Eating disorders are severe mental health disorders characterized by changes in eating-related behavior, thoughts and emotions. They typically manifest at young ages, chiefly in adolescence or preadolescence. Due to their complexity, the management of eating disorders requires a multidisciplinary approach led by mental health professionals. However, the high demand for services may delay access to specialized care, which makes it necessary for pediatricians to adopt a proactive role.
Pediatricians play a key role in the prevention of eating disorders by promoting a healthy relationship with food and body image as well as in their detection and initial management, enabling the implementation of early interventions to stabilize the patient while coordinating specialized care. The pediatrician is also a key figure throughout the followup in monitoring the physical and mental health of affected patients, guaranteeing the delivery of comprehensive care in collaboration with the multidisciplinary team.
Los Trastornos de la Conducta Alimentaria (TCA) son enfermedades mentales graves caracterizadas por alteraciones en el comportamiento, los pensamientos y las emociones relacionadas con la ingesta de alimentos. Suelen manifestarse a edades tempranas, principalmente en la adolescencia o preadolescencia. Su complejidad requiere un abordaje interdisciplinar, liderado por profesionales de la salud mental. No obstante, la alta demanda asistencial puede retrasar el acceso a la atención especializada, lo que hace imprescindible que el pediatra asuma un rol proactivo.
Su papel es clave en la prevención, promoviendo una relación saludable con la alimentación y la imagen corporal, así como en la detección y manejo inicial, asegurando intervenciones tempranas que estabilicen al paciente mientras se coordina la atención especializada. Además, a lo largo de toda la evolución de la enfermedad, el pediatra desempeña una función fundamental en el seguimiento del estado de salud física y mental, garantizando una atención integral en colaboración con el equipo interdisciplinar.
Eating disorders (EDs) are complex and serious mental health disorders that manifest with persistent disturbances in eating-related behavior, thoughts and emotions. These disturbances have a substantial impact on dietary intake, significantly impairing physical health and psychosocial functioning.1
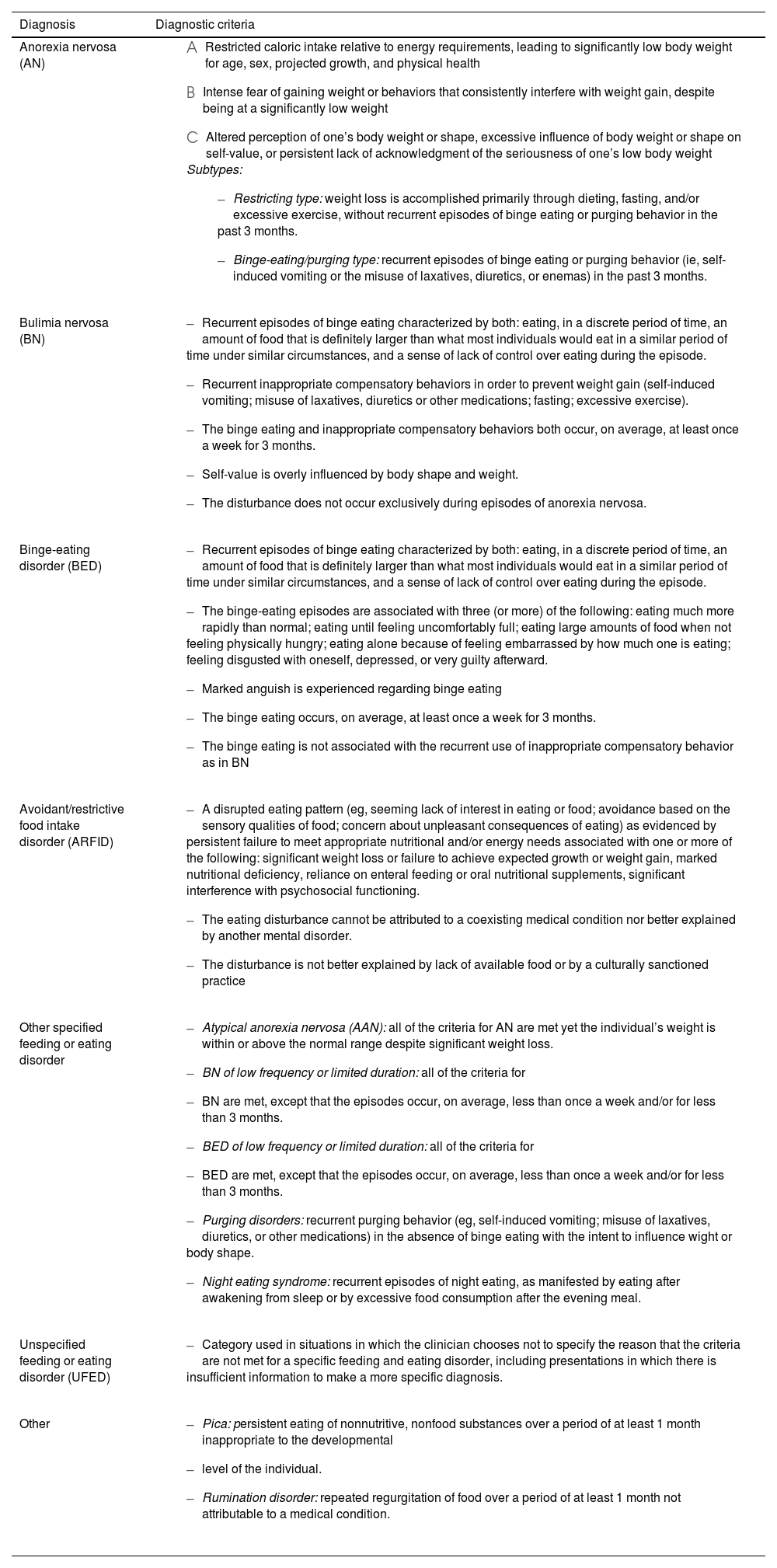
They include, among others, anorexia nervosa (AN), bulimia nervosa (BN), binge-eating disorder (BED), atypical anorexia nervosa (AAN) and avoidant/restrictive food intake disorder (ARFID) (Table 1).1 Due to the particular manifestations and specific approach to the management of ARFID, which differ from those of other EDs, we will not address it in this article.
