Developmental centered care (DC) is focused on sensorineural and emotional development of the newborns. In Spain we have had information on the application of DC since 1999, but the extent of actual implementation is unknown.
ObjectiveTo determine the level of implementation of DC in Spanish neonatal units where more than 50 infants weighing under 1500g were cared for in 2012. A comparison was made with previous data published in 2006.
Materials and methodsA descriptive observational cross-sectional study was performed using a survey with seven questions as in the 2006 questionnaire.
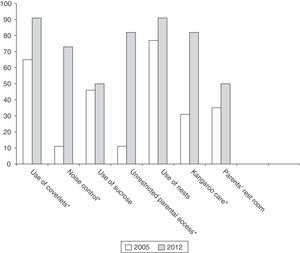
ResultsThe survey was sent to 27 units. The response rate was 81% in 2012 versus 96% in 2006. Noise control measures were introduced in 73% of units in 2012 versus 11% in 2006 (P<.01). The use of sucrose was 50% in 2012 versus 46% in 2006 (P=.6). Parents free entry was 82% in 2012 versus 11% in 2006 (P<.01). Kangaroo care was used without restriction by 82% in 2012 compared to 31% in 2006 (P<.01).
ConclusionsThe implementation of the DC in Spain has improved. There is still room for improvement in areas, such as the use of saccharose or noise control. However, it is important to highlight the positive change that has occurred in relation to unrestricted parental visits.
Los cuidados centrados en el desarrollo (CCD) tienen por objeto favorecer el desarrollo neurosensorial y emocional del niño. En España tenemos información de la aplicación de los CCD desde 1999, pero no se conoce el grado de implantación actual.
ObjetivosDescribir el grado de implantación de los CCD en las unidades neonatales públicas que atendieron a más de 50 recién nacidos con peso menor a 1.500g en el año 2012. Comparación con los datos previos publicados en 2006.
Material y métodosSe realizó un estudio transversal observacional descriptivo incluyendo las unidades neonatales españolas seleccionadas. Se envió un cuestionario con 7 preguntas formuladas de igual manera que en el cuestionario del 2006 para la comparación.
ResultadosSe envió la encuesta a 27 unidades. La tasa de respuesta del 2012 fue del 81% vs. el 96% en 2006. Respecto a medidas de control del ruido, en 2012 fue el 73% vs. el 11% en el 2006 (p < 0,01). El uso de sacarosa fue el 50% en 2012 frente al 46% en 2006 (p = 0,6). La entrada libre de padres en 2012 fue el 82% vs. el 11% en 2006 (p < 0,01). El Método Canguro, en el 2012, se realizó sin limitaciones en un 82% frente al 31% en el 2006 (p < 0,01).
ConclusionesLa implantación de los CCD en España ha mejorado. Todavía hay un margen de mejora en áreas como el uso de sacarosa o el control del ruido, pero hay que resaltar el cambio tan positivo que se ha producido en relación con la entrada de padres.
Developmental care (DC) is care aimed at fostering the neurosensory and emotional development of neonates. The core principles of this type of care are reducing stress, adopting interventions that support infants, recognising the family as a constant point of reference in their lives, even while they are in hospital, and seeing the two (neonate and family) as a unit.1 Family members are integrated into care, form an essential part of it and participate in decisions about their child. DC involves a change of attitude in professionals, who have to adapt their practices to a new health care paradigm.
This type of care is widely established in many European countries. Northern countries have pioneered the change; in southern Europe, however, DC is not yet part of the routine of some units.2 In Spain we have had information about the implementation of DC since 1999.3 At that time, the presence of parents in neonatal units was almost negligible. In 20064 the results of a questionnaire sent to all neonatal units were published. This study showed the extent to which DC was established in Spain. In the last few years, the application of DC in Spanish units seems to have improved substantially, and for this reason the authors of this article decided to send out a new questionnaire to ascertain the level of implementation of DC in Spanish units where more than 50 children weighing under 1500g are cared for per year and to compare the results with those obtained in 2006.
Materials and methodsStudy designA cross-sectional, observational, descriptive study. The study population was defined as neonatal units that care for more than 50 children weighing under 1500g per year. Between June 2012 and October 2012 a questionnaire was sent to these units, following contact by email with a doctor or nurse responsible for this type of care. The questionnaire was based on the one used by the European group led by Marina Cuttini,5 which explores policies on parental access to units, parental involvement in care, the macro-environment of units, pain management and other DC-related issues.
Having established contact by email, by telephone or in person, we sent the questionnaires to the units. The questionnaire was answered online, using the Survey Monkey program, or by email.
