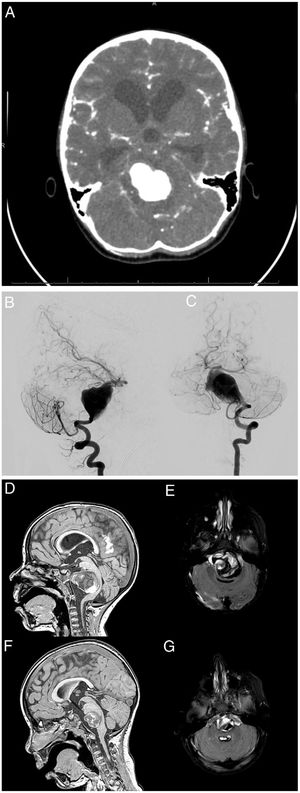
A girl aged 4 years was brought to the emergency department for assessment intense headache and vomiting the onset of which was followed by an episode of loss of consciousness and hypotonia that lasted 5 min. The patient presented with pallor and a Glasgow Coma Scale of 14 points. The mother reported that the patient had suffered from chronic headache for one year. The findings of a CT scan (Fig. 1A) prompted placement of an external ventricular drain. The angiogram (Fig. 1B and C) revealed the presence of an aneurysm in the basilar artery.
(A) The CT scan showed subarachnoid haemorrhage and obstructive hydrocephalus.
Cerebral angiogram. Left vertebral artery series: (B) lateral view and (C) anteroposterior view. Giant fusiform aneurysm in the two lower thirds of the basilar artery. Treatment options like parent artery sacrifice or stent-assisted reconstruction were ruled out on account of the age of the patient and anatomical considerations.
T1-weighted and FLAIR (fluid-attenuated inversion recovery) MRI images: (D) and (E) immediate postoperative period, and (F) and (G) 6 months after surgery. The images show a progressive reduction of the aneurysmal pouch and partial resolution of mass effect and obstructive hydrocephalus.
Parent artery sacrifice and stent-assisted reconstruction were ruled out as treatment options like were ruled out on account of the age of the patient and anatomical considerations. Flow reversal in the parent artery was considered the optimal approach, as the balloon occlusion test of the single left vertebral (with extreme hypoplasia of the right vertebral artery), was performed under neurophysiological monitoring and achieved an adequate deviation of basilar flow. Thus, the aneurysm was managed through endovascular occlusion of the left vertebral artery past the posterior cerebellar artery. An MRI scan was performed after the endovascular intervention (Fig. 1D–G). The patient was discharged at 34 days free of neurologic sequelae.
Cerebral aneurysms are infrequent in children, with an estimated incidence of 0.5%–4.6%. The most common clinical manifestation is headache, followed by syncope and seizures. Partially thrombosed giant aneurysms are a particular subset of aneurysms that should be considered a separate clinical and pathological entity. Due to its histological characteristics and the tendency to exert a mass effect, the optimal treatment is the sacrifice of the parent vessel with open or endovascular surgery. In this article, we present the second paediatric case managed with this approach in our hospital.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.