Diagnostic criteria for eating disorders defined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) of the American Psychiatric Association.
| Diagnosis | Diagnostic criteria |
|---|---|
| Anorexia nervosa (AN) |
|
| Bulimia nervosa (BN) |
|
| Binge-eating disorder (BED) |
|
| Avoidant/restrictive food intake disorder (ARFID) |
|
| Other specified feeding or eating disorder |
|
| Unspecified feeding or eating disorder (UFED) |
|
| Other |
|
The prevalence of EDs varies considerably depending on the country and the methodology used in epidemiological studies, resulting in heterogeneous estimates. At the global level, it is estimated that 5.5% to 17.9% of women and 0.6% to 2.4% of men will have an ED during their lifetime. In Europe, the estimated prevalence in women is 1% to 4% for AN, 1% to 2% for BN and 1% to 4% for BED. In men, the prevalence of EDs is estimated at 0.3 to 0.7%.2 Data from various European countries have evinced an alarming increase in the incidence of EDs in the population aged 6 to 18 years since the beginning of the coronavirus disease 2019 (COVID-19) pandemic, in addition to an increase in severity and earlier onset of these disorders.3–5
Although they are most common in female adolescents, they can affect people of any age, sex, race, socioeconomic status, body build or weight. The average age of onset is 12.5 years. Adolescents who participate in sports that emphasize thinness or impose weight requirements (eg, gymnastics, horseback riding, dance, athletics or boxing) are at increased risk of developing an ED.6–8
Patients with early onset of EDs (before adolescence) are more likely to have a previous history of psychiatric disorders, such as depression, obsessive-compulsive disorder or anxiety. In this subset of patients, binge-eating episodes and purging behaviors are less frequent. In addition, there is a more uniform sex distribution and weight loss tends to be quicker, which could facilitate earlier detection in many cases.6
The high prevalence and early onset of EDs highlight the importance of the role played by pediatricians in their prevention, detection and early diagnosis. Given their complexity, these disorders require multidisciplinary management led by mental health professionals. However, the high demand for care usually delays access to specialized treatment. In this context, it is important for pediatricians to be proactive, implementing early interventions to stabilize patients, making sure that they are not left unattended during this critical period and coordinating multidisciplinary care.
PreventionThe development of EDs involves a complex interaction of biological, genetic, psychological and social factors. Some of the most relevant modifiable risk factors are the energy intake deficit associated with the pursuit of restrictive diets and the low self-esteem associated with body dissatisfaction. In this regard, pediatricians play a key role in implementing strategies aimed at promoting a healthy relationship with food and the body, thus contributing to primary prevention. These strategies include9–12:
- 1
Discouraging restrictive diets, meal skipping or prolonged fasting. Extreme calorie restriction is the main risk factor for the development of EDs. In adolescents, following a very strict diet is associated with an 18-fold increase in the risk of developing an ED, while following a moderate diet is associated with a five-fold increase. Therefore, it is essential to promote balanced and sustainable dietary habits instead of to focusing on weight loss, with a family-centered approach to intervention.
- 2
Promoting family meals. A higher frequency of family meals is associated with improved diet quality and has a protective effect against the development of unhealthy eating behaviors in adolescents. It also facilitates early detection of changes in dietary habits.
- 3
Advising families to refrain from talking about weight or body image at home. The focus should be on promoting balanced nutrition and physical activity habits rather than on physical appearance.
- 4
Discouraging any form of teasing or negative comments about weight. Criticism or jokes related to body weight, especially within the family, are associated with an increased risk of excess weight, binge-eating and unhealthy weight-control behaviors in girls as well as excess weight in boys.
- 5
Promoting a positive body image. Fostering the acceptance of body diversity and self-care is important. Efforts should be made to avoid reinforcing body dissatisfaction as a motivation for changing dietary habits or body weight.
- 6
Inquiring about any past history of mistreatment or bullying. In adolescents with overweight or obesity, it is essential to assess for potential experiences of victimization, and these issues should be addressed with the patient and the family.
- 7
Carefully monitoring weight loss in adolescents who need to lose weight, prioritizing the establishment of a varied and flexible diet rather than focusing on weight changes. The weight loss process should always be closely monitored by a medical provider.
In conclusion, by promoting an environment that fosters healthy habits, a positive body image and emotional support in the home, pediatricians can contribute significantly to reducing the risk of EDs.
