The achievement of oral feeding competence (OFC) is a challenge in preterm infants and can be affected by several factors.
ObjectiveThe aim of our study was to determine the time elapsed to development of OFC in very low birth weight (VLBW, weight <1500g) preterm infants and to identify factors associated with greater difficulty in achieving this skill.
Population and methodsObservational, longitudinal and prospective study in VLBW infants over a period of 7 years (2016–2022). We collected data on perinatal variables, feeding practices and complications associated with prematurity. We analyzed the number of days needed to achieve OFC and which variables predicted greater delay in achieving OFC.
ResultsWe included 145 VLBW infants with a median gestational age (GA) of 29 weeks with a weight of 1247g. Oral feeding was initiated at 33.6 weeks (SD, 1.2) and full oral feeding was achieved at 35.9 weeks (SD, 1.9). The median time to achievement of OFC was 15 days (8–22.5). The variables associated with longer delay of OFC were severe combined morbidity (24 vs 14 days; P<.001) and moderate/severe bronchopulmonary dysplasia (23 vs 14 days; P<.001). In infants without severe combined morbidity, we found no differences in the days elapsed to achievement of OFC between those born before or after 28 weeks of GA (P=.131).
ConclusionsOur findings highlight the importance of structuring the transition to oral feeding and identifying the most at-risk group, which in our study were infants with severe morbidity associated with prematurity, for the purpose of targeting potential interventions.
La adquisición de la competencia para la alimentación oral (CAO) representa un desafío en RN prematuros y puede verse afectada por diversos factores.
ObjetivoEs conocer el tiempo necesario para adquirir la CAO en RN <1500g (RNMBP) e identificar factores asociados a mayor dificultad para alcanzar dicha habilidad.
Población y métodosEstudio observacional, longitudinal y prospectivo durante 7 años (2016-2022) en RNMBP. Se registran variables perinatales, prácticas de alimentación y complicaciones asociadas a la prematuridad. Se analiza número de días necesarios para alcanzar la CAO y qué variables permiten predecir la necesidad de más tiempo para conseguir dicha competencia.
ResultadosSe incluyen 145 RNMBP con una mediana de edad gestacional (EG) 29s y peso 1247g. La alimentación oral se inicia a las 33.6±1.2s y se completan todas las tomas por boca a las 35.9±1.9s La CAO se consigue en una mediana de 15 días (8-22.5). Las variables asociadas a un tiempo más prolongado para alcanzar la CAO fueron: morbilidad combinada grave (MCG) (24 vs. 14 días; p<0.001) y DBP moderada-grave (23 vs.14 días; p<0.001). En la población sin MCG, no se encontraron diferencias en número de días para la CAO en función de EG menor o mayor de 28s (p=0.131).
ConclusionesResaltamos la importancia de estructurar el proceso de transición a la alimentación oral e identificar a la población de más riesgo, que en nuestro estudio fueron los niños con morbilidad grave independientemente de la edad gestacional, para dirigir a ellos las posibles intervenciones.
During the second and third trimester of gestation, a series of complex and interrelated events take place in the foetus that enable proper brain development and allow the maturation of anatomical and functional systems in the newborn.1,2 Preterm birth entails immaturity and is frequently associated with other diseases and developmental disorders.3,4 Among other conditions, preterm (PT) infants may have feeding difficulties associated with their inability to coordinate sucking, swallowing and breathing5 and require enteral feeding through a nasogastric (NG) tube for a variable period of time.
