To describe the perceived wellbeing (pWB) and the psychological characteristics of young people with life-limiting and life-threatening conditions (LLTCs).
MethodsWe conducted a cross-sectional study in young people aged 8 years or older with collection of data on demographic and disease-related variables from the health records. In the psychological evaluation, we collected data on emotion regulation, cognitive strategies and risk of depression and anxiety, in addition to the assessment of the pWB through a visual analogue scale. We calculated means and standard deviations and assessed differences in means using the t test. We fitted multiple linear regression models for pWB as a function of sociodemographic, disease-related and psychological variables.
ResultsThe sample consisted of 60 children and adolescents with a mean age of 16.0 (SD, 4.2; range, 9–24), 33.3% female, and with a mean pWB score of 7.0 (SD, 1.8). Forty five percent had emotional symptoms; 46.7% problems with peers, 33.3% behavioural problems, 22% risk of depression, 30% risk of anxiety and 18.3% emotion regulation difficulties. The regression model showed that age 14 years or greater (P&#¿;=&#¿;.03), exacerbated symptoms (P&#¿;=&#¿;.01), the risk of depression (P&#¿;=&#¿;.01) and the use of the rumination and catastrophizing cognitive strategies (P&#¿;<&#¿;.01) had a negative impact on pWB.
ConclusionsYoung people with LLTCs have problems with peers, emotional symptoms and anxious-depressive symptoms. Poorer pWB scores were associated with age 14 years or older, symptom exacerbation, emotional symptoms, depression and the use of rumination and catastrophizing cognitive strategies. Psychological care programmes must respond to these characteristics.
Describir el bienestar percibido (BEp) y las características psicológicas que presentan los jóvenes con condiciones limitantes y/o amenazantes para la vida.
MétodosEstudio transversal con niños de 8 años o más, donde se recogen variables demográficas y de enfermedad a través de la historia clínica. La evaluación psicológica recogió datos sobre regulación emocional, estrategias cognitivas y riesgo de depresión y ansiedad, y sobre su BEp mediante una escala visual analógica. Se calcularon las medias, las desviaciones estándar y la prueba t para diferencias de medias. Se estimaron modelos de regresión lineal múltiple para el BEp en función de variables sociodemográficas, de enfermedad y psicológicas.
ResultadosLa muestra estuvo conformada por 60 niños y adolescentes con una edad promedio de 16,0 (DE&#¿;=&#¿;4,2; rango&#¿;=&#¿;9-24), 33,3% niñas, con un BEp promedio de 7,0 (DE&#¿;=&#¿;1,8). El 45% presentó síntomas emocionales; 46,7% problemas de relación con los pares; 33,3% problemas de conducta; 22% riesgo de depresión y 30% de ansiedad; y 18,3% dificultades de regulación de las emociones. El modelo de regresión estimó una influencia negativa en el BEp el tener 14 años o más (p&#¿;=&#¿;0,03), síntomas exacerbados (p&#¿;=&#¿;0,01), riesgo de depresión (p&#¿;=&#¿;0,01) y el uso de la estrategia cognitiva de rumiación y catastrofismo. (p&#¿;<&#¿;0,01).
ConclusionesLos jóvenes con condiciones limitantes para la vida presentan problemas con sus pares, síntomas emocionales y síntomas ansioso-depresivos. El peor BEp se asocia con tener 14 años o más, presentar síntomas agudizados, tener síntomas emocionales, depresión y estrategias cognitivas de rumiación y catastrofismo. Los programas psicológicos deben responder a estas características.
The World Health Organization estimates that 21 million children worldwide live with life-limiting or life-threatening conditions (LLTCs).1 Published studies2,3 show that every year more than 170&#¿;000 children with terminal illness in Europe need palliative care, while the number in Spain is estimated to be of 25&#¿;000 children. The LLTCs that affect children include solid tumour and blood cancers, neurological, neuromuscular, respiratory, metabolic, and chromosomal disorders and syndromes, malformations, infections and post-anoxic conditions, among others.4
According to international standards for paediatric palliative care (PPC),2 all palliative care programmes should have an established and systematic approach to the psychological and psychiatric aspects of care.5 The relationship between psychiatric disorders and other medical conditions is bidirectional, and the presence of psychiatric comorbidities is associated with greater functional impairment than would be expected otherwise.6 Although there are limited data on the paediatric population with palliative care needs, it is known that children and adolescents who have serious illness experience psychological distress.7,8 Some studies9,10 have found fear of being alone, loss of perspective and loss of independence in children with LLTCs or complex chronic diseases, and a high frequency of severe emotional distress and mood disorders. Anxiety, disruptive behaviours and emotion dysregulation are also common, with prevalence rates ranging from 7% to 50%.
The main objective of this study was to describe the psychological characteristics of young people with LLTCs in our setting and improve our understanding of the relationship between these characteristics and perceived wellbeing. Our main hypothesis was that emotional changes and maladaptive cognitive strategies have an impact on the child’s perceived wellbeing.
Patients and methodsStudy design and settingWe performed a cross-sectional study of the psychological characteristics associated with the perceived wellbeing (pWB) directly self-reported by young patients. The study was conducted on a convenience sample of young people managed in the department of palliative care. We evaluated the wellbeing of all the young people through assessments carried out between June 2021 and August 2023. The study was approved by the Medical Research Ethics Committee (file no. PIC-158-20; 02/06/2020).