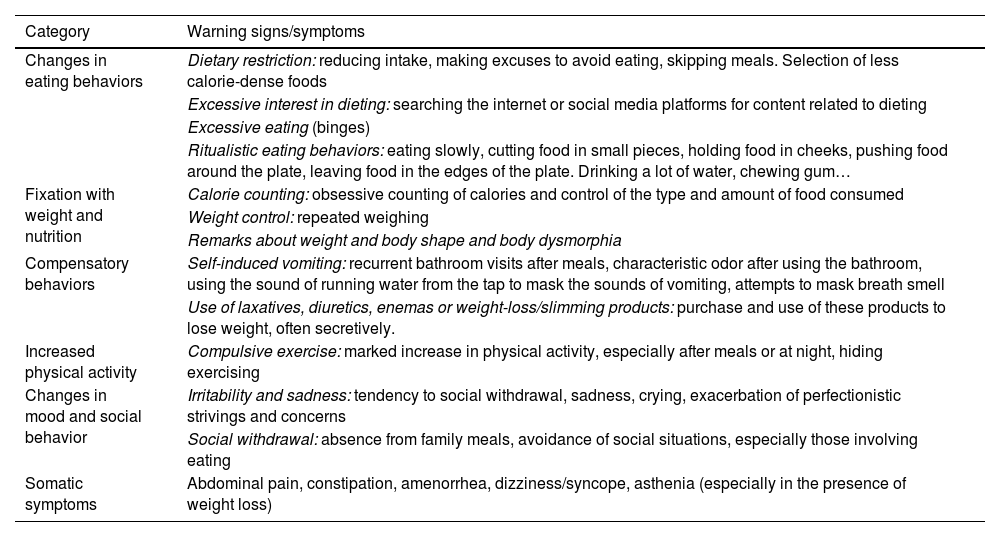
Early detection and assessmentThe best strategy for the early detection and diagnosis of an ED is for the pediatrician to maintain a high index of suspicion, being particularly watchful for the signs and symptoms that may indicate its presence (Tables 1 and 2).13,14 The presenting complaint is frequently a somatic symptom, such as abdominal pain (which is presented as the reason for the low intake), constipation, dizziness, amenorrhea or a “food intolerance” typically involving calorie-dense foods. Any of these, especially if associated with weight loss, should prompt the pediatrician to explore the possibility of an ED.
Warning signs/symptoms of an eating disorder.
| Category | Warning signs/symptoms |
|---|---|
| Changes in eating behaviors | Dietary restriction: reducing intake, making excuses to avoid eating, skipping meals. Selection of less calorie-dense foods |
| Excessive interest in dieting: searching the internet or social media platforms for content related to dieting | |
| Excessive eating (binges) | |
| Ritualistic eating behaviors: eating slowly, cutting food in small pieces, holding food in cheeks, pushing food around the plate, leaving food in the edges of the plate. Drinking a lot of water, chewing gum… | |
| Fixation with weight and nutrition | Calorie counting: obsessive counting of calories and control of the type and amount of food consumed |
| Weight control: repeated weighing | |
| Remarks about weight and body shape and body dysmorphia | |
| Compensatory behaviors | Self-induced vomiting: recurrent bathroom visits after meals, characteristic odor after using the bathroom, using the sound of running water from the tap to mask the sounds of vomiting, attempts to mask breath smell |
| Use of laxatives, diuretics, enemas or weight-loss/slimming products: purchase and use of these products to lose weight, often secretively. | |
| Increased physical activity | Compulsive exercise: marked increase in physical activity, especially after meals or at night, hiding exercising |
| Changes in mood and social behavior | Irritability and sadness: tendency to social withdrawal, sadness, crying, exacerbation of perfectionistic strivings and concerns |
| Social withdrawal: absence from family meals, avoidance of social situations, especially those involving eating | |
| Somatic symptoms | Abdominal pain, constipation, amenorrhea, dizziness/syncope, asthenia (especially in the presence of weight loss) |
It is also essential to consider the possibility of atypical presentations. Some patients, especially the youngest, may not explicitly express a desire to lose weight, a fear of gaining weight or a distorted body image. In the case of prepubertal patients, the weight loss may not be apparent, but there may be other noticeable manifestations, such as failure to reach the expected weight or deceleration of linear growth. In boys, the symptoms may be less evident and present under the guise of wanting to “be healthy” or “improve athletic performance”, with an emphasis on increasing muscle mass and excessive exercise.
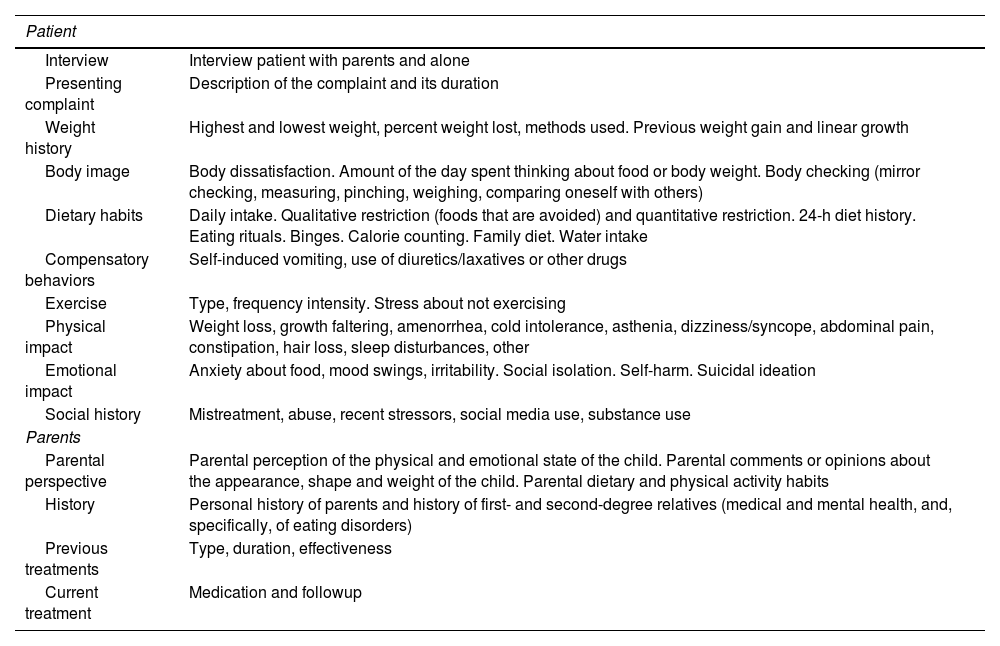
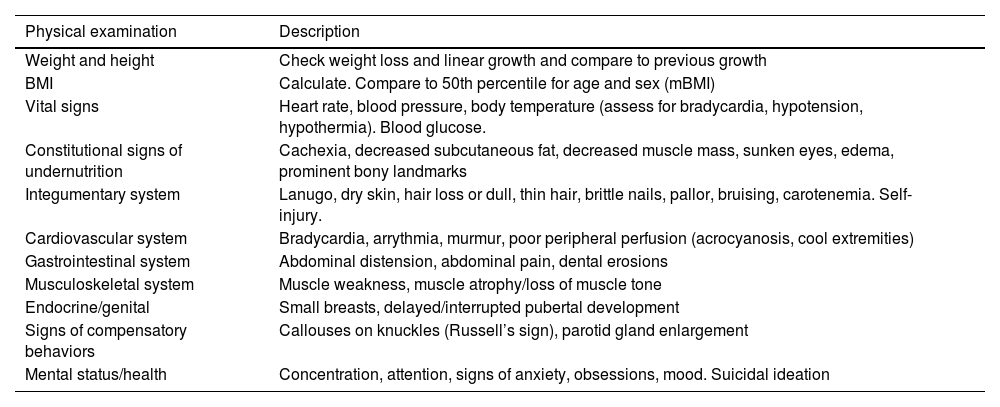
Any red flag should prompt a focused history taking (Table 3) in addition to an exhaustive physical examination (Table 4) and measurement of vital signs (standing and supine blood pressure, heart rate), weight, height and body mass index (BMI).6 It is important to compare current and premorbid anthropometric measurements, recording them in the growth chart, and monitoring weight loss and the pace at which it occurs.