Achieving oral feeding competence (OFC) is a challenge in PT infants, especially those with lower gestational age (GA) (extremely preterm, GA<28 weeks) and with severe complications.6,7 It is known that efficacy in achieving safe and competent oral feeding in PT infants is affected by multiple factors such as GA, muscle tone and the maturity of the nervous system and gastrointestinal tract, in addition to the presence or absence of severe comorbidities.8–10 However, there is little evidence on the role that these factors play in the transition from tube feeding to oral feeding.11 In PT infants, after overcoming severe morbidity and developing conditions associated with prematurity such as bronchopulmonary dysplasia (BPD), intraventricular haemorrhage (IVH) or necrotising enterocolitis (NEC), it is not infrequent for the length of stay to be prolonged due to their difficulties in achieving safe and effective oral feeding.12 Since competent oral feeding without cardiorespiratory compromise is one of the recommended criteria for hospital discharge,6 the longer it takes for the infant to achieve OFC, the longer the hospital stay will be.8,13,14 In addition, feeding difficulties during this period may result in inadequate nutrition, which in turn is associated with extrauterine growth restriction (EUGR) and an increased risk of adverse neurodevelopmental outcomes.15,16
Despite the clinical relevance of the subject, few studies have analysed the process of developing OFC, the factors that influence it and potential interventions to optimise the transition to oral feeding.17–19 Broadly speaking, there are strategies for this transition that are based on specific conditions such as the gestational age or weight of the PT infant, compared to others that are based on the observation of the infant’s feeding skills, which promote the transition to cue-based oral feeding.12,20 A recent Cochrane review concluded that there was insufficient evidence to recommend one approach over the other, highlighting the methodological limitations of the studies.21,22 Even more puzzling is the fact that there is no consensus definition of OFC,23 resulting in substantial heterogeneity in the criteria applied for discontinuation of tube feeding in studies and clinical practice guidelines. Despite the lack of robust evidence, it seems reasonable to assume that an individualised approach to the assessment and promotion of oral feeding skills would be beneficial toward the achievement of safe and competent full oral feeding.
ObjectiveTo determine the time to development of OFC in very low birth weight (VLBW, defined as birth weight <1500g) PT infants in our unit and identify factors associated with an increased difficulty in achieving it.
Population and methodsStudy designWe conducted a prospective longitudinal and observational study in a cohort of VLBW PT neonates admitted to the neonatal unit of our hospital, in which other studies related to infant feeding practices have also been conducted.24 The study was conducted over a 7-year period (2016–2022). The study was approved by the Research Ethics Committee of the hospital.
Description of the unitThe study was conducted in a level IIIB neonatal unit that manages an average of 1800 births and admits 25 to 30 VLBW PT neonates a year.
SampleThe sample included all inborn VLBW PT neonates admitted during the study period. We excluded neonates who were admitted to the unit more than 7 days post birth, transferred to other hospitals before 28 days post birth or died.
As has been done in similar studies and for the purpose of making comparisons, we divided the sample in 2groups based on GA (>28 weeks vs ≤28 weeks) to explore the impact of GA on feeding practices. We also evaluated other factors, such as the presence of complications associated with prematurity or severe comorbidities, infant feeding modalities, opportunities for feeding directly at the breast, history of intrauterine growth restriction (IUGR) and presence of EUGR.
Nutrition protocolOur unit has a protocol for nutritional support in VLBW PT infants that generally adheres to current recommendations. Parenteral nutrition is initiated on day 1 with an initial dose of 6 to 8g/kg/day of carbohydrates, 2–2.5g/kg/day of protein and 1.5–2g/kg/day of lipids, followed by gradual increase of nutrient doses. Since 2017, the unit has a specific protocol for the collection and oropharyngeal administration of colostrum. Trophic feeding is initiated as soon as the patient is stable enough, preferably with the mother’s own milk (MOM). Until June 2018, donor milk (DM) was not available, so in the case MOM was not available, special PT infant formula was used instead. Trophic feeds are increased gradually (20–30mL/kg/day) to a maximum of 160 to 180mL/kg/day. Fortification is introduced once the infant tolerates volumes of 100mL/kg/day; during the study period, standard multicomponent fortification was added to breastmilk and, in the last year, protein supplementation was adjusted based on serum uric acid levels. None of the patients received probiotics.
There is no specific protocol to guide the process of oral feeding skill development. The unit promotes kangaroo care and non-nutritive sucking (NNS) at the breast or on a dummy, independently of GA. The timing of initiation of oral feeding is left to the judgment of the physician in charge, usually based on established criteria such as GA, clinical stability and the subjective perception of the infant’s skills during NNS. Oral feeds were delivered with a bottle in nearly every case, although in recent years the earliest oral feeds were finger-fed through a syringe or cannula. Haemodynamic stability during oral feeds and the volume ingested are the criteria used in the progressive advance towards discontinuation of tube feeding. Since 2019, the unit promotes semi-demand feeding at the breast and the use of a nipple shield if the infant has difficulty latching on. For the purpose of the study, OFC was defined as the infant being able to ingest the full volume planned for the feed, in absence of moderate to severe cardiorespiratory adverse events (defined as a decrease in heart rate to less than 80bpm or a percutaneous oxygen saturation of less than 80% in continuous monitoring), with a weight gain greater than 15g/kg/day.
