clothing, hats and sunglasses) are the best and least expensive photoprotection strategies. Sunscreen should be integrated in the daily routine of children as much as in the routine of adults, taking into account that the use of sunscreen is meant to minimise skin damage associated to UVR exposure, but should not be considered a means to increase the duration of exposure to sunlight.
Physical barrier photoprotection (clothing, hats and sunglasses)Several studies15 have demonstrated that wearing protective clothing can decrease the number of melanocytic nevi developed by individuals. However, not every fabric provides adequate photoprotection. The ultraviolet protection factor (UPF) depends on the type and density of the fabric, the colour, design and processes used to finish the fabric. Thus, the use of dyes, especially dark ones, in thick material increases the protection afforded by a fabric by a factor of 3–5. In addition, the UPF of clothing is influenced by the shrinking, stretching and humidity of the fibres as well as the number of wash cycles. Lycra and elastane are the fabrics with a UPF of 50 or greater, followed by plastic, nylon and polyester.
Is specific sun-protective clothing better compared to regular clothing?Few published studies16 have compared the photoprotection of normal clothes to the photoprotection of sun-protective clothing, also known as UPF clothing. Broadly speaking, the latter is designed to be lighter and more breathable, which makes it an ideal option for summer and outdoor physical activity. While some everyday garments, such as jeans, provide a high UPF, they are not practical choices for physical activity.