Study sampleYoung people with LLTCs were eligible for participation. The additional inclusion criteria were: (1) minimum age of 8 years, (2) fluency in Spanish or Catalan; and (3) signed informed consent from the parents or legal tutors and the patient. The exclusion criterion was the presence in the patient of any cognitive impairment affecting the ability to understand or respond to the questionnaires. The referring health care professional indicated whether the child was capable of participating in the study or not.
Variables and data collectionSenior psychologists from the palliative care service collected data via self-report scales completed by the participating patients. Data on demographic and disease variables were collected from the health records and through questions to health care professionals. Following the completion of a pilot study in 8 paediatric patients to assess the feasibility of using specific tools for children, the psychological assessments were conducted in the recruited sample.
Demographic variables: age and sex, obtained from the health records.
Disease-related variables: we collected data on variables including diagnosis; withholding and withdrawing life-prolonging or life-sustaining measures (the decision to withhold or withdraw diagnostic and therapeutic measures in response to the patient’s condition, avoiding potentially inappropriate interventions and redirecting treatment goals towards comfort and wellbeing); presence of exacerbated symptoms (health professionals assessed whether or not the child was experiencing worsening of physical symptoms such as pain, dyspnoea, fatigue, etc.); whether the disease was or not present from birth and time elapsed from diagnosis, information that was collected from the health records and specific questions answered by health care professionals. To avoid potential sources of bias, health care professionals answered specific questions within a maximum of 3 days so that the time elapsed since the child’s own response would not have a confounding effect.
Psychological variables: different self-report scales validated for young people and adolescents were used for their assessment:
Emotion regulation: we used the repair subscale of the Spanish version of Trait Meta-Mood Scale-24 items (TMMS-24).11 This self-report scale has been adapted for use in adolescents. Respondents are asked to rate their degree of agreement with each item on a 5-point Likert scale ranging from strongly disagree (1) to strongly agree (5). The omega coefficient was 0.85.
Cognitive Strategies of Emotion Regulation: we used a short Spanish version of the Cognitive Emotion Regulation Questionnaire for Spanish Kids (CERQ-Sk).12 This self-report scale has been adapted for use in children and adolescents.12,13 The questionnaire contains 18 items structured in nine subscales (self-blame, acceptance, rumination, positive refocusing, refocus on planning, positive reappraisal, putting into perspective, catastrophizing, and other-blame) that assess what children think after experiencing negative life events and are rated on a 5-point Likert scale (1&#¿;=&#¿;almost never, 5&#¿;=&#¿;almost always). The higher the score on each subscale, the more pronounced the use of the corresponding cognitive coping strategy. In our study, the omega coefficient was 0.73.
Psychosocial functioning: the Strengths and Difficulties Questionnaire (SDQ)14 is a self-report instrument used to assess emotional and behavioural problems in children. It comprises 25 items grouped into 5 dimensions (emotional symptoms, conduct problems, hyperactivity, peer relationship problems and prosocial behaviour). There are three answer choices for each item, scored from 0 to 2 (0 points “not true”, 1 point “somewhat true, and 2 points “certainly true”). Higher scores are indicative of more severe problems on every subscale except for prosocial behaviour. The omega coefficient was 0.57.
Depression and Anxiety symptoms: the questionnaire included 2 items to evaluate depression (PHQ-2) and another 2 for anxiety (GAD-2)15 with a 4-point Likert scale (0-3) response format. These self-report scales have been adapted and used in children and adolescents.16 The cut-off is ≥ 3 points. In our study, the omega coefficient was 0.74.
Child’s perceived wellbeing (pWB): we adapted the Distress Thermometer17 to assess the perceived wellbeing of young patients. The DT is a single-item instrument through which patients rate their general distress level on a 0-10 visual analogue scale. It has also been adapted and validated for use with children with cancer aged 7 to 17 years and caregivers of children with cancer.17 We adapted the item to ask: “In general, how do you rate your wellbeing at the present time?” The young people responded by pressing directly on a screen, and the response ranged from 0 to 10, where 0 corresponded to very bad and 10 to very good.
Statistical analysisWe created the database and analysed the data with the software R, version 4.3.1. We calculated basic descriptive statistics, including the mean and the standard deviation for quantitative variables and the frequency distribution for categorical variables. We assessed the mean differences in pWB between different groups based on social, medical and psychological variables with the Student t test. In addition, we used the Pearson linear correlation to assess the association between pWB and psychological variables. We fitted 3 multivariate linear regression models. Model I included sociodemographic and disease-related factors. Model II also included psychological factors. Model III was fitted through a stepwise selection method and also included sex. We calculated P values and drew conclusions with a level of confidence of 95%.