Clinical variablesWe collected data on demographic and perinatal variables in addition to anthropometric measurements at birth and at discharge. We also documented the presence of NEC, patent ductus arteriosus (PDA) that required surgical closure and moderate to severe BPD. Bronchopulmonary dysplasia was defined and classified according to the 2000 consensus.25 Due to the low prevalence of severe complications in the sample, in order to obtain a representative size and be able to analyse their impact, we defined the combination variable of severe morbidity (SM), defined as the presence of at least one of the following: BPD, surgically corrected PDA, PDA, NEC, IVH grade 3 or 4, leukomalacia, life-threatening malformation or genetic disorder. The reference used in the anthropometric assessments was the Intergrowth-21st charts.26
The primary outcome was the time to achievement of OFC, and we attempted to identify the factors associated with a longer time to achieve competence. To do so, we collected data on variables related to feeding practices: days of parenteral nutrition; chronological age in days at initiation of enteral nutrition; postmenstrual age (PMA) at initiation of oral feeding and at achieving OFC; days from achieving OFC to discharge; length of stay in days; PMA and weight at discharge; infant feeding modalities and practice of feeding at the breast during hospitalization and at discharge. We defined exclusive breastfeeding (EBF) as exclusive feeding of human milk (mother’s own or donor) and mixed feeding (MF) as feeding of both human milk (mother’s own or donor) and artificial formula. We differentiated the specific practice of “feeding at the breast” from “breastfeeding” understood as the consumption of human milk (through feeding at breast or delivered by other means). At discharge, none of the infants met the indications for the prescription of DM, so breastfeeding at discharge always entailed consumption of MOM. We defined IUGR as a birth weight below the 10th percentile and EUGR as a decrease of more than 1 point in the weight z-score between birth and discharge. Given the long study period and the introduction in 2018 of specific measures to support breastfeeding including the availability of DM, we also analysed the possible differences between the periods before and from this year.
Statistical analysisThe statistical analysis was performed with the software IBM SPSS 19 version 25. We described continuous quantitative variables as mean and standard deviation if the data were normally distributed and otherwise as median and interquartile range. We summarised qualitative variables as absolute and relative frequencies, with the latter expressed as percentages.
We compared continuous variables in independent groups with the Student t test if the data followed a normal distribution. Otherwise, we used the nonparametric Mann-Whitney U test. We compared frequencies in qualitative variables by means of the χ2 test or Fisher exact test as applicable. Statistical significance was defined as a P value of less than 0.05.
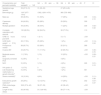
ResultsDuring the period under study, the sample added up to a total of 145 VLBW PT infants (46.9% male) born at a median GA of 29 weeks with a birth weight of 1247g. Table 1 presents the perinatal characteristics of the sample. As expected, the group born at or before 28 weeks comprised more complex cases, with a higher incidence of complications, increased use of resources and a greater PMA at discharge. On the other hand, all infants with IUGR but one belonged to the group born after 28 weeks of gestation.
Description of the sample.
| Characteristics and perinatal morbidity | Total sampleN=145 | GA>28wkn=96 | GA≤28wkn=49 | P | CI |
|---|---|---|---|---|---|
| Gestational age (weeks) | 29 (27.5–31) | 31 (29–32) | 27 (25.5–28) | ||
| Birth weight (g) | 1247 (977–1410) | 1392 (1200–1470) | 960 (735–995) | ||
| Male sex | 68 (46.9%) | 51 (53%) | 17 (35%) | .035 | 0.04–2.10 |
| Caesarean delivery | 94 (64.8%) | 65 (68%) | 29 (59%) | .309 | |
| Multiple gestation | 49 (33.8%) | 38 (40%) | 11 (22%) | .039 | 0.02–0.32 |
| Complete maturation with steroids | 100 (68.9%) | 62 (64.6%) | 38 (77.6%) | .110 | |
| CRIB 12hours post birth | 1 (0–2) | 1 (0–1) | 3 (1–7) | <.001 | |
| IUGR (birth weight<P10) | 26 (17.9%) | 25 (26%) | 1 (2%) | <.001 | 0.14–0.34 |
| Primiparous mother | 88 (60.7%) | 63 (66%) | 25 (51%) | .089 | |
| Invasive MV | 43 (29.7%) | 11 (11.5%) | 32 (65.3%) | <.001 | 0.40–0.70 |
| Moderate-severe BPD | 11 (7.6%) | 1(1%) | 10 (20%) | <.001 | 0.08–0.31 |
| Surgically corrected PDA | 4 (2.8%) | 0 | 4 (8%) | ||
| NEC | 5 (3.5%) | 1(1%) | 4 (8%) | .026 | 0.01–0.15 |
| IVH grade >2 | 1 (0.7%) | 0 | 1 (2%) | ||
| Life-threatening malformation or genetic disordera | 5 (3.5%) | 4 (4%) | 1 (2%) | .561 | |
| Severe morbidityb | 18 (12.4%) | 4(4%) | 14 (29%) | <.001 | 0.11–0.38 |
| Extrauterine growth restrictionc | 29 (20%) | 12 (12.5%) | 17 (35%) | .002 | 0.07–0.37 |
| PMA at discharge (weeks) | 38.9 (37.4–40) | 38 (37–39) | 40 (38–43) | <.001 | |
| Length of stay (days) | 63 (45–83) | 51.5 (40–65) | 89 (77–114) | <.001 |
Categorical variables expressed as n (%); continuous variables expressed as median (IQR).
