Obstructed hemivagina with uterus didelphys and ipsilateral renal anomaly (OHVIRA) syndrome, formerly known as Herlyn–Werner–Wunderlich syndrome, is a rare congenital malformation that involves abnormal development of the Müllerian and Wolffian ducts during the development of genitalia in female embryos.1,2 It amounts to 0.16%–10% of all cases of Müllerian malformations.3 The most frequent presentation is an abdominal mass secondary to hematocolpos during adolescence associated with pain and dysmenorrhoea, and diagnosis before puberty is rare. We present 2 cases of OHVIRA syndrome diagnosed prepubertally.
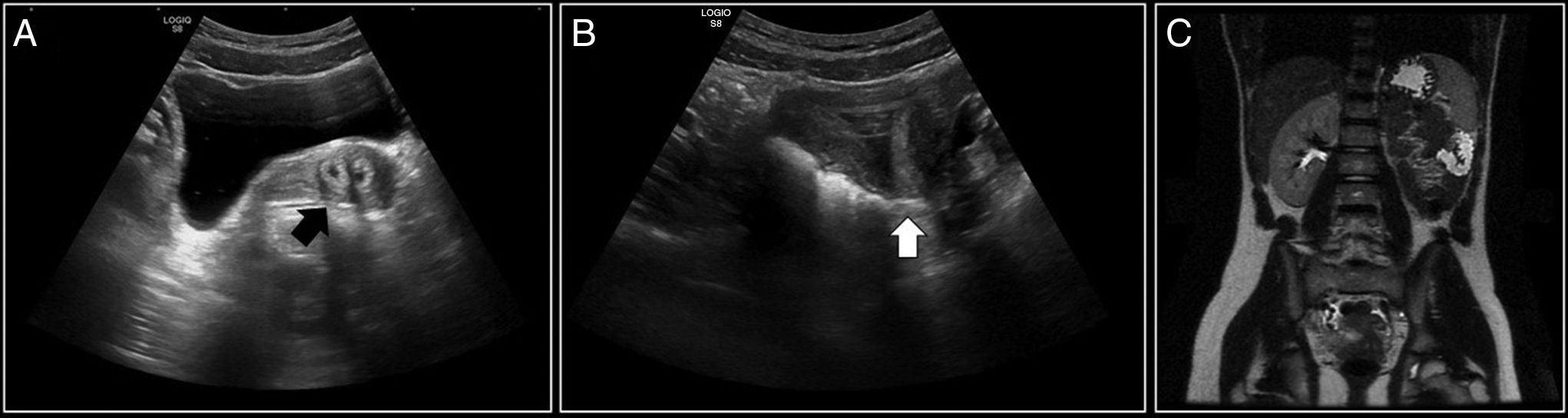
Case 1: girl aged 1 year managed in the nephrology department due to left renal agenesis with a vulvar cyst that became progressively larger. The patient underwent surgical intervention, with incision and full drainage of the cyst, which released a yellowish fluid, and resection of a posterior wall that appeared to form a hemivagina. The patient remained asymptomatic after surgery and was referred at age 13 years due to urinary incontinence and detection by abdominal ultrasound of a bicornuate bicollis uterus with otherwise normal morphology and structure (Fig. 1). The external genitalia appeared normal in the physical examination. A magnetic resonance imaging (MRI) scan revealed compensatory renal enlargement in the right side and features suggestive of a bicornuate uterus (Fig. 1). These radiological findings led to performance of a diagnostic cystoscopy and vaginoscopy. The cystoscopy revealed a smooth-walled bladder with a right ureteral orifice. A left ureteral meatus was not visualised either in the bladder or ectopically in the urethra. The vaginoscopy revealed a normal vagina in the distal two thirds and a vaginal septum in the proximal third associated with a double cervix.
