The use of point-of-care lung ultrasound (LUS) in the neonatal intensive care unit (NICU) allows neonatologists to carry out rapid, real-time, bedside, radiation-free, non-invasive assessments of neonates with respiratory distress and is emerging as a robust alternative to the use of traditional chest radiographs (CXR) for diagnosis.1,2
Although LUS has been integrated into NICU clinical practice,3 there has been a certain lag in integrating it in the training of paediatrics resident physicians, and there is no established curriculum to streamline official accreditation.
We hypothesized that paediatrics residents could readily learn how to use LUS for diagnosis of respiratory distress in neonates through the implementation and standardization of an e-learning and practical skills training programme on neonatal LUS.
We conducted a prospective longitudinal study in a Level III NICU that trains 6 paediatrics residents and manages 350 patients each year.
A total of 21 paediatrics residents with no previous experience in ultrasound received the training.
In the first part of the programme, participants took an e-learning course divided in several online modules developed specifically for paediatrics residents. The theoretical lectures (6 hours) included a combination of text, pictures and videos. The e-learning program included a student evaluation before and after the course consisting of 15 multiple choice questions.
In the practical component of the course (2 hours), the residents in training performed a point-of-care LUS examination under the supervision of a senior consultant in neonatology (SCN) with training on LUS and more than 10 years of experience in the technique.
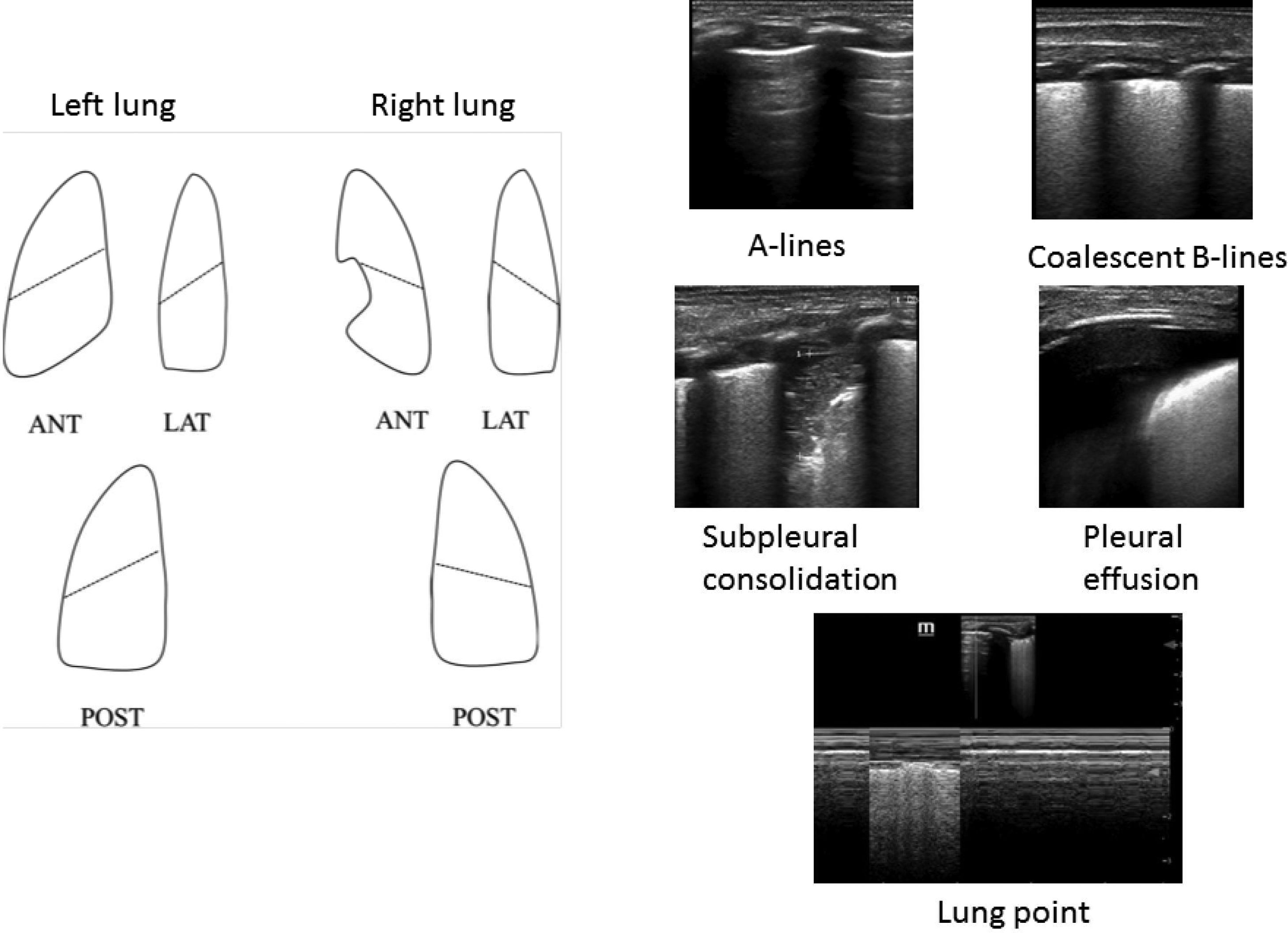
The examinations were performed with a portable ultrasound machine with a 12-MHz linear probe. In adherence to international recommendations,4 the examination included scanning of 3 areas for each hemithorax. The presence of the following had to be evaluated in each of these areas: A-lines, B-lines (number, separation and coalescence), lung sliding (M-mode), pleural line, lung consolidation, subpleural consolidation, lung point and lung pulse (Fig. 1).