BPD: bronchopulmonary dysplasia; GA: gestational age; IUGR: intrauterine growth restriction; IVH: intraventricular haemorrhage; MV: mechanical ventilation; NEC: necrotising enterocolitis; PDA: patent ductus arteriosus; PMA: postmenstrual age; P10: tenth percentile.
Includes: distal anal atresia (n=1), malrotation with volvulus (n=1), long-segment Hirschprung disease requiring surgical correction (n=1), Witteveen-Kolk syndrome (n=1), oesophageal atresia (n=1).
As regards feeding practices (Table 2), enteral nutrition was initiated on day 0 or 1 post birth in 61% of the sample, although this was infrequent in the group born at or before 28 weeks (73% vs 37%; P<.001). They received parenteral nutrition for a median of 6 days (IQR, 5–8). Fifty-seven percent of patients were discharged under EBF, and 58% could have at least 1 full feeding at the breast. Infants born at or before 28 weeks required more days of parenteral nutrition, and this group had lower proportions of infants who breastfed (consumed human milk) or could feed at the breast at discharge.
Variables related to infant feeding.
| Feeding-related variables | Total sampleN=145 | GA>28wkN=96 | EG≤28wkN=49 | P | CI |
|---|---|---|---|---|---|
| Initiation of EN on days 0–1 post birth | 88 (61%) | 70 (73%) | 18 (37%) | < .001 | 0.20–0.52 |
| Days of parenteral nutrition | 6 (5–8) | 6 (5–7) | 9 (6–12.5) | < .001 | |
| Initiation of SSC (days post birth) | 3 (2–6) | 2 (1–4) | 6 (4–8) | < .001 | |
| Feeding at breast during stay | 112 (77%) | 85 (89%) | 27 (55%) | < .001 | 0.14–0.45 |
| PMA at initiation of oral feeding | 33.6±1.2 | 33.5±1.02 | 33.7±1.6 | .733 | |
| PMA at achieving OFC (weeks) | 35.9±1.9 | 35.7±1.6 | 36.3±2.5 | .147 | |
| Days to OFC | 15 (8–22.5) | 13 (6.25–21) | 16 (10–25) | .026 | 0.83–8.57 |
| Days from OFC to discharge | 20 (12–30) | 16 (10–24.75) | 26 (16–40.5) | < .001 | |
| Exclusive BF at discharge | 83 (57.2%) | 58 (60%) | 25 (51%) | .279 | |
| BF at discharge | 110 (75.9%) | 80 (83%) | 30 (61%) | .003 | 0.06–0.37 |
| Feeding at breast(at least one full feeding/day) | 85 (59%) | 67 (70%) | 18 (37%) | < .001 | 0.17–0.49 |
| Birth-discharge weight z decrease >1 point | 29 (20%) | 12 (12.5%) | 17 (34.7%) | .002 | 0.07–0.37 |
| PMA at discharge | 38.9 (37.4–40) | 38 (37–39) | 40 (38–43) | < .001 |
Categorical variables expressed as n (%); continuous variables expressed as median (IQR) or mean±SD.
