Competency-Based Education is a learning method that has changed the traditional teaching-based focus to a learning-based one. Students are the centre of the process, in which they must learn to learn, solve problems, and adapt to changes in their environment. The goal is to provide learning based on knowledge, skills (know-how), attitude and behaviour. These sets of knowledge are called competencies. It is essential to have a reference of the required competencies in order to identify the need for them. Their acquisition is approached through teaching modules, in which one or more skills can be acquired. This teaching strategy has been adopted by Continuum, the distance learning platform of the Spanish Paediatric Association, which has developed a competency matrix based on the Global Paediatric Education Consortium training programme. In this article, a review will be presented on the basics of Competency-Based Education and how it is applied in Continuum.
La Formación Basada en Competencias es una modalidad formativa que ha cambiado el enfoque tradicional centrado en la enseñanza por otro basado en el aprendizaje. Los alumnos son el centro del proceso, en el que deben aprender a aprender, a resolver problemas y a adaptarse a los cambios en su entorno. El objetivo es lograr un aprendizaje que integre el saber, el saber hacer, el saber ser y el saber estar. A este conjunto de saberes se les denomina competencias. Es fundamental disponer de una referencia de las competencias requeridas para identificar la necesidad de las mismas. Su adquisición se aborda a través de módulos docentes en los que se pueden adquirir una o más competencias. Esta estrategia docente ha sido adoptada por Continuum, la plataforma de formación a distancia de la Asociación Española de Pediatría, que ha desarrollado una matriz de competencias, basada en el programa de formación del Global Pediatric Education Consortium. En este artículo repasaremos los fundamentos de la Formación Basada en Competencias y cómo se aplica en Continuum.
As a result of globalisation and the current mobility of healthcare professionals, we are living in a period of important and complex changes. The healthcare world needs teams of competent professionals, in our case paediatricians, with the knowledge and skills required to provide the best possible care and attention for children and adolescents and for their families: professionals capable of adapting to the setting and circumstances in which care, whether primary or specialist, is delivered, at both national and international level.
In this context, Competency-Based Education (CBE) has emerged, with the aim of achieving greater personal adaptation and development. This educational method, in which the traditional teaching-centred approach has developed into a type of training in which learning is paramount,1,2 has been adopted by Continuum, the distance learning platform of the Spanish Association of Paediatrics. In what follows, we review the basic principles of CBE and how it is applied in Continuum.
Competency-Based EducationIn traditional education the central aim of the teaching-learning process is to convey content; the teacher is the centre of the process, the one who possesses and transmits knowledge, and the student plays a passive role, as a mere receiver. With CBE, in contrast, students are the centre of the teaching–learning process, and the aim is for them to learn how to learn, to solve problems and to adapt to changes in their environment. Its objective is to achieve learning that combines knowledge, skills (know-how), attitude and behaviour. These sets of knowledge are called competencies.
This approach is regarded as one of the most important changes in education in the twenty-first century. Its importance lies in promoting the active participation of students in their own learning, making them aware of their progress and development, helping them to manage their knowledge and to acquire the necessary competencies that will make it easier for them to adapt to a changing and unpredictable environment. It also enables training programmes to be developed more flexibly, so that students learn at their own pace, and it emphasises formative assessment.1
In CBE, those responsible for training play the role of guides to learning, and to achieve this they must design educational experiences that engage students and make them participate actively.
The defining features of CBE are2:
- •
Competencies have to be clearly identified, verified and familiar to all those involved in the education process.
- •
Every training action must be geared towards achieving specific learning outcomes and accompanied by its corresponding assessment.
- •
Assessment must not be based exclusively on evaluating knowledge, but on evidence of learning, such as attitudes and performance. In addition, it must be qualitative (“students are competent or are not yet competent”) and personalised (students are compared with themselves, not with their peers).
- •
Efforts must be made to ensure that the teaching is individualised and tailored to the rate of progress of each participant.
