Criteria for newborn hospital discharge have to include physiological stability and family competence to provide newborn care at home. In this document, the Committee of Standards of the Spanish Society of Neonatology reviews the minimum criteria to be met before hospital discharge of a term newborn infant. We include a review of hospital discharge criteria for the late preterm infants, as these infants are often not hospitalised and remain with their mother after birth. A shortened hospital stay (less than 48h after delivery) for healthy term newborns can be considered, but it is not appropriate for every mother and newborn. Newborn infants discharged before 48h of age, should be examined within 3–4 days of life.
Los criterios para el alta de un recién nacido deben incluir la estabilidad fisiológica y la competencia de la familia para proporcionar los cuidados al recién nacido en el domicilio. En este documento, el Comité de Estándares de la Sociedad Española de Neonatología revisa los criterios de mínimos que se deben dar antes del alta de un recién nacido a término. Se incluye una revisión de los criterios de alta en el caso de recién nacidos prematuros tardíos, debido a que estos recién nacidos frecuentemente no son hospitalizados y permanecen con sus madres tras el nacimiento. Se puede considerar, en recién nacidos a término sanos, una estancia hospitalaria reducida (menor a 48h tras el nacimiento), pero esta no es apropiada para todas las madres y todos los recién nacidos. Aquellos recién nacidos dados de alta antes de las 48h del nacimiento deben ser evaluados entre el tercer y el cuarto día de vida.
The hospital stay of the mother and newborn must be long enough to allow the identification of problems and guarantee that the mother is recovered and prepared enough to care for herself and the newborn at home. Cardiopulmonary problems related to the transition from the intrauterine to the extrauterine environment usually become apparent within 12h from birth. However, other problems such as jaundice, ductal-related cardiac lesions, gastrointestinal obstruction, etc., may require a longer period of observation.1 The length of stay of the mother–infant dyad after delivery has progressively decreased in the past few decades.2 At present, the usual length of stay for healthy newborns in Spain is of at least 48h for vaginal deliveries and 72–96h for caesarean deliveries. This practice is recommended, as in general, existing diseases may manifest during this period, while it also allows for a more accurate assessment of initial feedings and bowel movements and for the time to provide the care and recommendations needed for transitioning to the care of the newborn at home.3
The criteria for NB discharge must include physiologic stability, family preparedness and competence to provide adequate care for the NB at home, and guaranteed access to the health care system and resources. An inadequate assessment in any of these areas prior to discharge can put the NB at increased risk and may result in readmission. Several epidemiological studies have used readmission rates to assess the adequacy of the NB hospital length of stay. However, they have reported readmissions after an early discharge ranging from no increase to a significant increase.2,4,5 These studies consistently identified jaundice, dehydration, feeding difficulties and infection as the most common reason for readmission.6,7 Other frequently reported risk factors for readmission are primiparity, maternal comorbidity, shorter gestation, lower birth weight, assisted delivery and small size for gestational age.1
Readiness for discharge. Perceptions of readiness or unreadiness of the family often differ among paediatricians, midwives, and the mothers themselves. Factors associated with perceptions of unreadiness for newborn discharge include first live birth, maternal history of chronic disease or illness after birth, neonatal illness in the early hours post birth, feeding difficulty, history of inadequate prenatal care and poor social support. In light of this, the American Academy of Paediatrics has recommended the use of checklists that can aid clinicians with the preparation of a newborn for discharge.1,8 The toolkit proposed by the American Academy of Paediatrics mainly focuses on the risk of severe hyperbilirubinaemia, access to breastfeeding support, and coordination of care to improve care for newborns following discharge.
All efforts should be made to keep mothers and newborns together to promote simultaneous discharge.
In this review, we analysed the criteria for the discharge of healthy term newborns, as well as specific criteria for late preterm newborns, who at present often do not require admission to inpatient care and can remain with their mothers. Furthermore, we will analyse the requisites that must be fulfilled for the safe early discharge of newborns.