BF, breastfeeding (includes exclusive and mixed feeding); EN: enteral nutrition; GA: gestational age; OFC: oral feeding competence; PMA: postmenstrual age; SSC: skin-to-skin contact.
Overall, oral feeding was initiated at approximately 34 weeks of PMA (mean, 33.6; SD, 1.2) and full oral feeding volumes were achieved around 36 weeks of PMA. Oral feeding competence was achieved at a median of 15 days (IQR, 8–22.5). In the group with GA of 28 weeks or less, oral feeds were initiated at a similar PMA compared to the group with GA greater than 28 weeks, but the time to OFC was longer in former (median, 16 vs 13 days). In addition, once they achieved OFC, infants in the overall sample stayed a median of 20 more days in hospital, a time that was significantly longer in the group born at or before 28 weeks (26 vs 16 days).
The variables associated with a longer time to OFC were the combined SM variable and the presence of moderate to severe BPD (Table 3). Patients that met the definition of SM required a median of 10 more days to develop OFC. Since most patients with SM had been born at or before 28 weeks of gestation, we analysed the time of OFC controlling for gestational age. In the subset without combined SM, we did not find significant differences in the time to OFC based on gestational age (≤28 vs >28 weeks, P=.131).
Analysis of factors associated with the development of oral feeding competence.
| Factor | n | Days to OFC, median (IQR) | P |
|---|---|---|---|
| Gestational age | |||
| GA≤28wk | 49 | 16 (10–25) | .026 |
| GA>28wk | 96 | 13 (6.3–21) | |
| Combined severe morbidity | |||
| Yes | 18 | 24 (16.8–31) | < .001 |
| No | 127 | 14 (7–21) | |
| Group without combined severe morbidity | |||
| GA≤28wk | 35 | 14 (8–22) | .131 |
| GA>28wk | 92 | 12 (6–20.8) | |
| Moderate to severe BPD | |||
| Yes BPD | 11 | 23 (17–42) | .002 |
| No BPD | 134 | 14 (7–22) | |
| Measures to support BF and availability of donor milk | |||
| Period before introduction | 54 | 12 (7–22) | .237 |
| Period after introduction | 91 | 16 (9–23) | |
| IUGR (birth weight<P10) | |||
| Yes | 26 | 8.5 (2.8–22.8) | .033 |
| No | 119 | 15 (9–23) | |
| Exclusive breastfeeding (human milk) at discharge | |||
| Yes | 83 | 16 (10–23) | .014 |
| No | 62 | 11 (6–20) | |
| Breastfeeding (human milk) at discharge | |||
| Yes | 110 | 15 (8–22) | .026 |
| No | 35 | 14 (7–23) | |
| Feeding at breast at discharge (whether exclusive or not) | |||
| Yes | 85 | 16 (9–23) | .360 |
| No | 26 | 13 (7–22) | |
| Twin pregnancy | |||
| Yes | 49 | 13 (7–21) | .406 |
| No | 96 | 15 (8–23) | |
| Extrauterine growth restriction (Decrease >1 point in weight z between birth and discharge) | |||
| Yes | 29 | 15 (11.5–24) | .263 |
| No | 116 | 14.5 (7–22) | |
BF: breastfeeding; BPD: bronchopulmonary dysplasia; IUGR: intrauterine growth restriction; OFC: oral feeding competence; P10: 10th percentile.
The time to OFC was longer in infants who were breastfed at discharge (EBF or MF), independently of gestational age or the presence of severe morbidity. However, the practice of feedings at the breast was not associated with differences in the time required to develop OFC.
Patients with IUGR had a greater GA compared to the rest of the sample (32 vs 29 weeks; P<.001), which is probably why they achieved OFC in fewer days (median of 8.5 vs 15 days; P=.033).
Other factors, such as twin gestation, extrauterine growth restriction, availability of donor milk and the implementation of measures to support breastfeeding did not appear to have an impact.
DiscussionOur study describes the temporal sequence of oral feeding competence acquisition in VLBW PT infants in the context of an established infant nutrition protocol. We also analysed the factors associated with the time required to achieve OFC. Our study was conducted in a sample of VLBW PT infants with long lengths of stay due to, among other circumstances, difficulties in achieving adequate oral feeding. The results allowed the identification of the groups of infants that experienced more difficulties and would be candidates for intervention with the aim of improving the transition to oral feeding.