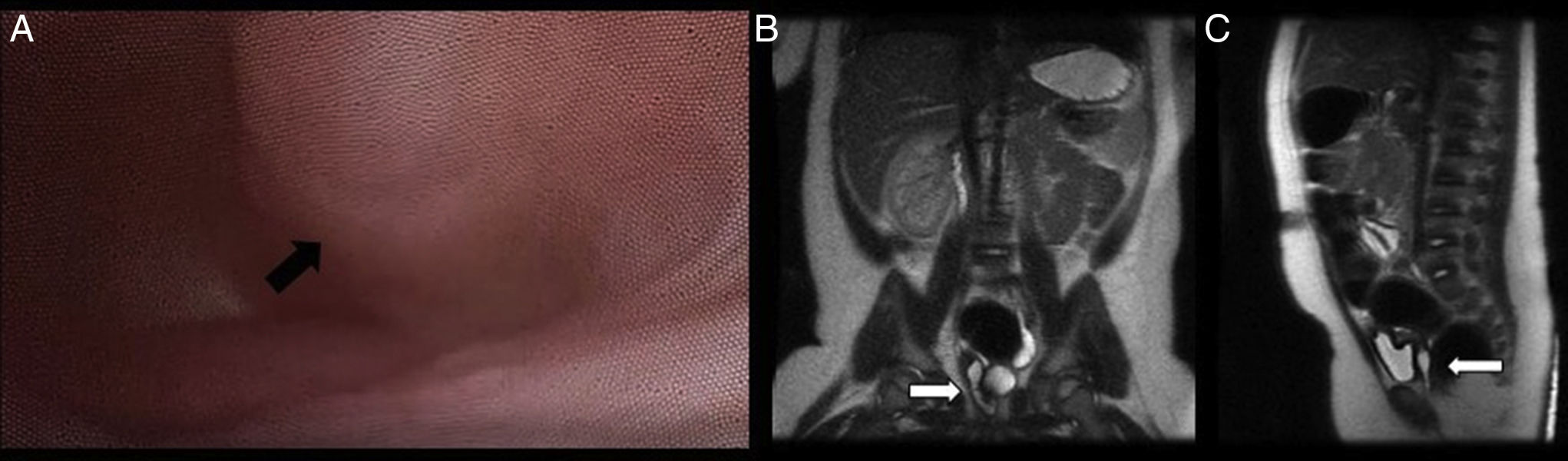
Case 2: girl aged 1 year managed in the nephrology department due to left renal atrophy. A follow-up ultrasound scan revealed a retrovesical cyst in the cervical region measuring 17×12.5mm, with a fixed, regular, vascularised wall. The possible diagnoses that were considered were imperforate hymen, medialised adnexal cyst and persistent urogenital sinus. The evaluation was completed with an MRI scan, which revealed compensatory enlargement of the right kidney and atrophy of the left kidney. A tubular structure was detected posterior to the bladder and anterior to the rectum in the usual location of the vagina that was continuous with the uterus and which extended caudally with a tubular tract that run anteriorly to the rectum with the appearance suggestive of a vagina filled with fluid. There was no evidence of communication between the vagina and the urinary system (Fig. 2). The external genitalia appeared normal on physical examination. Due to the imaging findings, the patient underwent cystoscopy, vaginoscopy and laparoscopy for diagnosis and treatment. The laparoscopy allowed visualisation of a uterus and adnexa of normal appearance, with no abnormalities in the retrovesical or retrouterine space that would compress the vagina. The cystoscopy allowed visualisation of an orthotopic right ureteral orifice, while a left ureteral orifice was not identified either in the bladder or in the urethra. The vaginoscopy revealed a patent vagina and a normal cervix and a paravaginal tubular structure attached to the posterior left wall of the vagina, with no communication between the two, suggesting the presence of an accessory blind hemivagina (Figure 2). The patient underwent resection of the vaginal septum with insertion of a cystoscope in the tubular structure compatible with hemivagina.
Case 2. (A) Vaginoscopy image showing an obstructed hemivagina (arrow) protruding into the vagina. (B) MRI coronal plane showing a tubular structure in the theoretical location of the vagina with fluid contents (arrow). (C) MRI sagittal view showing a retrovesical tubular structure anterior to the rectum (arrow).
Müllerian malformations encompass a broad range of developmental anomalies that result from the defective fusion or regression of the Müllerian ducts during foetal development.1,3 The incidence of OHVIRA is low, occurring in 1 per 2000 to 1 per 28000 women.1 These patients are usually asymptomatic until they reach menarche, when they may present symptoms such a development of a mass secondary to haematocolpos, pelvic or vaginal pain and, less frequently, abdominal pain, vomiting, fever, abnormal vaginal discharge or urine retention.2 However, there have also been cases diagnosed before birth due to detection of a retrovesical mass secondary to hydrocolpos and renal agenesis in ultrasound examinations before birth4 and before puberty.2,5,6 The onset of symptoms in prepubertal patients is less frequent and may involve vulvar or abdominal masses, urinary retention, urinary tract infection, hydrocolpos, pyocolpos or abdominal pain.2 Its clinical diagnosis is challenging, and sonography and MRI are the imaging tests of choice. However, diagnosis during childhood is complicated due to difficulties visualising the uterus and vagina of prepubertal patients in imaging tests due to their small size,5 as occurred in case 1 presented here, in which the diagnosis could not be made until age 13 years, when the presence of a double uterus could be confirmed by imaging. Once the diagnosis is confirmed, the first-line treatment is the resection of the vaginal septum to allow drainage of its contents to the vagina, an intervention associated with a good prognosis and prevents potential complications such as haematometra or pyometra, haematosalpinx or pyosalpinx, endometriosis, pelvic adhesions and infertility.1,5
Please cite this article as: González Ruiz Y, Delgado Alvira R, Siles Hinojosa A, Izquierdo Hernández B, Rihuete Heras MÁ. Diagnóstico prepuberal del síndrome de OHVIRA: ¿es posible? An Pediatr (Barc). 2019;90:244–245.