Focused complaint-directed history for a suspected eating disorder.
| Patient | |
|---|---|
| Interview | Interview patient with parents and alone |
| Presenting complaint | Description of the complaint and its duration |
| Weight history | Highest and lowest weight, percent weight lost, methods used. Previous weight gain and linear growth |
| Body image | Body dissatisfaction. Amount of the day spent thinking about food or body weight. Body checking (mirror checking, measuring, pinching, weighing, comparing oneself with others) |
| Dietary habits | Daily intake. Qualitative restriction (foods that are avoided) and quantitative restriction. 24-h diet history. Eating rituals. Binges. Calorie counting. Family diet. Water intake |
| Compensatory behaviors | Self-induced vomiting, use of diuretics/laxatives or other drugs |
| Exercise | Type, frequency intensity. Stress about not exercising |
| Physical impact | Weight loss, growth faltering, amenorrhea, cold intolerance, asthenia, dizziness/syncope, abdominal pain, constipation, hair loss, sleep disturbances, other |
| Emotional impact | Anxiety about food, mood swings, irritability. Social isolation. Self-harm. Suicidal ideation |
| Social history | Mistreatment, abuse, recent stressors, social media use, substance use |
| Parents | |
| Parental perspective | Parental perception of the physical and emotional state of the child. Parental comments or opinions about the appearance, shape and weight of the child. Parental dietary and physical activity habits |
| History | Personal history of parents and history of first- and second-degree relatives (medical and mental health, and, specifically, of eating disorders) |
| Previous treatments | Type, duration, effectiveness |
| Current treatment | Medication and followup |
Physical examination. Key aspects in patients with eating disorders.
| Physical examination | Description |
|---|---|
| Weight and height | Check weight loss and linear growth and compare to previous growth |
| BMI | Calculate. Compare to 50th percentile for age and sex (mBMI) |
| Vital signs | Heart rate, blood pressure, body temperature (assess for bradycardia, hypotension, hypothermia). Blood glucose. |
| Constitutional signs of undernutrition | Cachexia, decreased subcutaneous fat, decreased muscle mass, sunken eyes, edema, prominent bony landmarks |
| Integumentary system | Lanugo, dry skin, hair loss or dull, thin hair, brittle nails, pallor, bruising, carotenemia. Self-injury. |
| Cardiovascular system | Bradycardia, arrythmia, murmur, poor peripheral perfusion (acrocyanosis, cool extremities) |
| Gastrointestinal system | Abdominal distension, abdominal pain, dental erosions |
| Musculoskeletal system | Muscle weakness, muscle atrophy/loss of muscle tone |
| Endocrine/genital | Small breasts, delayed/interrupted pubertal development |
| Signs of compensatory behaviors | Callouses on knuckles (Russell’s sign), parotid gland enlargement |
| Mental status/health | Concentration, attention, signs of anxiety, obsessions, mood. Suicidal ideation |
Abbreviation: mBMI, median BMI (50th percentile) for age and sex.
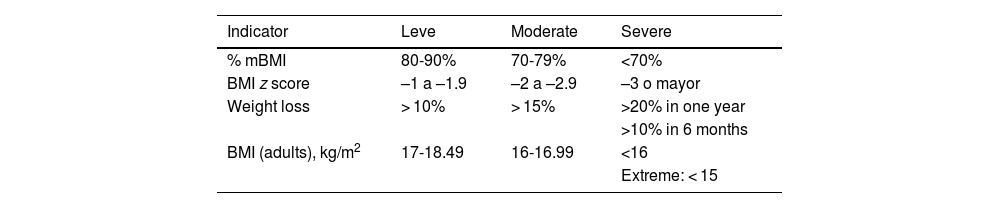
The degree of malnutrition must be assessed (Table 5),15 always remembering that a BMI in the normal range does not rule out EDs or the possibility of serious complications. Patients may maintain a normal weight or even be overweight, yet exhibit behaviors typical of EDs, such as binge eating or vomiting. In particular, patients who are overweight at the outset may experience severe malnutrition despite maintaining a normal BMI, which underscores the importance of a comprehensive assessment beyond the BMI.
Assessment of the degree of undernutrition.
| Indicator | Leve | Moderate | Severe |
|---|---|---|---|
| % mBMI | 80-90% | 70-79% | <70% |
| BMI z score | –1 a –1.9 | –2 a –2.9 | –3 o mayor |
| Weight loss | > 10% | > 15% | >20% in one year |
| >10% in 6 months | |||
| BMI (adults), kg/m2 | 17-18.49 | 16-16.99 | <16 |
| Extreme: < 15 |
%mBMI: BMI as percentage of the median for age and sex = current BMI/median BMI for age and sex × 100.