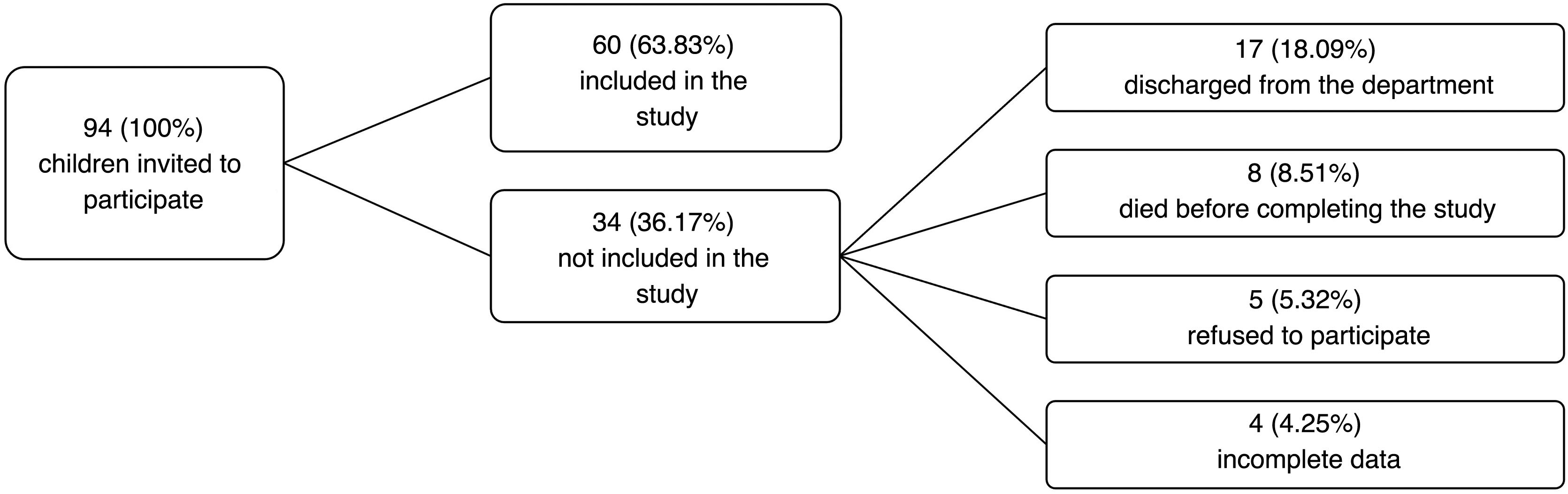
ResultsOf the 94 young people who met the inclusion criteria, 60 (63.83%) participated in the study. Fig. 1 presents a flow chart of the study participants.
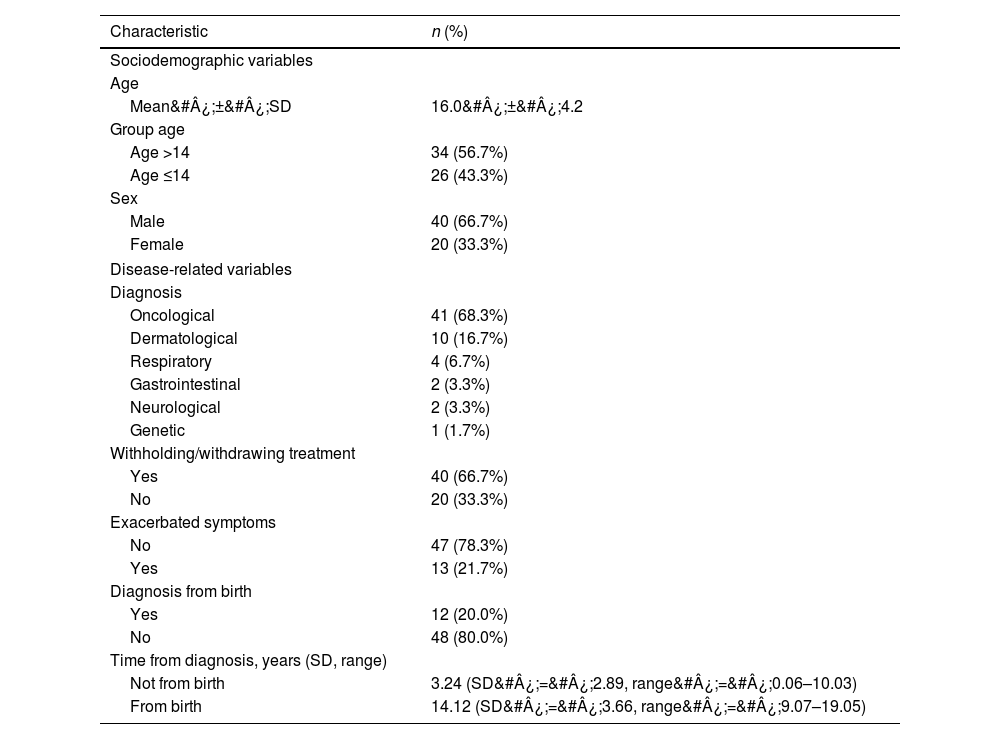
Table 1 presents the characteristics of the sample. The mean age of the paediatric patients was 16.0 years (SD, 4.2; range, 9–24), 20 were female (33.3%), 41 were Spanish nationals (68.3%) and 34 were older than 14 years (56.7%).
Sociodemographic and disease-related characteristics of the patients.