Hats and caps provide a good physical barrier to protect the face and neck from sunlight. Small brims, less than 2.5cm in length, offer little protection and only to parts of the face, while wider brims, longer than 7.5cm, protect the face, earlobes and neck.
Sunglasses protect the eyes and surrounding tissues from the damaging effects of UVR. Wearers need to take into account that darker glasses do not necessarily offer greater UV protection to the eyes, as darker glasses may lead to a greater dilatation of the pupils and thus increased exposure to UVR.
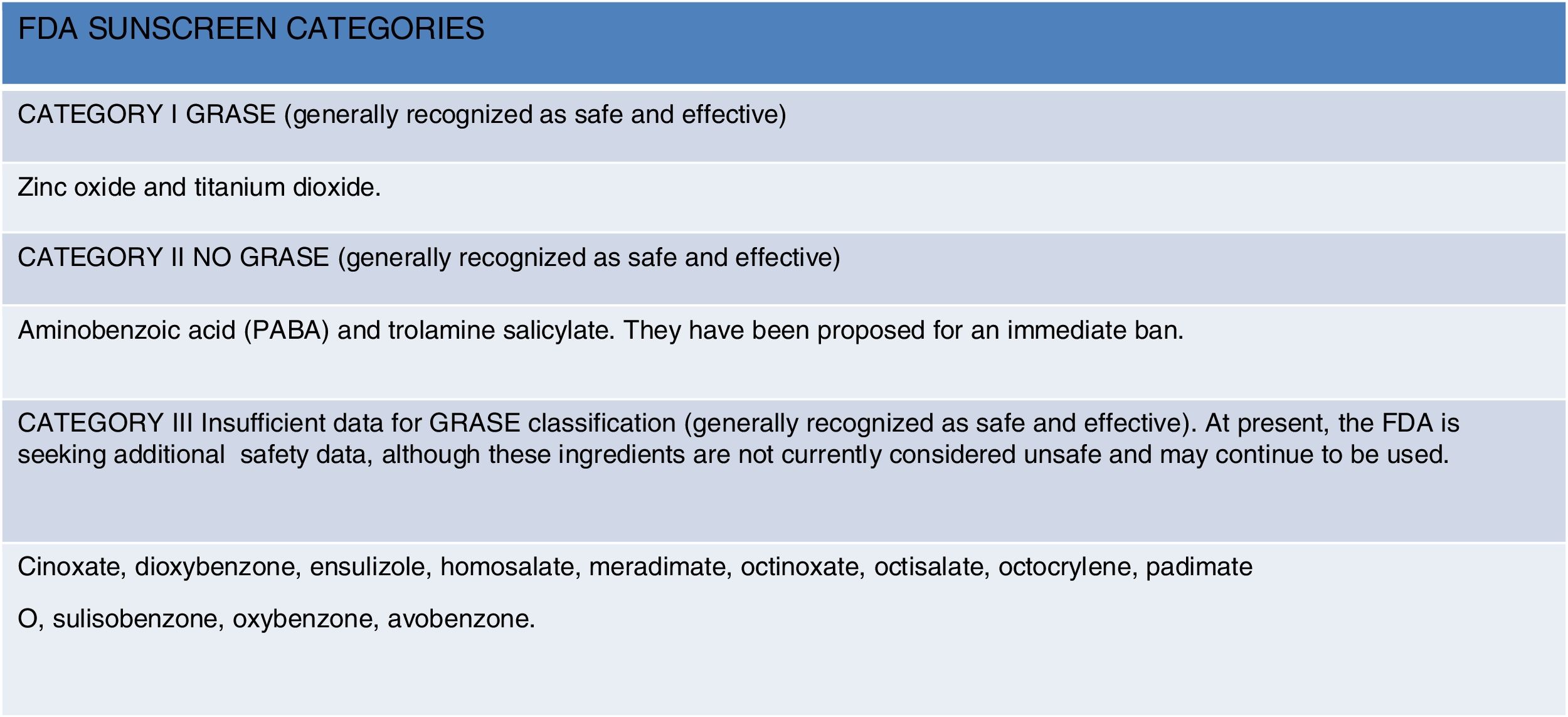
Photoprotective agents (sunscreen)Sunscreen17 works through the presence of an active ingredient that absorbs solar radiation in the 290–400nm range. In most countries, these active ingredients are regulated as cosmetics, but in the United States, Canada and Australia, sunscreens are considered over-the-counter medications. In the United States, the Food and Drug Administration (FDA) regulates the active ingredients found in sunscreens, determines how these products should be tested and establishes labelling requirements. At present, there are 16 sunscreen active ingredients approved in the United States18 (Fig. 2), compared to at least 34 in Australia and 26 in the European Union.
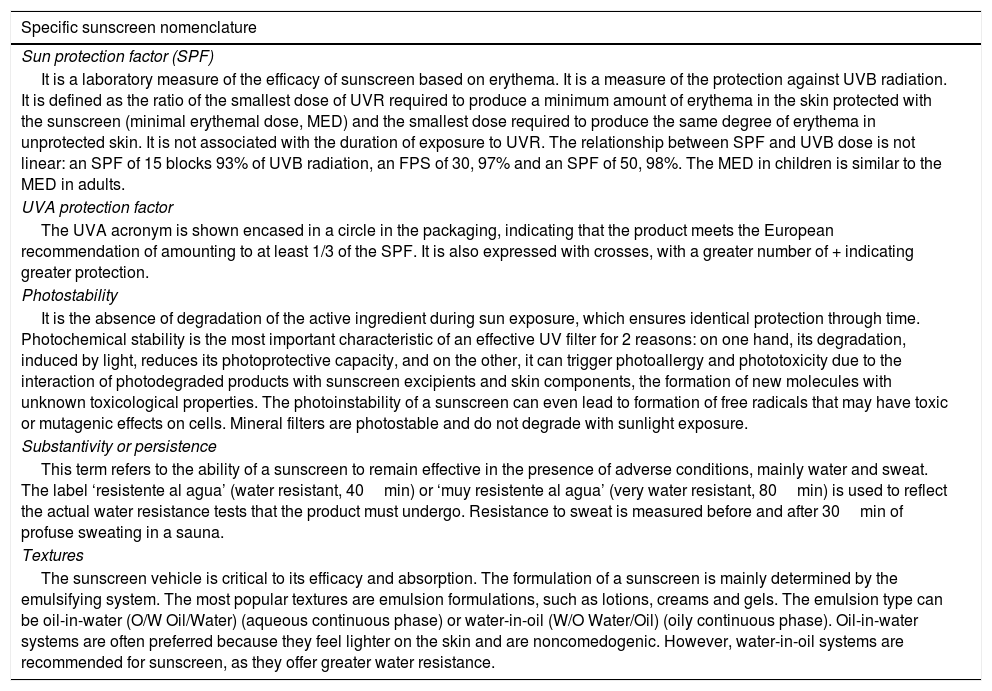
It is important for physicians to correctly interpret sunscreen terminology and provide correct information to their patients to ensure that they obtain the protection they do need (Table 2).