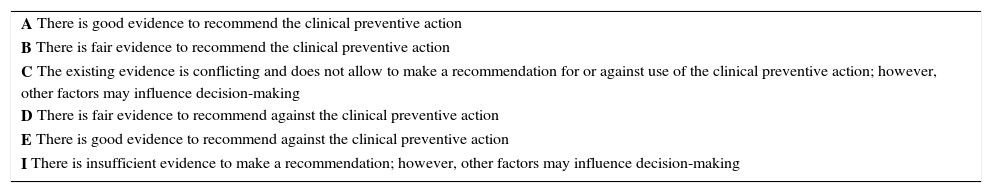
The grade for recommendations was based on the criteria established by the Canadian Task Force on Preventive Health Care (Table 1).9
Grade for recommendations for specific clinical preventive action.
| A There is good evidence to recommend the clinical preventive action |
| B There is fair evidence to recommend the clinical preventive action |
| C The existing evidence is conflicting and does not allow to make a recommendation for or against use of the clinical preventive action; however, other factors may influence decision-making |
| D There is fair evidence to recommend against the clinical preventive action |
| E There is good evidence to recommend against the clinical preventive action |
| I There is insufficient evidence to make a recommendation; however, other factors may influence decision-making |
Source: Canadian Task Force on Preventive Health Care.9
The length of stay of a healthy term newborn must be determined based on the health of the mother, the health and stability of the newborn, the capacity and confidence of the mother in providing care for the newborn, the support available at home and access to appropriate follow-up care. All efforts must be made to keep mothers and newborns together to promote breastfeeding on demand and simultaneous discharge.
Some pathological processes can have an early onset (first 24–48h post birth), even if the newborn seemed healthy at the time of birth and in the first hours of life. Thus, it is recommended that health providers specially trained in paediatrics conduct an evaluation prior to discharge from the hospital.3
The establishment of adequate feeding patterns in the first hours of life is essential to prevent the development of hypernatraemic dehydration problems, which occur frequently when feeding is insufficient.10,11 The subsets of healthy term newborns at highest risk of dehydration are those delivered by caesarean section and those that are exclusively breastfed.12 Since the length of stay is short, in some cases there is not enough time to verify that feeding is well established, so the weight of the newborn must be measured to compare it to the weight recorded soon after birth. This allows the rigorous monitoring of newborns with losses of more than 10% of their birth weights.13
As we have already mentioned, jaundice is one of the most frequent reasons for readmission.6,7 The risk of readmission for jaundice depends on several factors, including the length of stay, and lower rates of early discharge have been associated with lower rates of readmission due to jaundice.14,15 The findings of the medical examination along with the total serum bilirubin measurement can help predict the risk of subsequent severe bilirubinaemia,16 and this prediction is highly accurate when the predischarge total serum bilirubin is combined with gestational age.17 Furthermore, there is evidence that the implementation of predischarge jaundice screening programmes with the use of appropriate nomograms reduces the risk of subsequent admission for significant hyperbilirubinaemia.18 While exposure to natural light may reduce bilirubin levels, its use in our setting is not justified due to the risks associated with sun exposure of a skin surface area large enough to be effective, and therefore is recommended against. There is no evidence that direct exposure, exposure through a pane of glass or exposure to environmental light have beneficial effects in the prevention or treatment of neonatal jaundice.
It is recommended that the following minimum criteria be met before discharge of a term newborn following an uncomplicated gestation and delivery:
- 1.
Healthy term newborns should not be discharged before 48h from birth if delivered vaginally or 72–96h if delivered by caesarean section (B).
- 2.
Absence of evidence of abnormalities in the newborn during the hospital stay and the routine physical examination. This examination must be performed by a physician with a paediatrics specialty at least once, or by a physician with documented experience in neonatal care and under the supervision of a paediatrics specialist (B).
- 3.
It is recommended that the weight, hydration and nutritional status of the newborn be assessed prior to discharge, especially in exclusively-breastfed newborns or those delivered by caesarean section (B).
- 4.
Normal and stable vital signs for at least 12h prior to discharge; axillary temperature between 36.5 and 37.4°C, respiratory rate below 60bpm and no other signs of respiratory distress and an awake heart rate of 100–160bpm.19–21 A resting heart rate of up to 70bpm with no signs of circulatory compromise and adequate responsiveness is also acceptable. A heart rate close to or above the upper bound of the normal range requires further assessment (B).
- 5.
The newborn has urinated regularly and passed at least one stool spontaneously (B).
- 6.
The newborn has completed at least two successful feedings, with assessment to verify that the newborn is able to coordinate sucking, swallowing and breathing while feeding (B).
- 7.
Routine bilirubin measurement in all newborns is not indicated. If the newborn presents with significant jaundice before discharge or is discharged before 48h (early newborn discharge) the total serum bilirubin levels must be measured and compared with risk charts to determine whether the newborn needs phototherapy. Under these circumstances, an appropriate follow-up plan must be instituted (B). Newborns at risk of significant hyperbilirubinaemia must be identified and assessed22:
- a.
Gestational age of less than 38 weeks.
- b.
A previous sibling with neonatal jaundice requiring phototherapy.
- c.
Mother's intention to breastfeed exclusively.
- d.