| Characteristic | n (%) |
|---|---|
| Sociodemographic variables | |
| Age | |
| Mean&#¿;±&#¿;SD | 16.0&#¿;±&#¿;4.2 |
| Group age | |
| Age >14 | 34 (56.7%) |
| Age ≤14 | 26 (43.3%) |
| Sex | |
| Male | 40 (66.7%) |
| Female | 20 (33.3%) |
| Disease-related variables | |
| Diagnosis | |
| Oncological | 41 (68.3%) |
| Dermatological | 10 (16.7%) |
| Respiratory | 4 (6.7%) |
| Gastrointestinal | 2 (3.3%) |
| Neurological | 2 (3.3%) |
| Genetic | 1 (1.7%) |
| Withholding/withdrawing treatment | |
| Yes | 40 (66.7%) |
| No | 20 (33.3%) |
| Exacerbated symptoms | |
| No | 47 (78.3%) |
| Yes | 13 (21.7%) |
| Diagnosis from birth | |
| Yes | 12 (20.0%) |
| No | 48 (80.0%) |
| Time from diagnosis, years (SD, range) | |
| Not from birth | 3.24 (SD&#¿;=&#¿;2.89, range&#¿;=&#¿;0.06–10.03) |
| From birth | 14.12 (SD&#¿;=&#¿;3.66, range&#¿;=&#¿;9.07–19.05) |
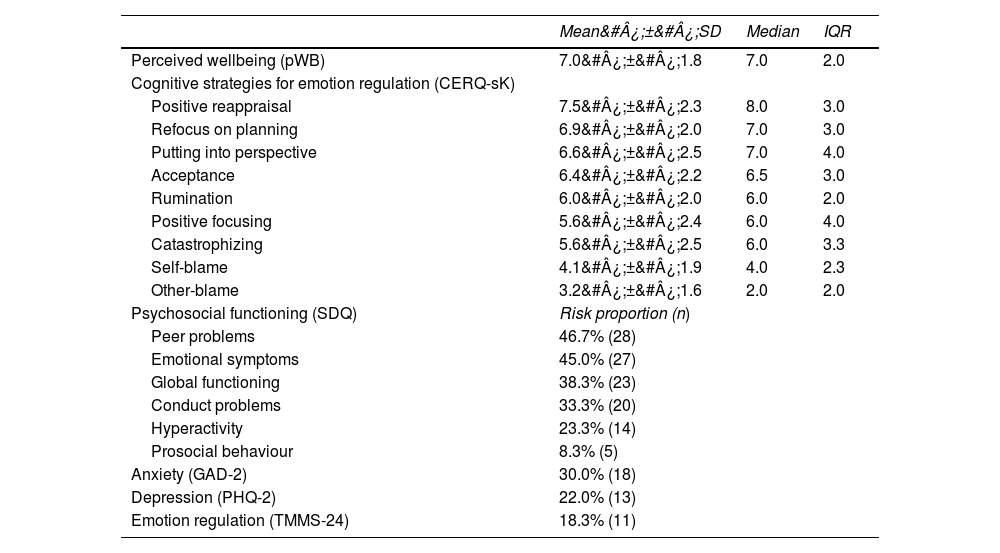
Table 2 presents the data on the pWB of the patients and the different psychological variables assessed. On average, young people rated their pWB as 7 out of 10 (SD, 1.8; range, 3–10; median, 7.0) and 18.3% had difficulties in emotion regulation. When it came to psychosocial functioning, we found the highest risk of problems in the dimensions of problems with peers (46.7%) and emotional symptoms (45.0%). In addition, 30.0% of the young patients were at risk of anxiety and 22.0% at risk of depression. The coping strategy with the highest score was positive reappraisal (mean, 7.5; SD, 2.3; median, 8.0). The correlation coefficient for the strategies of catastrophizing and rumination was 0.72, which suggested that they could be measuring similar aspects. To avoid the inclusion of highly correlated variables and multicollinearity in the models, they were combined and included in the model as a one-dimensional factor.
Descriptive statistics for psychological variables.
| Mean&#¿;±&#¿;SD | Median | IQR | |
|---|---|---|---|
| Perceived wellbeing (pWB) | 7.0&#¿;±&#¿;1.8 | 7.0 | 2.0 |
| Cognitive strategies for emotion regulation (CERQ-sK) | |||
| Positive reappraisal | 7.5&#¿;±&#¿;2.3 | 8.0 | 3.0 |
| Refocus on planning | 6.9&#¿;±&#¿;2.0 | 7.0 | 3.0 |
| Putting into perspective | 6.6&#¿;±&#¿;2.5 | 7.0 | 4.0 |
| Acceptance | 6.4&#¿;±&#¿;2.2 | 6.5 | 3.0 |
| Rumination | 6.0&#¿;±&#¿;2.0 | 6.0 | 2.0 |
| Positive focusing | 5.6&#¿;±&#¿;2.4 | 6.0 | 4.0 |
| Catastrophizing | 5.6&#¿;±&#¿;2.5 | 6.0 | 3.3 |
| Self-blame | 4.1&#¿;±&#¿;1.9 | 4.0 | 2.3 |
| Other-blame | 3.2&#¿;±&#¿;1.6 | 2.0 | 2.0 |
| Psychosocial functioning (SDQ) | Risk proportion (n) | ||