Specific terms summarising the properties and characteristics of sunscreens.
| Specific sunscreen nomenclature |
|---|
| Sun protection factor (SPF) |
| It is a laboratory measure of the efficacy of sunscreen based on erythema. It is a measure of the protection against UVB radiation. It is defined as the ratio of the smallest dose of UVR required to produce a minimum amount of erythema in the skin protected with the sunscreen (minimal erythemal dose, MED) and the smallest dose required to produce the same degree of erythema in unprotected skin. It is not associated with the duration of exposure to UVR. The relationship between SPF and UVB dose is not linear: an SPF of 15 blocks 93% of UVB radiation, an FPS of 30, 97% and an SPF of 50, 98%. The MED in children is similar to the MED in adults. |
| UVA protection factor |
| The UVA acronym is shown encased in a circle in the packaging, indicating that the product meets the European recommendation of amounting to at least 1/3 of the SPF. It is also expressed with crosses, with a greater number of + indicating greater protection. |
| Photostability |
| It is the absence of degradation of the active ingredient during sun exposure, which ensures identical protection through time. Photochemical stability is the most important characteristic of an effective UV filter for 2 reasons: on one hand, its degradation, induced by light, reduces its photoprotective capacity, and on the other, it can trigger photoallergy and phototoxicity due to the interaction of photodegraded products with sunscreen excipients and skin components, the formation of new molecules with unknown toxicological properties. The photoinstability of a sunscreen can even lead to formation of free radicals that may have toxic or mutagenic effects on cells. Mineral filters are photostable and do not degrade with sunlight exposure. |
| Substantivity or persistence |
| This term refers to the ability of a sunscreen to remain effective in the presence of adverse conditions, mainly water and sweat. The label ‘resistente al agua’ (water resistant, 40min) or ‘muy resistente al agua’ (very water resistant, 80min) is used to reflect the actual water resistance tests that the product must undergo. Resistance to sweat is measured before and after 30min of profuse sweating in a sauna. |
| Textures |
| The sunscreen vehicle is critical to its efficacy and absorption. The formulation of a sunscreen is mainly determined by the emulsifying system. The most popular textures are emulsion formulations, such as lotions, creams and gels. The emulsion type can be oil-in-water (O/W Oil/Water) (aqueous continuous phase) or water-in-oil (W/O Water/Oil) (oily continuous phase). Oil-in-water systems are often preferred because they feel lighter on the skin and are noncomedogenic. However, water-in-oil systems are recommended for sunscreen, as they offer greater water resistance. |
Sunscreens are classified as physical or chemical based on their active ingredients.
Physical or mineral sunscreensThe active ingredient is an inorganic compound that provides protection by reflecting or dispersing UVR. The 2 physical active ingredients currently used most frequently are zinc oxide and titanium dioxide,19 which offer broad-spectrum protection against UVA and UVB rays and are less likely to cause irritation, making them more suitable for sensitive skin. The development of novel coating materials, a reduction in particle size to the nanometric range (individual particles with diameters <100nm) and clever formulations that avoid the use of iron oxides have made it possible to produce sunscreens that are easier to spread on the skin, with an appealing appearance and the benefits of mineral protection. Despite their small size, these particles do not penetrate healthy intact skin20 and mostly stay in the stratum corneum. On the other hand, toxicity studies with subcutaneous and intravenous administration of the active ingredient generally found a low toxicity.
Chemical or organic sunscreensThe active ingredient is an organic compound that offers protection by absorbing UVR and dissipating its energy in the form of heat or light. Most of them absorb UVB rays, some absorb UVA2 rays and only 1 organic sunscreen ingredient approved by the FDA, avobenzone, can absorb radiation in the UVA1 range. These are the most common sunscreens in the market. These chemical ingredients include cinoxate, dioxybenzone, ensulizole, homosalate, meradimate, octinoxate, octisalate, octocrylene, padimate O, sulisobenzone, oxybenzone and avobenzone, usually formulated in combinations of two or more active ingredients.