In addition, since some of the authors of this study were also authors of the one carried out in 2005 and published in 2006,4 we had access to the questionnaires distributed at that time. From those 2006 questionnaires we selected the surveys of units with more than 50 children weighing under 1500g that were also included in the 2012 questionnaire. Seven questions formulated in a similar way in the two questionnaires (2006 and 2012) were identified (use of canopies or coverlets on incubators, noise control in units, use of nests, use of sucrose, implementation of Kangaroo Care (KC), existence of parents’ rooms and policy on parental access to units). The replies to these seven questions were considered to be comparable.
Finally, regarding the policy on parental access to neonatal units, we carried out a PubMed search which enabled us to identify three studies that provide information on Spanish units,2–4 and we have compared their results with the data obtained in 2012. The first of these studies, published by Cuttini et al.3 in 1999, used different inclusion criteria; the units in Spain that care for more than 20 children weighing under 1500g per year were identified, and subsequently 19 units were randomly selected, of which 18 responded. From the second study, by Perapoch López et al.,4 already mentioned above, we retrieved the data on the units that fulfilled the criteria of the 2012 study. The third, published by Greisen et al.2 in 2012 (conducted in 2009), used the same criteria for selecting units as our study.
Plan of analysisAll the variables analysed are categorical; the results are presented in descriptive form in absolute numbers and in proportions. The results of the studies were compared using the chi-squared test, applying the Yates correction where necessary. The differences were considered significant for P<.05. The analyses were performed using the Statgraphics Centurion XVI program version 16.1.15 (Statpoint Technologies Inc., Warrenton, VA, USA).
ResultsTable 1 lists the public hospitals that cared for more than 50 children weighing under 1500g per year. The response rate in 2012 was 81% (22/27); in 2006, a response rate of 96% (26/27) was obtained.
List of hospitals surveyed.
| Andalusia | Complejo Hospitalario Torrecárdenas | Almería |
| Andalusia | Hospital Universitario Puerta del Mar | Cadiz |
| Andalusia | Hospital Universitario Reina Sofía | Córdoba |
| Andalusia | Hospital Universitario Virgen de las Nieves | Granada |
| Andalusia | Hospital Carlos Haya | Málaga |
| Andalusia | Hospital Materno Infantil Virgen del Rocío | Seville |
| Andalusia | Hospital Virgen de la Macarena | Seville |
| Aragon | Hospital Miguel Servet | Zaragoza |
| Asturias | Hospital Universitario Central de Asturias | Oviedo |
| Cantabria | Hospital Universitario Marqués de Valdecilla | Santander |
| Castile and León | Hospital Universitario, Salamanca | Salamanca |
| Castile-La Mancha | Complejo Hospitalario Universitario de Albacete | Albacete |
| Castile-La Mancha | Hospital Virgen de la Salud | Toledo |
| Catalonia | Hospital Sant Joan de Déu | Barcelona |
| Catalonia | Hospital Materno Infantil Vall d’Hebron | Barcelona |
| Community of Madrid | Hospital Universitario Gregorio Marañón | Madrid |
| Community of Madrid | Hospital Universitario La Paz | Madrid |
| Community of Madrid | Hospital Universitario 12 de Octubre | Madrid |
| Valencian Community | Hospital General Universitario de Alicante | Alicante |
| Valencian Community | Hospital Clínico Universitario | Valencia |
| Valencian Community | Hospital Universitari i Politècnic La Fe | Valencia |
| Balearic Islands | Hospital de Son Dureta | Mallorca |
| Canary Islands | Hospital Materno-Infantil de Canarias | Las Palmas |
| Navarre | Hospital Virgen del Camino, Pamplona | Pamplona |
| Basque Country | Hospital de Cruces Barakaldo | Barakaldo |
| Basque Country | Hospital de Donostia | Donostia (San Sebastián) |
| Region of Murcia | Hospital Universitario Virgen de la Arrixaca | Murcia |
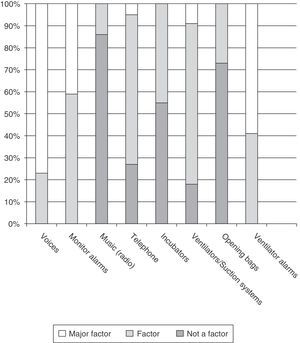
In 2012, 91% (20/22) of the units surveyed used canopies or coverlets over the incubators to provide protection from light versus 65% (17/26) in 2006 (P=.03). As for noise pollution in the units, 73% (16/22) had noise-reduction measures in place in 2012 versus 11% (3/26) in 2006 (P<.01). In 2012, 45% (10/22) of the units continuously measured the noise level. Fig. 1 shows what health care professionals consider to be the main sources of noise.