| Peer problems | 46.7% (28) | ||
| Emotional symptoms | 45.0% (27) | ||
| Global functioning | 38.3% (23) | ||
| Conduct problems | 33.3% (20) | ||
| Hyperactivity | 23.3% (14) | ||
| Prosocial behaviour | 8.3% (5) | ||
| Anxiety (GAD-2) | 30.0% (18) | ||
| Depression (PHQ-2) | 22.0% (13) | ||
| Emotion regulation (TMMS-24) | 18.3% (11) |
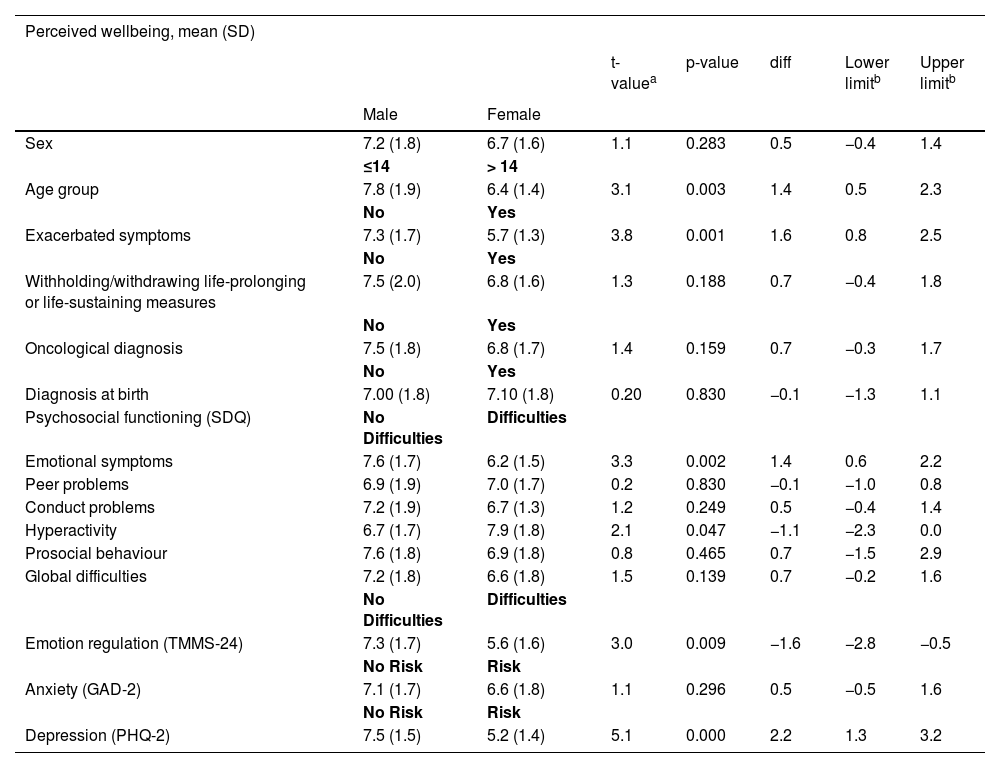
Table 3 presents the results on pWB in relation to the other variables (demographic, disease-related and psychological). It shows a difference in the group aged more than 14 years (mean, 6.4; SD, 1.4) compared to the group aged less than 14 years (mean, 7.8; SD, 19) that was statistically (P&#¿;=&#¿;.003).
Wellbeing in relation to sociodemographic, disease-related and psychological variables.
| Perceived wellbeing, mean (SD) | |||||||
|---|---|---|---|---|---|---|---|
| t-valuea | p-value | diff | Lower limitb | Upper limitb | |||
| Male | Female | ||||||
| Sex | 7.2 (1.8) | 6.7 (1.6) | 1.1 | 0.283 | 0.5 | −0.4 | 1.4 |
| ≤14 | > 14 | ||||||
| Age group | 7.8 (1.9) | 6.4 (1.4) | 3.1 | 0.003 | 1.4 | 0.5 | 2.3 |
| No | Yes | ||||||
| Exacerbated symptoms | 7.3 (1.7) | 5.7 (1.3) | 3.8 | 0.001 | 1.6 | 0.8 | 2.5 |
| No | Yes | ||||||
| Withholding/withdrawing life-prolonging or life-sustaining measures | 7.5 (2.0) | 6.8 (1.6) | 1.3 | 0.188 | 0.7 | −0.4 | 1.8 |
| No | Yes | ||||||
| Oncological diagnosis | 7.5 (1.8) | 6.8 (1.7) | 1.4 | 0.159 | 0.7 | −0.3 | 1.7 |
| No | Yes | ||||||
| Diagnosis at birth | 7.00 (1.8) | 7.10 (1.8) | 0.20 | 0.830 | −0.1 | −1.3 | 1.1 |
| Psychosocial functioning (SDQ) | No Difficulties | Difficulties | |||||
| Emotional symptoms | 7.6 (1.7) | 6.2 (1.5) | 3.3 | 0.002 | 1.4 | 0.6 | 2.2 |
| Peer problems | 6.9 (1.9) | 7.0 (1.7) | 0.2 | 0.830 | −0.1 | −1.0 | 0.8 |
| Conduct problems | 7.2 (1.9) | 6.7 (1.3) | 1.2 | 0.249 | 0.5 | −0.4 | 1.4 |
| Hyperactivity | 6.7 (1.7) | 7.9 (1.8) | 2.1 | 0.047 | −1.1 | −2.3 | 0.0 |
| Prosocial behaviour | 7.6 (1.8) | 6.9 (1.8) | 0.8 | 0.465 | 0.7 | −1.5 | 2.9 |
| Global difficulties | 7.2 (1.8) | 6.6 (1.8) | 1.5 | 0.139 | 0.7 | −0.2 | 1.6 |
| No Difficulties | Difficulties | ||||||
| Emotion regulation (TMMS-24) | 7.3 (1.7) | 5.6 (1.6) | 3.0 | 0.009 | −1.6 | −2.8 | −0.5 |
| No Risk | Risk | ||||||
| Anxiety (GAD-2) | 7.1 (1.7) | 6.6 (1.8) | 1.1 | 0.296 | 0.5 | −0.5 | 1.6 |
| No Risk | Risk | ||||||
| Depression (PHQ-2) | 7.5 (1.5) | 5.2 (1.4) | 5.1 | 0.000 | 2.2 | 1.3 | 3.2 |
Among the disease-related variables, we found significant differences in the presence of exacerbated symptoms (P&#¿;=&#¿;.001).