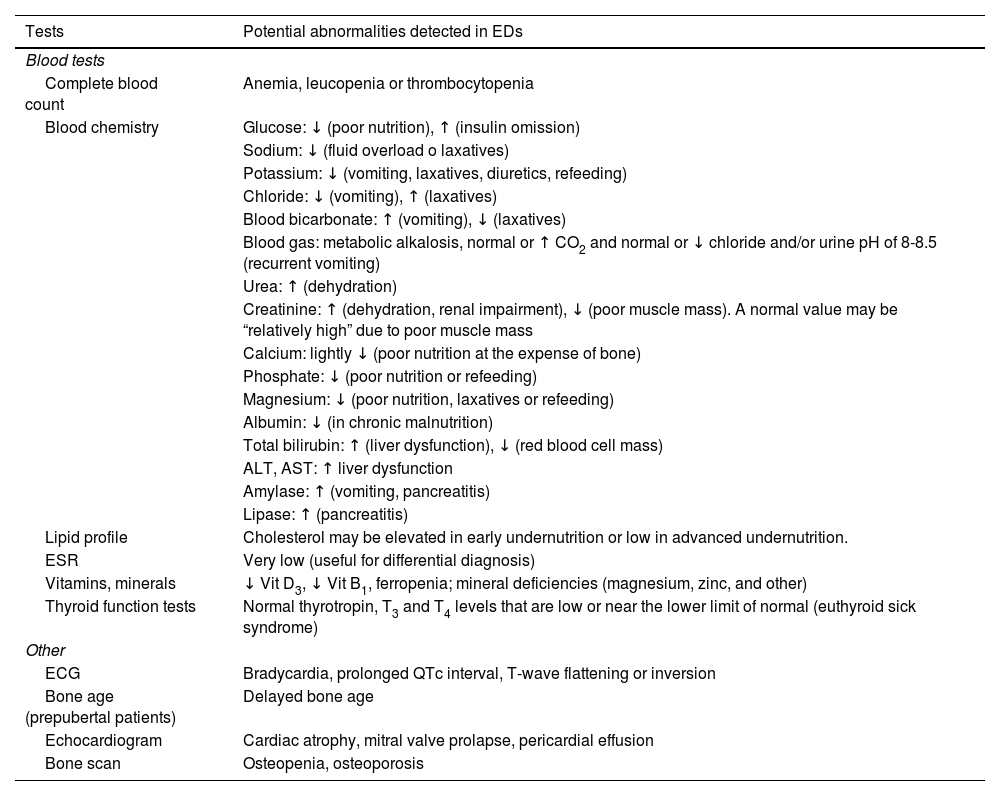
Laboratory tests can be useful for identification of certain complications associated with EDs (Table 6). However, it is important to keep in mind that results within the normal range do not exclude the presence of an ED.
Abnormalities detected in the diagnostic tests used most commonly in patients with eating disorders.
| Tests | Potential abnormalities detected in EDs |
|---|---|
| Blood tests | |
| Complete blood count | Anemia, leucopenia or thrombocytopenia |
| Blood chemistry | Glucose: ↓ (poor nutrition), ↑ (insulin omission) |
| Sodium: ↓ (fluid overload o laxatives) | |
| Potassium: ↓ (vomiting, laxatives, diuretics, refeeding) | |
| Chloride: ↓ (vomiting), ↑ (laxatives) | |
| Blood bicarbonate: ↑ (vomiting), ↓ (laxatives) | |
| Blood gas: metabolic alkalosis, normal or ↑ CO2 and normal or ↓ chloride and/or urine pH of 8-8.5 (recurrent vomiting) | |
| Urea: ↑ (dehydration) | |
| Creatinine: ↑ (dehydration, renal impairment), ↓ (poor muscle mass). A normal value may be “relatively high” due to poor muscle mass | |
| Calcium: lightly ↓ (poor nutrition at the expense of bone) | |
| Phosphate: ↓ (poor nutrition or refeeding) | |
| Magnesium: ↓ (poor nutrition, laxatives or refeeding) | |
| Albumin: ↓ (in chronic malnutrition) | |
| Total bilirubin: ↑ (liver dysfunction), ↓ (red blood cell mass) | |
| ALT, AST: ↑ liver dysfunction | |
| Amylase: ↑ (vomiting, pancreatitis) | |
| Lipase: ↑ (pancreatitis) | |
| Lipid profile | Cholesterol may be elevated in early undernutrition or low in advanced undernutrition. |
| ESR | Very low (useful for differential diagnosis) |
| Vitamins, minerals | ↓ Vit D3, ↓ Vit B1, ferropenia; mineral deficiencies (magnesium, zinc, and other) |
| Thyroid function tests | Normal thyrotropin, T3 and T4 levels that are low or near the lower limit of normal (euthyroid sick syndrome) |
| Other | |
| ECG | Bradycardia, prolonged QTc interval, T-wave flattening or inversion |
| Bone age (prepubertal patients) | Delayed bone age |
| Echocardiogram | Cardiac atrophy, mitral valve prolapse, pericardial effusion |
| Bone scan | Osteopenia, osteoporosis |
Abbreviations: ALT, alanine aminotransferase; AST, aspartate aminotransferase; CO2, carbon dioxide; ECG, electrocardiogram; ED, eating disorder; ESR, erythrocyte sedimentation rate; QTc, corrected QT interval.