Specific interventions to help the child develop his or her abilitiesIn 2012, 36% (8/22) of the units surveyed reported that when children were connected to mechanical ventilation they were not placed in any set position by reason of being intubated, 41% (9/22) had them supine, 4.5% (1/22) side-lying, 4.5% (1/22) prone and 14% (3/22) in other positions. In 36% (8/22) children were clothed when the clinical situation permitted (4% in their own clothes and 32% in hospital clothes); in 41% (9/22) they normally wore only a diaper, and in 23% (5/22) a diaper and a cap and/or booties.
Nests or rolls were used around infants to support their posture in 91% (20/22) in 2012 versus 77% (20/26) in 2006 (P=.3).
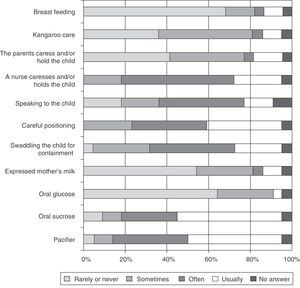
Pain managementFig. 2 shows the comfort measures used before/during painful procedures in the intensive care area in 2012. Of the units surveyed, 41% (9/22) reported that they had a person dedicated exclusively to attending to infants and comforting them during painful procedures, although not continuously. A written protocol for pain management was in place in 73% (16/22) of the units. Sucrose was used as an analgesic when performing any maneuver that could be assumed to cause discomfort in 50% (11/22) in 2012 versus 46% (12/26) in 2006 (P=.6).
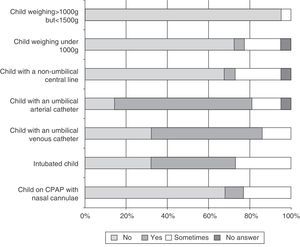
Policy towards parents and family membersIn 2012, 82% (18/22) of the units allowed parents to be with their children in the intensive care area at any time of day, compared with 11% (3/26) in 2006 (P<.01). Fig. 3 shows the procedures during which parents, in 2012, were allowed to accompany their children. In 2012 50% of the units (11/22) had a rest room for parents versus 35% (9/26) in 2006 (P=.28).
As regards kangaroo care (KC), in 2012 82% (18/22) of the units allowed mothers to practice KC without limitations, compared with 31% (8/26) in 2006 (P<.01). In 2012, 73% (16/22) of the units routinely allowed the father to do KC. Other family members were occasionally allowed to perform KC in 9% (2/22) of the units.
Fig. 4 presents the limitations on the practice of KC, in the opinion of the professionals in the units surveyed in 2012. Fig. 5 summarises the comparison of the results obtained in the 2005 questionnaire with those from 2012.
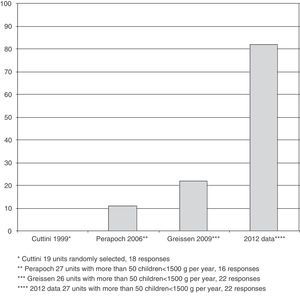
Fig. 6 illustrates the development of policies on parental access according to the data provided in the studies by Cuttini et al. in 1999,3 Perapoch López et al. in 2006,4 as modified, Greisen et el. in 20092 and those obtained in this 2012 study.
DiscussionThis study provides information on the state of DC in 2012 in Spanish neonatal units that care for more than 50 newborn infants weighing under 1500g per year and compares it with the situation in 2006. The results obtained show that during the period from 2006 to 2012 there has been a clear improvement in policies on parental access to units, application of KC and use of noise and light control measures; in other types of care, however, conditions have changed to a lesser degree.
The first study published by Cuttini et al. in 19993 found that unrestricted parental access to neonatal units was almost non-existent. Gradually units became more accessible to families, but not until 2012 do we see them adopting a fully open policy. There has been an improvement in this respect, but further progress needs to be made so that parents are not mere spectators but play an active part in the care of their children. In many Spanish units, as the results of our study show, limits are still placed on the presence of parents when some technique or procedure is to be performed on the child. Several studies have demonstrated that contact between parents and their child during hospitalisation enhances the bond with the child6 and encourages interaction.7 Besides, the child's family is his or her natural environment and it should not be necessary to demonstrate any additional benefit in order to justify the need for children and their parents to be together.