When we reviewed the mean pWB values in relation to the assessed psychological characteristics, we found statistically significant differences. Lower mean pWB scores were associated with higher scores in emotional symptoms (mean difference [MD], 1.4; 95% CI, 0.6–2.2), and lower scores in emotion regulation (MD, 1.6; 95% CI, 0.5–2.8). Young people at risk of hyperactivity had a higher mean pWB compared to those not at risk (MD, 1.1; 95% CI, 0.0–2.3; P&#¿;=&#¿;.047). This result is not representative because there were few young patients with hyperactivity (n&#¿;=&#¿;14) and most of them (n&#¿;=&#¿;12) rated their pWB at 8 out of 10. Higher scores of depression were associated with lower mean pWB scores (MD, 2.2; 95% CI, 1.3–3.2; P&#¿;<&#¿;.001). We did not find significant differences in the mean pWB in relation to the risk of having anxiety (MD, 0.5; 95% CI, −0.5 to 1.6; P&#¿;=&#¿;.296).
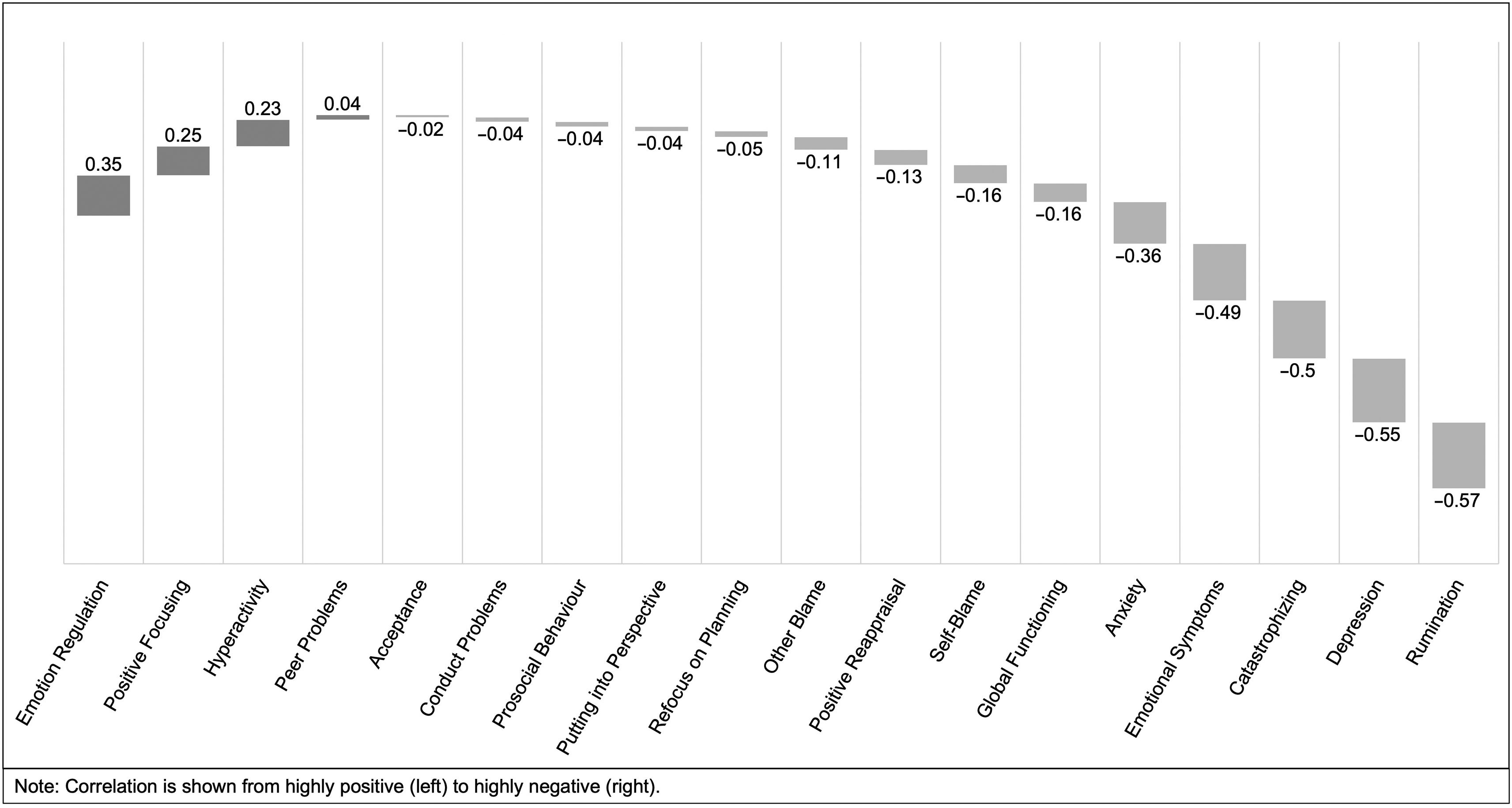
Fig. 2 presents the results on the correlation between pWB and psychological variables. The variables that correlated most strongly with the self-reported pWB of young patients were the cognitive strategy of rumination (r&#¿;=&#¿;−0.57) and the risk of depression (r&#¿;=&#¿;−0.55). The pWB increased with increasing emotion regulation (r&#¿;=&#¿;0.35) and increasing use of the cognitive strategy of positive refocusing (r&#¿;=&#¿;0.25).