An electrocardiogram (ECG) is indicated in patients with clinically significant abnormalities (bradycardia with heart rate < 50 bpm, tachycardia, hypotension, syncope, dizziness, palpitations or chest pain), electrolyte disturbances, severe undernutrition and/or use of diuretics, laxatives or medication that prolongs the QT interval.16
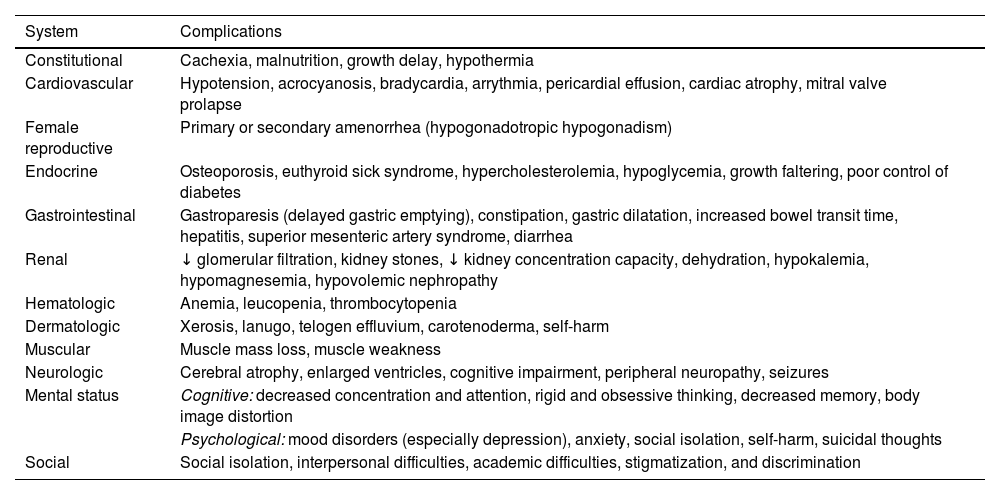
It is important to consider and rule out other causes of weight loss or vomiting, although this should not result in delaying intervention. Once the diagnosis is confirmed, patients should be followed up with assessments at regular intervals to detect medical complications. These can be severe, may involve any organ or system, and usually result from weight loss, malnutrition and/or recurrent purging behaviors (Table 7).16–18
Complications of eating disorders.
| System | Complications |
|---|---|
| Constitutional | Cachexia, malnutrition, growth delay, hypothermia |
| Cardiovascular | Hypotension, acrocyanosis, bradycardia, arrythmia, pericardial effusion, cardiac atrophy, mitral valve prolapse |
| Female reproductive | Primary or secondary amenorrhea (hypogonadotropic hypogonadism) |
| Endocrine | Osteoporosis, euthyroid sick syndrome, hypercholesterolemia, hypoglycemia, growth faltering, poor control of diabetes |
| Gastrointestinal | Gastroparesis (delayed gastric emptying), constipation, gastric dilatation, increased bowel transit time, hepatitis, superior mesenteric artery syndrome, diarrhea |
| Renal | ↓ glomerular filtration, kidney stones, ↓ kidney concentration capacity, dehydration, hypokalemia, hypomagnesemia, hypovolemic nephropathy |
| Hematologic | Anemia, leucopenia, thrombocytopenia |
| Dermatologic | Xerosis, lanugo, telogen effluvium, carotenoderma, self-harm |
| Muscular | Muscle mass loss, muscle weakness |
| Neurologic | Cerebral atrophy, enlarged ventricles, cognitive impairment, peripheral neuropathy, seizures |
| Mental status | Cognitive: decreased concentration and attention, rigid and obsessive thinking, decreased memory, body image distortion |
| Psychological: mood disorders (especially depression), anxiety, social isolation, self-harm, suicidal thoughts | |
| Social | Social isolation, interpersonal difficulties, academic difficulties, stigmatization, and discrimination |
Early and appropriate treatment of EDs is crucial to modify the course of disease and improve patient outcomes. A multidisciplinary approach, led by mental health specialists and with participation of pediatricians or other health care professionals (family physicians, endocrinologists, nutritionists…) enables the effective management of both the physical and psychological aspects of the disease. Referral to mental health specialists, including psychiatrists and psychologists, cannot be delayed. Within the care team, the pediatrician plays a key role as coordinator, facilitating the interactions between patients, families and the care team, and helping destigmatize mental health disorders. The pediatrician also has the responsibility of monitoring the patient throughout the followup.
Nutritional support and psychotherapy are the cornerstones of treatment. In patients with undernutrition, weight restoration is the primary goal, as it is considered an absolutely necessary to promote changes in cognition, emotion and behavior. Weight goals in the nutritional rehabilitation process must be individualized, taking into account premorbid growth trajectories (weight, height and BMI), the age at pubertal onset and the current pubertal stage.19,20 In female patients, the spontaneous resumption of menses is a key indicator of physical and nutritional recovery.