- •
The students must play a part in developing the learning and assessment strategies, which require continuous feedback.
Identifying the competencies needed for professional practice is an essential component of this approach to teaching. They include those required by the official training programme, as well as others that arise in day-to-day practice, as a result of changes in the healthcare environment or of new knowledge or advances in technology. Other sources of information are assessments of training actions and studies carried out to ascertain their real impact. All this provides the system with feedback, expands knowledge of training needs and gradually identifies the set of real competencies.
Competency-Based Education makes it possible to establish a direct relationship between competencies and the contents of training programmes, which are structured in training modules.2 Thus a competency may be developed in more than one training module, and a module, in turn, may address several competencies. Modules in CBE are the learning units that enable objectives, contents and activities to be structured around a problem in professional practice and the competencies we are seeking to develop. The modules may or may not be hierarchically related and go from the general to the specific.2
Any CBE programme must be constructed on the basis of knowledge of the competencies required, developing training actions that make use of all the resources available and conducting assessment processes on their performance, to provide feedback and optimise learning.
Continuum, the distance learning platform of the Spanish Association of PaediatricsAs we have seen, all available learning opportunities must be utilised. Distance learning, with the aid of new technologies, is an efficient method of achieving this, which can be adapted to the student's needs (timetable, pace of work, place of residence, financial means, etc.). Adoption of the principles of CBE has given rise to Continuum, the distance learning platform of the Spanish Association of Paediatrics. It offers training activities designed to cover the competencies (knowledge and skills) that paediatricians need to acquire and maintain in their day-to-day practice. The available content is structured in various types of activity (training courses, new publications, images of the week, interactive clinical cases, knowledge pills, tools) which function as training modules, designed to cover a set of predefined competencies. For this purpose we have developed a competence matrix, which constitutes the teaching structure of Continuum.
The matrix is based on the Global Pediatric Education Consortium3 (GPEC) training programme. This body is made up of leaders of national and regional organisations devoted to education, qualification and accreditation, whose mission is to establish relevant criteria for training and practice in paediatrics at an individual level and to assess their efficacy for ensuring the quality of paediatric learning and care throughout the world. The GPEC curriculum is designed for general paediatric training, in both primary and hospital care, and although it addresses competencies pertaining to specific training areas, with a greater or lesser degree of development, it is not currently intended as a benchmark for training in such areas. Nevertheless, since it is by its nature an open-ended document, it can be supplemented with whatever contributions and improvements professionals in the various training areas consider necessary for their speciality.
The matrix has a hierarchical structure, with 2 generic sections: one for basic abilities and behaviour and another in which the various areas of paediatric knowledge are deployed (Table 1). In the latter, specific, successively subordinated contents are developed, and in each one there are subgroups of competencies related to history, physical, diagnosis and management. The programme has been adapted into Spanish from the original version in English, and as new training actions arise, with teaching aims that are not included in the matrix, modifications are introduced or new competencies are created.
Continuum competency matrix (adapted from GPEC).