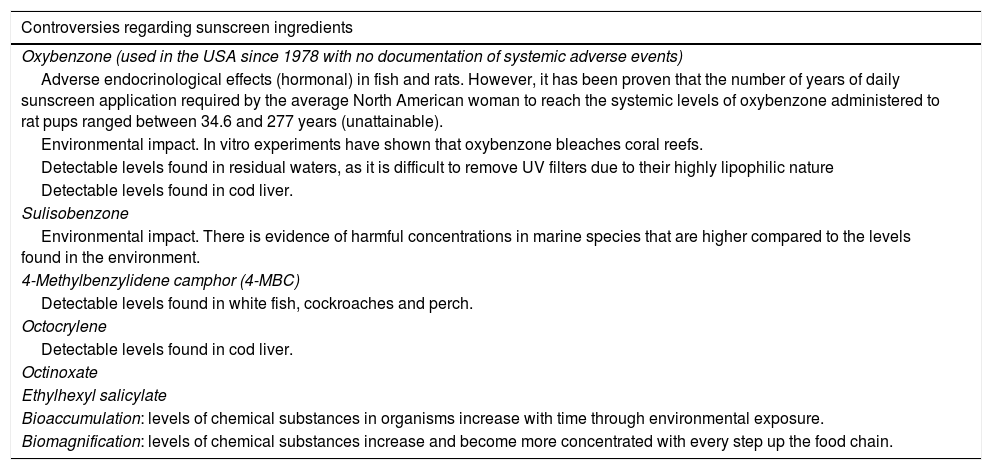
Unfortunately, a growing body of evidence has shown that there are numerous negative effects associated with the use of chemical sunscreens, such as skin hypersensitivity reactions, neurotoxicity and deleterious hormonal effects (Table 3).
Summary of current evidence on the different chemical or organic sunscreen ingredients that have led the FDA to their classification as Category III: skin allergic reactions, hormone disturbances, environmental impact ….
| Controversies regarding sunscreen ingredients |
|---|
| Oxybenzone (used in the USA since 1978 with no documentation of systemic adverse events) |
| Adverse endocrinological effects (hormonal) in fish and rats. However, it has been proven that the number of years of daily sunscreen application required by the average North American woman to reach the systemic levels of oxybenzone administered to rat pups ranged between 34.6 and 277 years (unattainable). |
| Environmental impact. In vitro experiments have shown that oxybenzone bleaches coral reefs. |
| Detectable levels found in residual waters, as it is difficult to remove UV filters due to their highly lipophilic nature |
| Detectable levels found in cod liver. |
| Sulisobenzone |
| Environmental impact. There is evidence of harmful concentrations in marine species that are higher compared to the levels found in the environment. |
| 4-Methylbenzylidene camphor (4-MBC) |
| Detectable levels found in white fish, cockroaches and perch. |
| Octocrylene |
| Detectable levels found in cod liver. |
| Octinoxate |
| Ethylhexyl salicylate |
| Bioaccumulation: levels of chemical substances in organisms increase with time through environmental exposure. |
| Biomagnification: levels of chemical substances increase and become more concentrated with every step up the food chain. |
On the other hand, they may pose a hazard to the environment21,22 (especially to marine life) and even end up in the human food supply chain.
In 2018, the state of Hawaii enacted laws banning 2 of the most popular chemical sunscreens (oxybenzone and octinoxate) due to their harmful impact on coral reefs. Since then, local governments like those of Miami Beach and the Florida Keys have proposed similar legislation.
In 2014, benzophenones were named the “Allergen of the Year” by the American Contact Dermatitis Society.23 Among all UVR filters, they are the most common trigger of photosensitivity and contact allergy reactions (of all patients with allergic reactions to sunscreen, 70.2% had a positive patch test for oxybenzone).
Given the high standards that must be met by sunscreen ingredients, new compounds and combinations have been developed24 with the aim of preventing photodegradation, providing broad-spectrum protection and attain the maximum sun protection factor (SPF) approved for sunscreens by the FDA. One example is the addition of octocrylene to prevent the degradation of avobenzone, a photosensitive compound, or the development in the past decade of ecamsule (Mexoryl SX), a chemical sunscreen appropriate for sensitive skin that is the ideal chemical ingredient for formulations targeted to the paediatric population.