All the VLBW PT infants in the study, independently of gestational age, achieved OFC before discharge. Similar to the findings of other studies,10 we found that infants in this cohort achieved full oral feeding at a median of 36 weeks of PMA.
Although the PMA at which oral feeding was initiated did not vary based on GA, our findings are consistent with those of previous authors in showing that the time required to achieve full oral feeding increases with decreasing GA9,10,27; thus, we found that PT infants born after 28 weeks of gestation achieved OFC a median of 3 days before infants born at or before 28 weeks. Although the difference was statistically significant, the clinical relevance of 3 days seems small compared to the total length of stay required by these patients. In addition, when we controlled for severe morbidity, which was more prevalent in the cohort born at or before 28 weeks, GA was no longer a statistically significant factor.
According to our findings, unlike those of other studies, it was the presence of SM that had a negative impact on OFC, as opposed to GA less or more than 28 weeks. Patients with SM required a median of 24 days to achieve OFC compared to 14 in the group without SM. Oral feeding was initiated and full oral feeding achieved at greater PMAs in this group of patients with complex morbidity. One important subset of patients with SM are those with moderate to severe BPD, which was independently associated with a longer time to OFC, something that had been described in previous studies.28,29 This seems to be related to the prolonged need of respiratory support, which would affect the sensory afferent arc and the development of oral reflexes in critical periods of development.30
When it came to feeding modalities, our results show that infants discharged with EBF required a median of 5 more days to achieve OFC (16 vs 11; P=.014). A possible explanation is that infants who are exclusively breastfed and feed at the breast require more time to achieve an efficient transfer of milk that would allow discontinuation of tube feeding without a deleterious impact on weight gain. Since most exclusively breastfed infants receive some amount of human milk through a bottle, we applied the same criteria for the definition of OFC in this subset; however, we cannot rule out the possibility of nipple confusion interfering with the acquisition of oral feeding skills and thus delaying OFC.
On the other hand, a history of IUGR was associated with achievement of OFC in fewer days, probably in relation to the greater GA of this group, which entails greater maturity and physiological stability.
Our study identified factors that were associated with delayed acquisition of OFC under a nutrition strategy based on time- and volume-driven feeding, which is common in NICU settings. There are systematic reviews8 that suggest cue-based, responsive or infant-led feeding as a possible alternative that could facilitate the achievement of full oral feeding. It seems logical to assume that if oral feeding does not follow a fixed schedule but is guided by the skills exhibited by the patient, the outcomes will be better. Although the Cochrane review21 yielded no evidence on the subject, it did note that many of the challenges were methodological: there is no consensus definition of OFC, which is a barrier to comparing studies. One salient finding was that once infants developed OFC, which in our study was defined as the definitive removal of the NG tube without clinically significant haemodynamic instability episodes, they still stayed in hospital for a long time: a median of 20 days, which was even longer in infants born at or before 28 weeks of gestation and/or with severe morbidity. The most frequent reason for delaying discharge was the presence of bradycardia and/or mild desaturation during feeds. This raises questions about the criteria currently applied to assess oral feeding competence and whether tube feeding is being discontinued before the infant is truly ready.
Among the limitations of the study, we ought to highlight that we did not document certain variables, such as the amount of time the parents were with the infant or the time spent in kangaroo care, which are clearly associated with the development of OFC. In addition, the unit does not have a specific protocol to guide the transition to oral feeding, which may have resulted in variation in practices between health care providers, but, on the other hand, this is the current reality (clearly in need of improvement) in many neonatal units. In any case, we believe that our study contributes to a better understanding of the factors that affect the development of oral feeding skills in VLBW PT infants.
ConclusionWe believe that the criteria to define and the protocol to promote the development of OFC in VLBW PT infants should be standardised. This would allow performance of methodologically adequate studies, identification of the population at risk and development and assessment of interventions aimed at improving oral feeding skills.
All VLBW PT infants should have access to early care based on the kangaroo care model, with frequent and continuous skin-to-skin contact, non-nutritive sucking, breastfeeding and cue-based feeding to promote oral feeding competence. Based on our findings, we believe that the subset of patients with severe morbidity could benefit from specific therapeutic interventions to improve oral feeding competence.
Previous meeting: Partial results from this study were presented at the XII Congreso Español de Lactancia Materna (Spanish Breastfeeding Congress); April 18–20, 2024, las Palmas de Gran Canaria, Spain.