In children and adolescents with AN or BN, interventions at the family level, including family-based therapy (FBT), have proven most effective. The FBT approach emphasizes active parental involvement as a key element for the success of treatment and focuses on eliminating the factors that perpetuate the disorder. Its goals are to increase knowledge and competence in parents and caregivers and to offer them support, as they are considered the most important resource in the nutritional rehabilitation and recovery process.21–23 In addition, while the data on the subject are still scarce, there is evidence suggesting that FBT can be modified for management of children with ARFID and adolescents with AAN, expanding its utility to different disordered eating patterns.14,15
In children and adolescents, pharmacotherapy is generally not used as first-line treatment, but it may be useful in patients with significant psychiatric comorbidities, chiefly depression or anxiety, or in whom nutritional and psychological interventions prove insufficient.24,25
Pediatricians can play an active role, both in the initial stages (while the patient awaits access to specialized treatment) and throughout the therapeutic process. The following are the interventions that pediatricians can implement in coordination with the rest of the care team6,12–15:
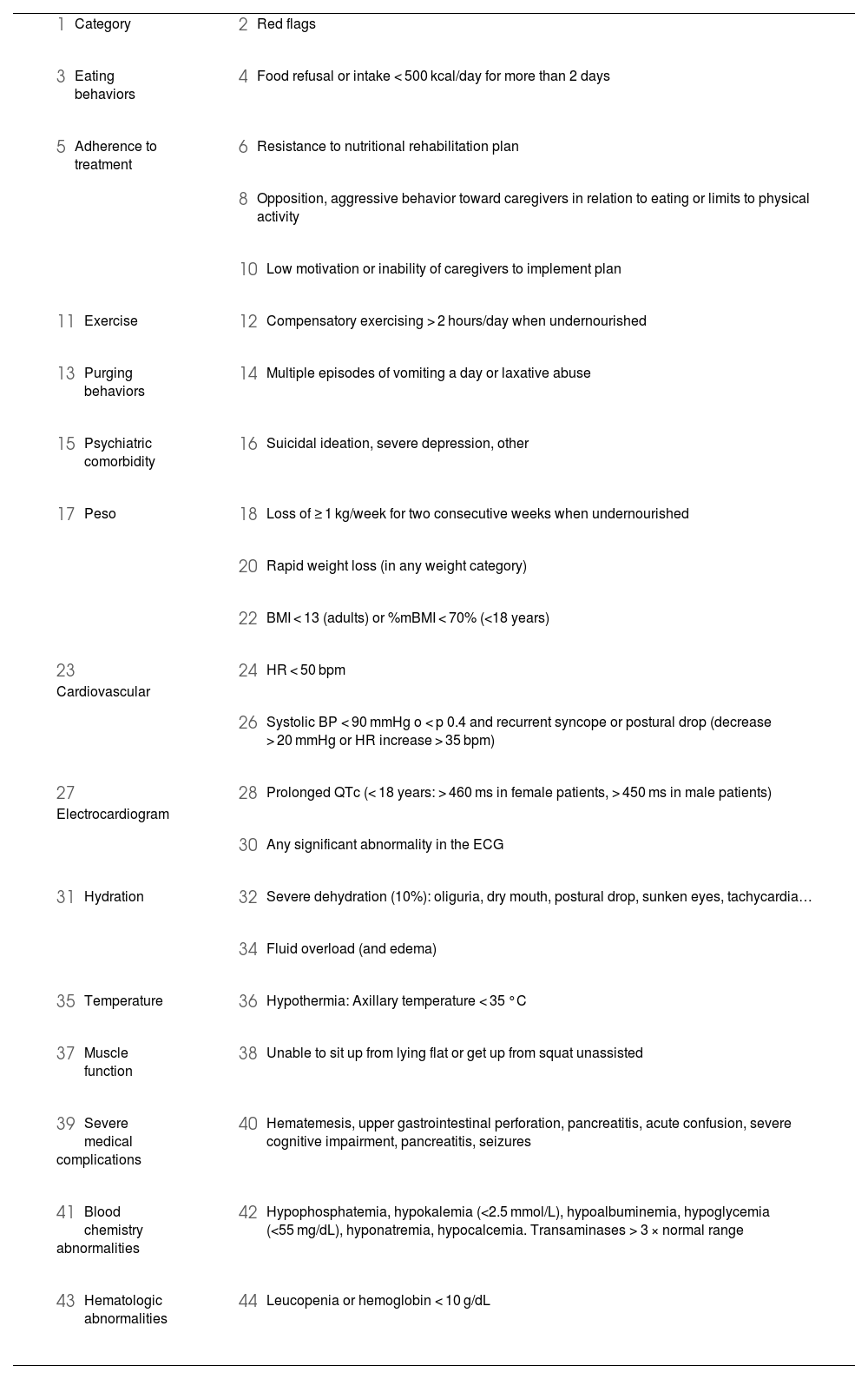
Risk assessment: recognizing the imminent risk to the life of the patientThe first priority in the evaluation of patients with suspected EDs is to assess medical or psychiatric risk to life. This assessment should take place in the first visit, identifying any red flags or high-risk clinical factors indicative of the need for urgent assessment by a specialist or hospital admission, including suicide risk. The goal is to prevent even more severe complications and to pursue medical stabilization (Table 8).26
Criteria warranting urgent admission or specialized assessment.
|
|
|
|
|
|
| |
| |
|
|
|
|
|
|
|
|
| |
| |
|
|
| |
|
|
| |
|
|
| |
|
|
|
|
|
|
|
|
|
|
Abbreviations: BMI, body mass index; BP, blood pressure; ECG, electrocardiogram; HR, heart rate; QTc, corrected QT interval; %mBMI, BMI percentage relative to the median for age and sex = current BMI/median BMI for age and sex × 100.
The pediatrician can provide a clear and understandable explanation of the diagnosis to the patient and the family, underscoring the seriousness of undernutrition and other complications and their potential physical, cognitive and emotional repercussions.
At the same time, it is essential to emphasize that recovery is possible with the right treatment, explaining that progress may not always be linear, for while nutritional status may stabilize early on, changes in cognition and behavior tend to take longer.
Reducing guilt and promoting self-responsibilityIt is important to clarify that neither the patient nor the family are to blame for the eating disorder. The etiology of these disorders is multifactorial and results from the interaction of genetic, biological, psychological and social factors.
“Externalizing” the disorderIt is useful to refer to the ED as an entity separate from the patient. This is particularly valuable when parents feel frustrated about the resistance to refeeding, broken promises, hurtful remarks or inappropriate behaviors of the child. At such moments, it is helpful to remind them that it is the ED, and not the child, who is challenging them. Such reframing may help parents redirect their efforts to fight the disorder, and not the child, fostering greater understanding and empathy in the relationship.