Other topical protective agentsThere is evidence that sunscreens that contain topical antioxidants25 decrease production of reactive oxygen species and cytokines and expression of metalloproteinases after exposure to UVR and visible light, and that the combination of the active ingredient and topical antioxidants performs better compared to sunscreens with the active ingredient alone. There is even evidence that these agents can protect the skin from the effects of environmental pollutants. However, the use of topical antioxidants is limited by their ability to diffuse in the epidermis and their stability. The incorporation of stabilised antioxidants to sunscreens has grown in popularity. Some of the most commonly used antioxidants are vitamin C, quercetin, aloe vera, silymarin, chromane (benzodihydropyran), green tea extract, ginseng extract and Polypodium leucotomos extract, among others.
Photolyases26 are enzymes that repair mutagenic pyrimidine dimers (MPDs). They are naturally occurring enzymes found in bacteria, plants and animals subject to high exposure to UVR, but absent in human and other placental mammals. They repair DNA in the presence of flavonoid compounds, which are UV-active chromophores. Photolyases are packaged in liposomes to improve penetration of the stratum corneum, combined with antioxidants (synergistic effect) and organic UVR filters.
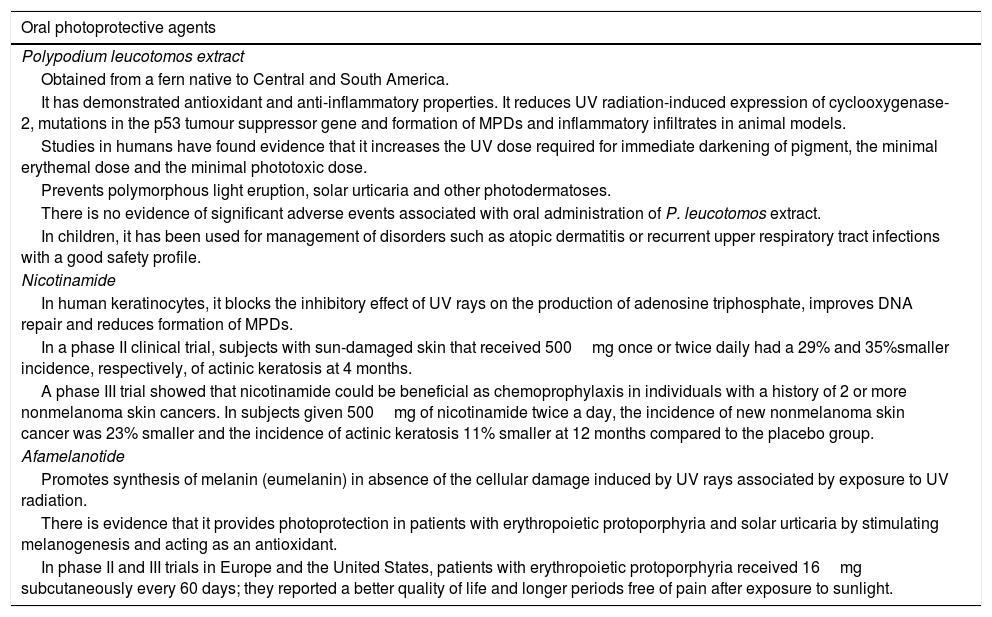
Oral photoprotectionSeveral studies have demonstrated that photoprotective agents administered orally may be useful in reducing photodamage, but studies of larger scope are required to confirm their efficacy (Table 4).27,28 At present, these agents can be used as adjuvants, and not as substitutes, of the photoprotective measures discussed to this point.