Visible jaundice in the first 24h of life.
- 8.
The risk factors for infection have been assessed, and, when present, the newborn has been evaluated appropriately and according to established guidelines for the management of newborns with suspected early-onset bacterial sepsis23 (A).
- 9.
The results of maternal blood tests, newborn blood type and direct Coombs test have been reviewed1 (B).
- 10.
Due to the change in the vaccination calendar and delay in the first dose of the Hepatitis B vaccine, a high level of cover must ensure a high coverage for the prenatal screening of pregnant women, with vaccination and immune globulin prophylaxis of newborns of HBsAg+ mothers in the first 24h post birth24 (A).
- 11.
Newborn metabolic25 and hearing26 screenings have been completed according to the specific protocols established for each (A).
- 12.
The mother has been given information and education on how to provide adequate care for her infant,1 and the acquisition of this knowledge and competencies has been confirmed (B).
- 13.
Instructions have been given in regard to the subsequent followup of the newborn, emphatically recommending a first visit in primary care within 72h of discharge, which ideally would be scheduled between the hospital and primary care prior to discharge.3 Directions to follow in case of a complication or emergency must also be given (B).
- 14.
It is advisable to ensure that there have been no misinterpretations of the provided information on the part of the family due to language barriers or physical, psychical or sensory impairments3 (B).
- 15.
Social risk factors have been assessed.1 When any are identified, discharge should be delayed until they are resolved or a plan has been developed to guarantee the safety of the newborn (B).
Late preterm newborns, with a gestational age of 34+0 to 36+6 weeks at birth, frequently receive care in level I units and remain with their mothers after delivery. However, they are immature from a physiological and metabolic standpoint. Consequently, they are at higher risk than term newborns of developing complications, which are associated with increased morbidity and mortality, and have higher rates of readmission during the neonatal period, most frequently due to jaundice, feeding difficulties, dehydration and sepsis.27
The risk factors for readmission or neonatal morbidity identified in this population include: first born child, exclusive breastfeeding at discharge and history of maternal complications during delivery.28,29
The criteria and recommendations for the discharge of late preterm newborns are similar to those for healthy term newborns. However, given the increased risk of neonatal morbidity, the parents of late preterm newborns need to be given specific instructions before discharge and require a more thorough followup thereafter. It is important to educate parents on how to assess for adequate feeding and which signs to watch for to detect dehydration and hyperbilirubinaemia at an early stage. In some instances, this education may require a longer stay after birth. In 2014, the SEN34-36 group of the Spanish Society of Neonatology (Sociedad Española de Neonatología) developed guidelines for the perinatal management and followup of late preterm newborns.30 We would like to highlight the recommendations pertaining to discharge in this article.
The minimum criteria for discharge are similar to those for healthy term newborns, although the following points must be emphasised:
- 1.
Gestational age has been calculated through appropriate methods.
- 2.
The length of stay after birth must be determined on a case-to-case basis and be based on feeding ability, adequate thermoregulation and the absence of disease and social risk factors. Late preterm newborns may not have developed the abilities required for discharge before 48h post birth (B).
- 3.
Medical followup in primary care 24–48h after discharge must be arranged prior to discharge (B). The SEN34-36 group of the Spanish Society of Neonatology recommends a schedule of weekly checkups until 40 weeks’ postmenstrual age.
- 4.
Adequate breastfeeding or bottle feeding for a minimum of 24h has been verified, with evidence of adequate coordination, suction and breathing during feedings (B). The SEN34-36 of the Spanish Society of Neonatology recommends that weight loss during the hospital stay do not exceed 7% of the birth weight.
- 5.
Feeding technique has been assessed thoroughly during the hospital stay following birth (B).
- 6.
A feeding plan has been established, and the family understands it (B).
- 7.
The risk of developing severe hyperbilirubinaemia has been assessed. As noted above, combining the findings of the medical examination with the total serum bilirubin measurement helps predict the risk of severe hyperbilirubinaemia. In this regard, measurement of total serum bilirubin prior to discharge is recommended in all late preterm newborns, especially those that are exclusively breastfed (B).
- 8.
The physical examination of the newborn was conducted by a physician with a paediatrics specialty and ruled out anomalies that could require a longer stay (B).
- 9.
Potential social risk factors have been assessed. When such factors are identified, discharge should be delayed until they are resolved or social services become involved (B).
- 10.
The mother and other potential caregivers have received sufficient information and education to provide adequate care to the infant after discharge, with particular emphasis on specific issues pertaining to late preterm newborns (B).
- 11.
Information on the prevention of sudden infant death has also been provided (A).