As for KC, many units have also incorporated this type of care on a routine basis, so that in 2012 it is performed in most neonatal units. The fact that units have opened their doors to parents has certainly contributed to the implementation of KC. This is an encouraging development; but it is not yet widespread practice. In a recent study, Spain emerged once again as one of the European countries that most restrict the application of KC.5 Wide disparities in the use of KC are still evident among units; the creation of protocols agreed by all the professionals involved would probably reduce these differences. With this in mind, the guides provided by the World Health Organization could be very helpful.8
With regard to the macro-environment, a significant advance can be observed in noise control. Many neonatal units measure the noise level continuously with sound meters and make use of noise-reduction measures. This greater concern for noise will probably help parents who hear sounds when they are with their children (machines, alarms) that are not familiar to them and that they do not know how to interpret; this makes them anxious and worried and impedes communication with health care staff and even with their own child.9 Parents can be allies to professionals in achieving quiet neonatal units and avoiding the stress caused by noise, which has such a serious effect on children and parents.10 Despite the increase in noise control, almost half the units still did not measure noise levels at all in 2012.
There were also more units in 2012 that had introduced measures to provide protection from light, so that 91% of the units applied some means of controlling it, such as the use of coverlets or canopies. Despite the high level of implementation of some ambient light control procedures, measures for reducing light intensity are the least favourably regarded by professionals of all those related to DC.11
The use of nests to encourage correct posture is almost universally established. In 2006 the level of implementation was already high, and the increase was therefore not significant.
It is striking that administration of sucrose as a non-pharmaceutical analgesic remains at a low level, since although it has increased slightly in the last few years, only 50% of the units used sucrose in their daily routine in 2012. Nor do they routinely use other non-pharmacological analgesic measures that are easy to apply. These data are consistent with those published in a recent study,12 which reveals that the means employed for pain control during such common procedures as heel prick are insufficient and still rarely implemented in most participating European countries. Many studies have demonstrated the importance of minimising and controlling pain, given its short- and long-term effects on premature infants.13,14 In the light of these results, the use of sucrose15 and other measures to achieve greater comfort and adequate pain control should be encouraged.
A limitation of this study is that the information was collected using questionnaires and not by direct observation of the units. Nevertheless, all the data with which we have compared it was collected in the same way, and therefore the positive trend we have identified in implementation of DC very probably reflects the day-to-day situation in the units. Another limitation arises from the fact that the first study we used to compare parental admission policy3 does not use the same criterion for selecting units as the other studies with which we have made comparisons. The frequency of unrestricted parental access in that first study was very low. Even if the number of units allowing parents unrestricted entry was underestimated because of the way the units were selected, in view of the trend in later studies it is very unlikely that the rate was much higher at that time in units that care for more than 50 infants weighing under 1500g per year. Furthermore, the 2006 and 2012 questionnaires were handled anonymously, and therefore no unit-by-unit comparisons have been made, because as the professionals were informed when they were asked for the information, the analyses were performed on an anonymous basis.
This study reveals the major change that is taking place with regard to DC in the neonatal units with the highest level of care in Spain. The degree to which it is applied has increased significantly in the last few years, and the very significant change which has taken place in policies on parental access to neonatal units must be emphasised. The results obtained in this study are very positive, but we have identified certain issues, including such important matters as prevention and treatment of pain, that still require attention from the teams of professionals, in order to achieve continuing improvement in the quality of care provided.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors would like to thank the following institutions for their collaboration: Hospital Universitario Marqués de Valdecilla, Santander; Hospital de Donostia, San Sebastián; Hospital de Cruces, Barakaldo; Hospital Universitario Central de Asturias, Oviedo; Hospital Virgen del Camino, Pamplona; Hospital Miguel Servet, Zaragoza; Hospital Sant Joan de Déu, Barcelona; Hospital Materno Infantil Vall d’Hebron, Barcelona; Hospital Universitario, Salamanca; Hospital Universitario La Paz, Madrid; Hospital Universitario Gregorio Marañón, Madrid; Hospital Universitario 12 de Octubre, Madrid; Hospital Virgen de la Salud, Toledo; Hospital Clínico Universitario, Valencia; La Fe, Valencia; Hospital Universitario Virgen de la Arrixaca, Murcia; Hospital Materno Infantil Virgen del Rocío, Seville; Hospital Virgen de la Macarena, Seville; Hospital Universitario Virgen de las Nieves, Granada; Hospital Universitario Puerta del Mar, Cadiz; Complejo Hospitalario Torrecárdenas, Almería; Hospital Materno-Infantil de Canarias, Las Palmas; and also the Spanish Research Network on Mother and Child Health and Development (SAMID).
We are grateful to the European Science Foundation Network for generously supporting this study by granting us use of the questionnaire they designed to assess the implementation of Developmental Care in Neonatal Units.
Please cite this article as: López Maestro M, Melgar Bonis A, de la Cruz-Bertolo J, Perapoch López J, Mosqueda Peña R, Pallás Alonso C. Cuidados centrados en el desarrollo. Situación en las unidades de neonatología de España. Anales de Pediatría. 2014;81:232–240.