Oral photoprotective agents. Characteristics.
| Oral photoprotective agents |
|---|
| Polypodium leucotomos extract |
| Obtained from a fern native to Central and South America. |
| It has demonstrated antioxidant and anti-inflammatory properties. It reduces UV radiation-induced expression of cyclooxygenase-2, mutations in the p53 tumour suppressor gene and formation of MPDs and inflammatory infiltrates in animal models. |
| Studies in humans have found evidence that it increases the UV dose required for immediate darkening of pigment, the minimal erythemal dose and the minimal phototoxic dose. |
| Prevents polymorphous light eruption, solar urticaria and other photodermatoses. |
| There is no evidence of significant adverse events associated with oral administration of P. leucotomos extract. |
| In children, it has been used for management of disorders such as atopic dermatitis or recurrent upper respiratory tract infections with a good safety profile. |
| Nicotinamide |
| In human keratinocytes, it blocks the inhibitory effect of UV rays on the production of adenosine triphosphate, improves DNA repair and reduces formation of MPDs. |
| In a phase II clinical trial, subjects with sun-damaged skin that received 500mg once or twice daily had a 29% and 35%smaller incidence, respectively, of actinic keratosis at 4 months. |
| A phase III trial showed that nicotinamide could be beneficial as chemoprophylaxis in individuals with a history of 2 or more nonmelanoma skin cancers. In subjects given 500mg of nicotinamide twice a day, the incidence of new nonmelanoma skin cancer was 23% smaller and the incidence of actinic keratosis 11% smaller at 12 months compared to the placebo group. |
| Afamelanotide |
| Promotes synthesis of melanin (eumelanin) in absence of the cellular damage induced by UV rays associated by exposure to UV radiation. |
| There is evidence that it provides photoprotection in patients with erythropoietic protoporphyria and solar urticaria by stimulating melanogenesis and acting as an antioxidant. |
| In phase II and III trials in Europe and the United States, patients with erythropoietic protoporphyria received 16mg subcutaneously every 60 days; they reported a better quality of life and longer periods free of pain after exposure to sunlight. |
Countless campaigns have been devoted to improving knowledge in this area and promoting adherence with healthy sunlight exposure habits, but awareness does not necessarily lead to the establishment of healthy habits.29
One of the largest studies30 conducted in students (887 schoolchildren in Switzerland) found that knowledge about photoprotection and the risks of sunlight exposure was adequate, yet there was no adherence to photoprotective habits. Most participants attributed this to forgetfulness, not to mention the widespread positive attitude towards tanning.31
Studies to date conclude that in general, adolescents, as occurs with alcohol and drug use, are aware of the risks, yet many continue to not limit their sunlight exposure.
Exposure of infants and younger children rather depends on the attitudes and beliefs of their parents.32 The use of sunscreen by parents predicts the use of sunscreen in their children, and a positive attitude towards tanning is inversely associated to the photoprotective measures used in children. Yet even when sunscreen is used, its administration is inadequate, with a mean application thickness of 0.48mg/cm2, less than ¼ of the amount used in clinical trials of sunscreens (2mg/cm2), meaning that the SPF of the amount used is less than ¼ of the SPF specified in the product label.33
Photoprotection campaigns and development of specific denominationsSchool-based programmes are key to improve behaviours related to sunlight exposure. Educational programmes such as SunSmart School34 in Australia, SunWise in the United States or SolSano35 in Spain have succeeded in improving awareness, attitudes and especially photoprotective practices in schoolchildren, and to reduce the incidence of sunburn in the target population. They have also proven to be the most cost-effective type of intervention.
The World Health Organisation has encouraged governments to develop photoprotection policies (concerning educational curricula, shade management, timing of outdoor activities, school uniforms, use of caps, sunglasses and sunscreen) applicable to outdoor activities when the UVI is 3 or greater. It also recommends the development of evaluation systems leading to official recognition of centres that implement adequate measures to motivate schools to promote photoprotection. The accreditation/certification of photoprotection in schools has been put into practice in countries like Australia, New Zealand, the United States and Germany, with good reception by the public and excellent results. The Soludable denomination is the first distinction awarded in recognition of school-based photoprotection implemented in Spain. It is a certification that identifies schools that actively promote photoprotection policies and practices and involve the entire school community.
Vitamin D and photoprotectionThere has been constant concern that the use of sunscreen may lead to vitamin D (VD) deficiency. However, it has been proven that regular suberythemal sunlight exposure with application of SPF 30 sunscreen can achieve serum VD levels comparable to those achieved by exposure without photoprotection in healthy adults. The required dose of sunlight required to synthesise adequate amounts of VD depends on the type of skin (phototype), the time of day, the month of the year and the latitude. The duration of exposure required by an individual with dark skin is approximately 10 times greater compared to a light-skinned individual. Different studies36,37 suggest that exposure to sunlight for 5min to 5h a day (depending on the aforementioned factors) could suffice to synthesise daily VD requirements.