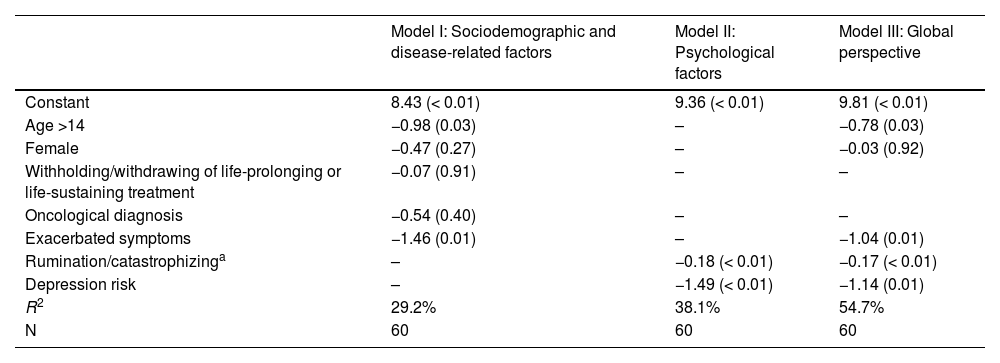
Finally, to assess the predictive value of the variables that best explained the self-reported pWB of young patients, we fitted 3 regression models (Table 4). Model I considered demographic and disease-related variables. It showed that the combination of age greater than 14 years (coef&#¿;=&#¿;−0.98; P&#¿;=&#¿;.03) with the presence of symptom exacerbation (coef&#¿;=&#¿;−1.46; P&#¿;=&#¿;.01) explained 29.2% of the pWB variance. Model II considered the psychological variables, combining the rumination and catastrophizing cognitive strategies into a single variable due to the strong correlation discussed above. The variables risk of depression (coef&#¿;=&#¿;−1.49; P&#¿;<&#¿;.01) and the combined variable of rumination/catastrophizing (coef&#¿;=&#¿;−0.18; P&#¿;<&#¿;.01) were statistically significant. This model explained the variation in pWB with an R2 of 38.1%. To obtain a broader perspective, we decided to incorporate all the analysed variables in Model III. This last model showed that age greater than 14 years (coef&#¿;=&#¿;−0.78; P&#¿;=&#¿;.03), having exacerbated symptoms (coef&#¿;=&#¿;−1.04; p&#¿;=&#¿;0.01), risk of depression (coef&#¿;=&#¿;−1.14; P&#¿;=&#¿;.01) and the cognitive strategies rumination and catastrophizing (coef&#¿;=&#¿;−0.17; P&#¿;<&#¿;.01) explained the variance in pWB with an R2 of 54.7%.
Regression models for pWB as a function of sociodemographic, disease-related and psychological variables.
| Model I: Sociodemographic and disease-related factors | Model II: Psychological factors | Model III: Global perspective | |
|---|---|---|---|
| Constant | 8.43 (< 0.01) | 9.36 (< 0.01) | 9.81 (< 0.01) |
| Age >14 | −0.98 (0.03) | – | −0.78 (0.03) |
| Female | −0.47 (0.27) | – | −0.03 (0.92) |
| Withholding/withdrawing of life-prolonging or life-sustaining treatment | −0.07 (0.91) | – | – |
| Oncological diagnosis | −0.54 (0.40) | – | – |
| Exacerbated symptoms | −1.46 (0.01) | – | −1.04 (0.01) |
| Rumination/catastrophizinga | – | −0.18 (< 0.01) | −0.17 (< 0.01) |
| Depression risk | – | −1.49 (< 0.01) | −1.14 (0.01) |
| R2 | 29.2% | 38.1% | 54.7% |
| N | 60 | 60 | 60 |
The primary objective of our study was to describe the main psychological features exhibited by young people with LLTCs and to improve the understanding of the relationship between these features and perceived wellbeing. The results show that the most prevalent psychological features were problems with peers, emotional symptoms, and anxious-depressive symptoms. The most frequently used “adaptive” cognitive strategies were positive reappraisal and refocus on planning, and the most frequently used “maladaptive” strategies were rumination and catastrophizing. We also found a lower pWB in patients aged 14 years and older, with exacerbated symptoms, with risk of depression and who used the rumination and catastrophizing cognitive strategies.