Once residents had completed the course, they performed LUS examinations in neonates admitted consecutively to the NICU within 24 hours of birth with signs of respiratory distress. The LUS images were stored and subsequently interpreted by the SCN, and we analysed the agreement with the interpretation of the residents.
We have summarised qualitative variables as absolute and relative frequencies and quantitative variables as mean and standard deviation if the data followed a normal distribution, or otherwise as median and interquartile range.
We measured the level of agreement between the interpretations of the residents and the SCN by means of the kappa coefficient (κ) or the weighted kappa in case of ordinal data. We calculated the coefficients the using the psych package for R. We interpreted kappa values as follows: < 0, poor agreement; 0.01-0.2 slight agreement, 0.21-0.40 fair agreement, 0.41-0.6 moderate agreement, 0.61-0.8 substantial agreement, 0.81-1.00 near perfect agreement. The statistical analysis was performed with the software SPSS®, version 21.0.
The mean score of residents in the assessment before the training was 5.5 points of a possible 15, and the mean score after the training was 13 points.
To evaluate the acquisition of practical skills, the residents performed LUS on 38 neonates, acquiring a total of 228 images (Table 1). Only 1 LUS was performed per patient.
Neonate characteristics and use of non-invasive ventilation at admission.
| Patients (N = 38) | |
|---|---|
| Gestational age (weeks) | 34.5 ± 4 |
| Birth weight (grams) | 2180 ± 650 |
| Caesarean section | 15 (38.3%) |
| 5-minute Apgar | 8 ± 1.5 |
| Male sex | 20 (52.4%) |
| Non-invasive ventilation | 34 (89.2%) |
Data expressed as mean ± standard deviation or n (%). The Apgar score is a dimensionless quantity.
When it came to the presence of A-lines, the overall κ was 0.68 (95% confidence interval [CI], 0.55-0.81), which indicated substantial agreement. For nonhomogeneous B-lines, the overall κ was 0.82 (95% CI, 0.8-0.87), indicative of near perfect agreement. For coalescent B-line patterns, the overall κ was 0.84 (95% CI, 0.82-0.88), indicative of near perfect agreement. When it came to the presence of pleural effusion, the κ was 0.87 (95% CI, 0.83-0.89), corresponding to near perfect agreement.
To our knowledge, this the first study to demonstrate that paediatrics residents can be trained to perform LUS independently and competently in neonates with respiratory distress through the combination of e-learning resources and in-person practical skills training, having found a high level of agreement with the interpretation of the SCN. This is important to consider in developing and implementing a LUS training curriculum.
Previous studies have shown that e-learning resources can be used to teach LUS skills5 and that combining interactive learning resources and different training activities improves skill acquisition. Furthermore, e-learning programmes can achieve results similar to those of traditional classroom-based approaches.6
We believe our approach of integrating an e-learning training programme may be helpful in the context of the health care disruption caused by the current coronavirus disease 2019 (COVID-19) pandemic. Education programmes based on a combination of remote learning and clinical practice in small groups in a safe environment may be useful for continuing medical education.
There are several limitations to our study. The main one is that it was carried in the NICU of a single hospital. In addition, it would have been useful to include a larger number of neonatal patients with other presenting problems. Nevertheless, we believe that it provides valuable information.
Please cite this article as: Rodríguez-Fanjul J, Balaguer Gargallo M, Rodrigo Gonzalo de Liria C, Ginovart G. Formación online en ecografía pulmonar para residentes de Pediatría. An Pediatr (Barc). 2022;97:135–136.
Previous presentation: This study was presented at the 4th joint European Neonatal Societies Congress, September 2021, Athens, Greece.