In recent decades, the length of stay after delivery has been declining steadily from eight to ten days in 1950 to two to four days today in the countries in our region, changing the concept of early newborn discharge over time.31 Thus, at present an early newborn discharge corresponds to discharge between 24 and 48h post birth, always in newborns from uncomplicated gestations and deliveries. Very early newborn discharge is defined a discharge before 24h post birth.
Some of the potential risks associated with early discharge are those derived from the failure to detect certain anomalies, hypernatraemic dehydration secondary to insufficient feeding, and severe jaundice. However, there are no controlled studies demonstrating an increased risk of readmission, and only one retrospective study conducted in Canada.32 This study compared early discharges in the 1989–1990 and The 1996–1997 periods, and found an inverse correlation between length of stay in days and the risk of readmission. However, the authors did not analyse whether any type of postpartum care was provided at home or in primary care settings in the early days of life.
Some of the advantages of early newborn discharge include increased parental satisfaction and that it facilitates mother–child bonding and the establishment of breastfeeding.33 In this sense, the decision to discharge must be determined on a case-to-case basis taking into account the mother's perception of her ability to take on the care of the newborn and herself. Another advantage would be the optimisation of health care resources resulting from early discharge. Cost analyses performed in Spain have demonstrated cost cuts of 18–20% compared to the usual lengths of stay.34
One essential feature of early discharge programmes is the establishment of a postpartum care plan for the mother and infant that ideally would include a home visit service and guaranteeing at minimum one paediatric visit at the hospital or primary care centre at three to four days post birth.1,15,31,35,36 In this regard, one study found that a group of infants enrolled in an early discharge programme that included home visits made fewer emergency department visits in the first three months of life compared to the group that was discharged following the usual protocol without home visits.37 On the other hand, another two studies did not find differences between home visits and office visits in the associated rates of readmission, duration of breastfeeding and incidence of postpartum depression.38,39
Recommendations for early newborn discharge:
- 1.
Discharge of the newborn before 48h post birth is possible if the following criteria are met (B):
- a.
Absence of family-related, social or environmental risk (teen mother, mental illness, history of domestic violence during pregnancy, substance use, lack of family support or inability of the mother to care for the NB).
- b.
Records of maternal blood tests (HIV, hepatitis B and syphilis).
- c.
Born to term with a weight appropriate for gestational age.
- d.
Normal medical examination findings and vital signs. Absence of disease requiring admission.
- e.
Absence of risk of infection requiring observation.
- f.
Adequate thermoregulation.
- g.
Ability to feed orally and to appropriately coordinate sucking, swallowing and breathing.
- h.
Urination and meconium defecation (at least one bowel movement before discharge).
- i.
In case the maternal blood group is O or Rh-negative, verification that the direct Coombs test of the newborn is negative.
- j.
Absence of significant hyperbilirubinaemia.
- k.
A sample has been collected for metabolic screening. In addition to the sample before discharge, collection of a second sample is recommended at 5–7 days of life.
- l.
Hearing screening has been performed.
- 2.
A written protocol on early newborn discharge must be in place (B).
- 3.
The capacity of the mother to adequately care for the newborn must be assessed before making the decision to discharge (B).
- 4.
The family will be provided with a report covering not only the care given during the stay, but also the post-discharge care and follow-up plan (B).
- 5.
It must be possible for the newborn to have a postnatal checkup (at a hospital or primary care clinic) at 3 or 4 days of life, and this visit should be scheduled prior to discharge from the maternity ward (B).
Should discharge before 24h post birth be requested (very early newborn discharge), the parents will be informed of the risks of discharge under these circumstances and asked to sign an informed consent form.
ConclusionsThe timing of newborn discharge must be decided by a paediatric-specialty physician on the basis of strictly clinical criteria and involving the family in the decision-making process. A shortened hospital stay (of less than 48h following birth) can be considered for healthy term newborns; however, this is not an option for every mother and newborn. In addition to meeting a series of criteria before discharge, early newborn discharge requires a postnatal paediatric visit at day 3 or 4 post birth, which can take place at the hospital or primary care centre. The establishment of standardised processes such as the use of pre-discharge checklists may facilitate a more uniform implementation of the recommendations in the different health facilities that provide neonatal care throughout Spain.
Conflicts of interestThe authors have no conflicts of interest to declare
Please cite this article as: Rite Gracia S, Pérez Muñuzuri A, Sanz López E, Leante Castellanos JL, Benavente Fernández I, Ruiz Campillo CW, et al. Criterios de alta hospitalaria del recién nacido a término sano tras el parto. An Pediatr (Barc). 2017;86:289.