Immediate treatmentIt is essential to convey the need for immediate treatment to the patient and family, underscoring the importance of psychotherapy, weight restoration and adequate nutrition. Caregivers are responsible for guaranteeing nutritional intake in the patient, ensuring that energy requirements are met, in adherence with the treatment plan. Fluid intake also needs to be monitored, ensuring the patient does not drink too little (for fear of fluid retention or weight gain) or too much (to feel full, for cleansing or to “cheat” on weight measurements). The general recommendation is consumption of 1500 to 2000 mL of water a day. Immediate implementation of a dietary intervention is essential to halt the progression of the ED.
Dietary recommendationsA regular eating structure needs to be established, implementing a fixed eating schedule including three main meals and a mid-morning and mid-afternoon snack. Each meal should be balanced, including a combination of carbohydrates, protein and fats and avoiding light/diet food products, restrictive diets or any kind of practice that could sustain a calorie deficit. Portion sizes and calorie density should be adjusted based on weight gain.
It is important to introduce all food groups progressively in order to promote a varied and complete diet. In this process, caving to the “demands of the ED” should be avoided, as it could perpetuate and reinforce maladaptive eating patterns.
A calm atmosphere should be preserved during meals, avoiding any discussion of subjects related to weight, body image or food. The family needs to be present to monitor intake and provide support and emotional containment, guaranteeing that the patient achieves the necessary intake. It is important to listen to the fears of the patient with empathy, avoiding any form of arguing, debate or negotiation that may reinforce the dynamics of the disorder.
To reduce anxiety and prevent controlling behavior, it is recommended that the patient not be involved in grocery shopping or food preparation.
Reducing physical activityLimiting or suspending vigorous physical activity may be necessary until the patient’s weight stabilizes. Physical activity can then resume progressively, working toward rewards other than changes in weight or physical appearance. Rest must also be prioritized, scheduling periods of rest after the main meals to optimize the patient’s physical and metabolic recovery.
Avoiding purging behaviorsSupervising and keeping the patient from going to the bathroom after meals is recommended to prevent purging behaviors. Patients and families should be educated about the risks associated with these behaviors (damage to the esophagus, teeth, electrolyte balance, heart), and the emotional factors that trigger them should be identified. Providers should propose coping strategies, such as distraction techniques, relaxation and emotional support techniques, to get through difficult times.
Weight measurementsDuring the followup, body weight should only be measured under supervision in a clinical setting, such as the doctor or nurse’s office. In the initial stages, it is recommended that patients not be told their weight and to remove scales from the home to prevent an obsessive focus on weight. The frequency of weight measurements will be individualized, adjusting it to the needs of each patient and where the patient is in the recovery process.
Active involvement of the familyProviders must educate caregivers on their key role in patient recovery, especially in regard to meal planning and dietary intake supervision. Caregivers must be given tools to manage conflict and provide emotional support, especially during meals. It is important that both parents be actively involved in the treatment process, acting in a coordinated manner. Involving siblings or other relatives may also be necessary.
Management of the psychological impact in caregiversEating disorders have a significant emotional impact on families and cause high levels of stress. For this reason, pediatricians should assess the emotional wellbeing of caregivers at regular intervals, searching for signs of overburden, burnout or need of additional support.
Management of social media useOpen communication and critical thinking should be promoted in relation to social media use. Supervision and guidance are required to ensure selection of sources and content that promote body diversity and self-esteem, avoiding those that reinforce harmful behaviors and thoughts.
Other resourcesGreater knowledge of the disease allows better support of individuals with ED. Pediatricians can provide information on additional resources, such as support associations (Federación Española de Asociaciones de Ayuda y Lucha contra la Anorexia y la Bulimia [FEACAB], Asociación en Defensa de la Atención a la Anorexia Nerviosa y Bulimia [ADANER], Associació Contra l’Anorèxia i la Bulímia [ACAB]) and patient and family education materials.27–31
Regular follow-up planFollow-up visits should be scheduled at regular intervals and always include monitoring of vital signs (heart rate, blood pressure), weight, BMI, growth and pubertal development, assessing for potential medical complications, both acute and chronic, and monitoring changes in symptoms of the ED and mental status. Pediatricians are in a privileged position to support patients and families and to detect signs or symptoms indicative of relapse or exacerbation after the initial stage of treatment.
Most children and adolescents with eating disorders can be treated on an outpatient basis, provided that regular medical and psychological follow-up is ensured. However, in more severe cases, other resources such as day hospital, hospital admission in specialized units or even hospital-at-home services may be required.32 In the most complex cases, In more complex cases, admission to medium-stay units may be an option. It is important for pediatricians to be aware of the health care resources available in their community to ensure appropriate referral.6,12,14,15
PrognosisThere is substantial variation between studies in the reported long-term outcomes for adolescents with EDs in relation to the methodology, definition of recovery and duration of follow-up. In general, success rates are higher in adolescents compared to adults, with the overall recovery rate ranging between 60% and 70%.6
Compared to the general population, the risk of mortality is six times greater in individuals with AN and nearly double in individuals with BN or UFED.33 Anorexia nervosa has the highest fatality rate among the EDs, resulting from severe medical complications (eg, undernutrition, cardiovascular disturbances, sudden death) and a high risk of suicide. One in five deaths in patients with AN is the result of suicide.33–35
The current evidence indicates that early response to therapy is a reliable predictor of long-term recovery, which supports the need for early intervention and comprehensive treatment, especially in patients with AN.
ConclusionsPediatricians play a key role in the prevention, detection and comprehensive management of EDs. Their role includes the promotion of a healthy relationship with food and the body, early identification of red flags, clinical diagnosis, monitoring of medical complications and coordination of multidisciplinary care. In addition, they provide health education that is essential for patients and families to understand the disease and adjust dietary patterns to meet the needs of the patient.
FundingThis research did not receive any external funding.
The authors have no conflicts of interest to declare.