On the other hand, one pilot study38 demonstrated that high doses of oral vitamin D3 (200,000UI cholecalciferol) are beneficial in attenuating the effects of sunburn, probably by upregulating expression of the anti-inflammatory mediator arginase-1 in the skin.
Blue light, or high-energy visible lightLight is composed of electromagnetic particles that travel in waves of variable length and frequency. The human eye is only sensitive to a limited part of the light spectrum, which we refer to as visible light and perceive as colour. Colours corresponding to shorter wavelengths, such as blue, carry more energy.
The use of electronic devices is increasing in children of all ages, from the youngest toddlers to adolescents. Computers, tablets and mobile phones have entered their daily lives for both educational and entertainment purposes.
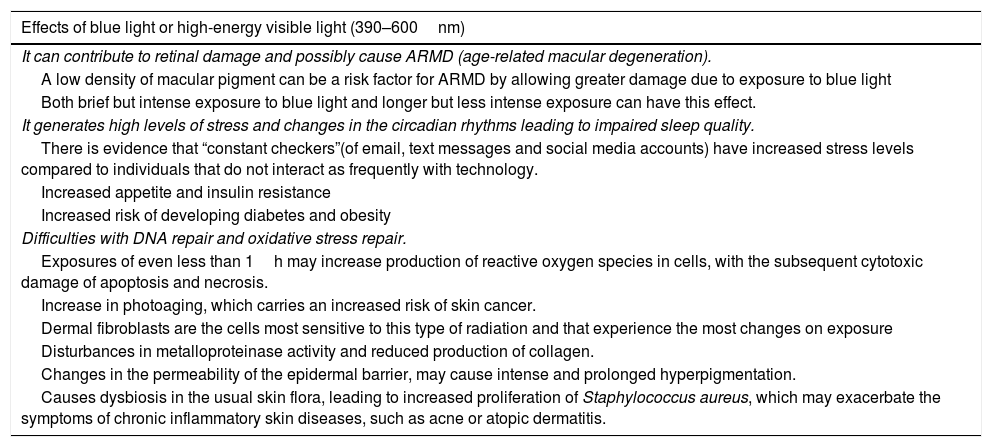
The fact that blue light may affect our health is supported by more than anecdotal evidence in the scientific literature (Table 5),39,40 and we need to use specific photoprotection for it.
Effects of blue light or high-energy visible light.
| Effects of blue light or high-energy visible light (390–600nm) |
|---|
| It can contribute to retinal damage and possibly cause ARMD (age-related macular degeneration). |
| A low density of macular pigment can be a risk factor for ARMD by allowing greater damage due to exposure to blue light |
| Both brief but intense exposure to blue light and longer but less intense exposure can have this effect. |
| It generates high levels of stress and changes in the circadian rhythms leading to impaired sleep quality. |
| There is evidence that “constant checkers”(of email, text messages and social media accounts) have increased stress levels compared to individuals that do not interact as frequently with technology. |
| Increased appetite and insulin resistance |
| Increased risk of developing diabetes and obesity |
| Difficulties with DNA repair and oxidative stress repair. |
| Exposures of even less than 1h may increase production of reactive oxygen species in cells, with the subsequent cytotoxic damage of apoptosis and necrosis. |
| Increase in photoaging, which carries an increased risk of skin cancer. |
| Dermal fibroblasts are the cells most sensitive to this type of radiation and that experience the most changes on exposure |
| Disturbances in metalloproteinase activity and reduced production of collagen. |
| Changes in the permeability of the epidermal barrier, may cause intense and prolonged hyperpigmentation. |
| Causes dysbiosis in the usual skin flora, leading to increased proliferation of Staphylococcus aureus, which may exacerbate the symptoms of chronic inflammatory skin diseases, such as acne or atopic dermatitis. |