Our results indicate that patients with LLTCs aged 14 or over reported a poorer pWB compared to younger patients. Other studies show similar results in adolescents and young adults with palliative care needs, whose wellbeing is poorer compared to younger children, with higher rates of depression and anxiety, loss of independence, fear and guilt and a higher prevalence of complex pain.18 This could be a reflection of adolescents’ superior cognitive capacity for logical and abstract thinking, which leads to increased questioning of one’s own values and beliefs, and a greater understanding of the disease that may give rise to more illness-related stressors compared to younger children.19 Children aged 7 to 11 are better at applying their reasoning skills to concrete information compared to abstract concepts20 like pWB. Although more studies are necessary, it is nevertheless widely accepted that sociocultural factors can have an influence on young people’s pWB.21
The presence of exacerbated symptoms was found to be a significant and influential variable in the perception of decreased wellbeing. Other studies have found similar results, with an association between disease progression and higher physical symptom scores.9 Young people with LLTCs express a desire for physical comfort, including pain relief and being able to eat, walk and sleep.19
In our study, the risk of depression and the use of the rumination or catastrophizing cognitive strategies were associated with a poorer pWB and found to be significant in the regression model. Other studies show that palliative care needs substantially increase the risk of experiencing symptoms of anxiety and depression in young people by an estimated 20% to 50%.21 The cognitive strategies used most commonly by young people in our study were adaptive strategies, specifically positive reappraisal and refocus on planning. Even so, we did not find a direct relationship between their use and the pWB. However, the use of maladaptive strategies, such as rumination and catastrophizing, was associated with a decrease in pWB. Other studies show that adaptive coping strategies can be key to improving wellbeing,22 and have found a stronger relationship between these cognitive emotion regulation strategies and the report of depressive symptoms.13 In our study, a high percentage of young people (46.7%) reported problems with their peers. Social interaction with friends is an important coping tool for adolescents and young adults.21 Forty-five percent of the young patients in our study exhibited emotional symptoms. It is known that emotional distress is another psychological challenge faced by young people21 and that higher levels of emotion regulation are associated with a better psychological adjustment to their situation and a better mental health.23 This increases their risk of developing emotional and behavioural problems compared to their healthy peers.24 Young people with LLTCs describe many psychological and emotional repercussions such as anger, worry, sadness and an overwhelming desire to be happy.25 Various studies describe that children may express optimism to maintain a positive mindset,26 that they find it difficult to rate their wellbeing negatively27 or that it may be a way of preserving an appearance of normality. Some children, however, pretend to be brave, possibly to motivate themselves or to protect their parents from feeling guilty or sad.28
Professionals can optimize the wellbeing of young people and their families by identifying the issues that matter to them and working together to set goals and the steps to achieve them. Simple tools and training to support professionals may help them implement this approach.29
Implications for practiceThe results of this study provide greater insight into the variables associated with the perceived wellbeing reported by young people with LLTCs, and can be useful for psychologists and other professionals in paediatric palliative in guiding their evaluation strategy to take these variables into account and adapt their intervention accordingly to improve wellbeing.
The individual management of each child should include cognitive-behavioural therapy, parent management training and relaxation training.30 Narrative techniques also help build rapport between patients and health care professionals, so that the latter can provide relational support, and are also useful in processing emotional and existential aspects. There is growing evidence that acceptance- and mindfulness-based therapeutic approaches, including acceptance and commitment therapy, are beneficial for children with a variety of psychological and physical complaints.31 Group therapies that promote social skills among peers, intrafamily communication and emotional regulation are also useful. The literature available to date shows that psychological interventions are useful for paediatric patients with organic illnesses, but there is still a dearth of evidence in the palliative care setting.
Strengths and limitationsDespite the importance of its findings, there are limitations to our study. First of all, the sample size, use of a cross-sectional design in a non-random sample and the fact that the study was conducted in a single centre hinders the generalizability of the results. Reproducing the study in larger samples and analysing similar populations would be important. Nevertheless, a prospective study in a sample of 60 patients of these characteristics is a particularly strong representation of the population of interest. Secondly, the use of sociodemographic variables could be problematic. The wide age range of the participants may be a confounding variable in the interpretation of the results, as well as in the application of the different self-report scales. Thirdly, the wellbeing assessment was simplified into a single question, but future studies should encompass evaluation of physical, social, psychological and spiritual aspects. Furthermore, most children with LLTCs are aged less than 8 years and/or have cognitive disorders, so a potential future line of research would be to confirm these results in children with these characteristics.
ConclusionsYoung people with LLTCs experience a substantial psychological impact, including problems with peers, emotional symptoms, and anxious and depressive symptoms. The self-perceived wellbeing was poorest in patients aged 14 years of older, with exacerbated symptoms, at risk of depression and who used the rumination and catastrophizing cognitive strategies. These results illustrate the need to work directly with these young people and to guide the psychological evaluation and management with instruments and therapeutic approaches that respond to these characteristics. After obtaining these results, future research could pursue the generalization of these findings in the Spanish population.
CRediT authorship contribution statementDTP conceived and designed the study, designed the data collection instruments, collected data, and drafted and revised the manuscript.
JL and ECR conceived and designed the study, coordinated and supervised data collection, and participated in the critical review of the intellectual content of the manuscript and its editing.
SNV participated in the critical review of the intellectual content of the manuscript and contributed to its drafting and editing.
CB and MG performed the analysis of the results and contributed to the drafting and editing of the manuscript.
The first draft of the manuscript was written by Daniel Toro-Pérez and all authors commented on previous versions of the manuscript. All authors read and approved the final version of the manuscript.
Consent to participationWe obtained the informed consent of all the patients who participated in the study and their parents.
Ethical considerationsAll the procedures that contributed to this study adhered to the ethical standards of the competent national and institutional human research committees and with the Declaration of Helsinki of 1975 as revised in 2008. The study was approved by the Medical Research Ethics Committee of the Sant Joan de Déu Hospital (file PIC-158-20; 02/06/2020).
FundingNo funds, grants, or other support were received by the authors during the preparation of this manuscript.
We would like to express our gratitude to all participating children and parents for contributing to help improve the assessment of young people with life-limiting and life-threatening conditions. We are also grateful to the members of the department of palliative care and complex chronic disease service (Sant Joan de Déu Hospital) and to the ANJANA working group of the Sociedad Catalano-Balear de Cuidados Paliativos (Catalan-Balearic Society of Palliative Care) and the Sociedad Catalana de Pediatría (Catalan Society of Paediatrics) for their support, and for including this study among their research priorities toward the improvement of end-of-life care.