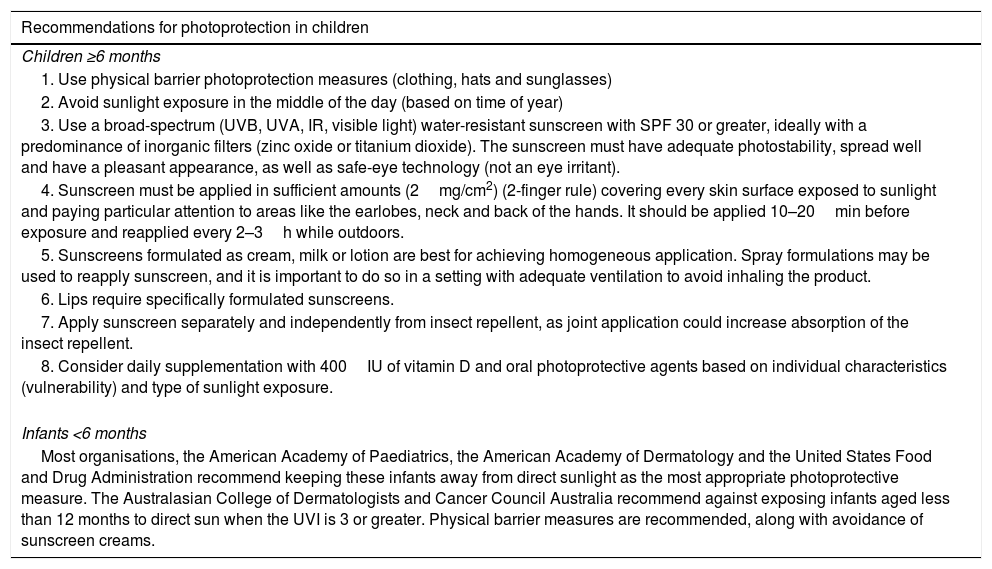
As is the case of other healthy lifestyle habits (diet, physical activity, hygiene, …), good photoprotection habits (Table 6) are invaluable, and instilling them in our children should be made a priority. Our society, with its increasing knowledge, expectations and environmental awareness has developed excellent photoprotective products that are being reformulated on a daily basis with the aim of improving quality.
Summary of recommendations for photoprotection in children by age group.
| Recommendations for photoprotection in children |
|---|
| Children ≥6 months |
| 1. Use physical barrier photoprotection measures (clothing, hats and sunglasses) |
| 2. Avoid sunlight exposure in the middle of the day (based on time of year) |
| 3. Use a broad-spectrum (UVB, UVA, IR, visible light) water-resistant sunscreen with SPF 30 or greater, ideally with a predominance of inorganic filters (zinc oxide or titanium dioxide). The sunscreen must have adequate photostability, spread well and have a pleasant appearance, as well as safe-eye technology (not an eye irritant). |
| 4. Sunscreen must be applied in sufficient amounts (2mg/cm2) (2-finger rule) covering every skin surface exposed to sunlight and paying particular attention to areas like the earlobes, neck and back of the hands. It should be applied 10–20min before exposure and reapplied every 2–3h while outdoors. |
| 5. Sunscreens formulated as cream, milk or lotion are best for achieving homogeneous application. Spray formulations may be used to reapply sunscreen, and it is important to do so in a setting with adequate ventilation to avoid inhaling the product. |
| 6. Lips require specifically formulated sunscreens. |
| 7. Apply sunscreen separately and independently from insect repellent, as joint application could increase absorption of the insect repellent. |
| 8. Consider daily supplementation with 400IU of vitamin D and oral photoprotective agents based on individual characteristics (vulnerability) and type of sunlight exposure. |
| Infants <6 months |
| Most organisations, the American Academy of Paediatrics, the American Academy of Dermatology and the United States Food and Drug Administration recommend keeping these infants away from direct sunlight as the most appropriate photoprotective measure. The Australasian College of Dermatologists and Cancer Council Australia recommend against exposing infants aged less than 12 months to direct sun when the UVI is 3 or greater. Physical barrier measures are recommended, along with avoidance of sunscreen creams. |
Please cite this article as: Garnacho Saucedo GM, Salido Vallejo R, Moreno Giménez JC. Efectos de la radiación solar y actualización en fotoprotección. An Pediatr (Barc). 2020;92:380.