| Basic knowledge and patient care programme | ||
|---|---|---|
| Basic abilities and behaviour | Organ- and body system-based content | Palliative care, surgery, rehabilitation and sports medicine |
| 1. Ethics in clinical practice | 1. Allergy | 1. Palliative care |
| 2. Collaboration | 2. Cardiology | 2. Peri- and post-operative care |
| 3. Global health awareness | 3. Dermatology | 3. Rehabilitation |
| 4. Patient safety and quality improvement | 4. Endocrinology | 4. Sports medicine |
| 5. Research principles and evidence-based practice | 5. Gastroenterology and Hepatology | |
| 6. Scholarly activities | 6. Haematology | Developmental issues |
| 7. Self-leadership and practice management | 7. Immunology | 1. Behaviour and mental health |
| 8. Communication and interpersonal skills | 8. Infectious diseases | 2. Genetics |
| 9. Health advocacy and children's rights | 9. Metabolism | 3. Growth and development |
| 10. Professionalism | 10. Musculoskeletal disorders | 4. Language, learning and sensory disorders |
| 11. Neonatal care | 5. Nutrition | |
| Basic skills | 12. Nephrology | 6. Psychosocial functioning |
| 1. Assessment and diagnostic skills | 13. Neurology | |
| 2. Basic therapeutic skills | 14. Oncology | Adolescence and related issues |
| 3. Basic procedural skills | 15. Ophthalmology | 1. Adolescent medicine |
| 16. Oral and dental | 2. Gynaecology | |
| 17. Otolaryngology | ||
| 18. Pharmacology | Problems of abuse | |
| 19. Respiratory | 1. Child abuse and neglect | |
| 20. Rheumatology | 2. Substance abuse | |
| 21. Urology | ||
| Community and preventive paediatrics | ||
| Emergency and critical care for children | 1. Community paediatrics | |
| 1. Critical care in children | 2. Preventive paediatrics | |
| 2. Critical care in neonates | ||
| 3. Emergency medical care | ||
| 4. Disorders of fluid, electrolyte and acid-base balance | ||
| 5. Toxicological and poisoning emergencies | ||
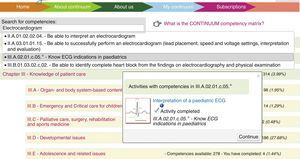
To facilitate locating items in the matrix, each competency is assigned a hierarchically structured code (see Tables 2 and 3). This means that when students perform an activity, they can find out what results they can achieve with it.
Partial selection of areas of competencies related to electrocardiograms.
| II. | Basic skills |
| II.A.03. | Basic procedural skills |
| II.A.03.01. | Performing basic procedures |
| II.A.03.01.01. | Be able to successfully perform basic procedures: |
| … | |
| II.A.03.01.01.15. | Be able to successfully perform an electrocardiogram (lead placement, speed and voltage settings, interpretation and evaluation) |
| … | |
| III. | Basic knowledge and patient care programme |
| III.A. | Organ- and body system-based content |
| III.A.02. | Cardiology |
| III.A.02.01. | General issues |
| … | |
| III.A.02.01.c. | Diagnosis |
| … | |
| III.A.02.01.c.04. | Be able to identify the most common ECG abnormalities |
| III.A.02.01.c.05.* | Know ECG indications in paediatrics |
| … | |
| III.A.02.06. | Rate and rhythm disorders |
| III.A.02.06.a. | History |
| III.A.02.06.a.01. | Know the causes of arrhythmias |
| III.A.02.06.b. | Physical |
| III.A.02.06.b.01. | Be able to identify the clinical manifestations of the most common cardiac arrhythmias |
| III.A.02.06.c. | Diagnosis |
| III.A.02.06.c.01. | Be able to identify a benign arrhythmia |
| III.A.02.06.c.02. | Be able to recognise the most common dysrhythmias using ECG |
| III.A.02.06.c.03. | Be able to differentiate arrhythmias that require urgent therapy from those that require chronic therapy or no therapy |
| III.A.02.06.c.04. | Be able to understand the clinical significance of a prolonged corrected QT interval |
| III.A.02.06.c.05. | Be able to identify premature atrial contractions, premature ventricular contractions, supraventricular tachycardia and ventricular tachycardia using electrocardiographic patterns |
| III.A.02.06.c.06.* | Be able to identify ECG abnormalities suggestive of conduction disturbances, complete or incomplete right bundle branch block, left bundle branch block, pre-excitation and Wolff-Parkinson-White syndrome |
| III.A.02.06.c.07.* | Be able to identify electrocardiographic findings suggestive of channelopathies: long QT syndrome, short QT syndrome and Brugada syndrome |
| III.A.02.06.d. | Management |
| … |
… Areas of the matrix not referenced in the table.
Competencies related to 3 training activities.
| Image of the week: self-limiting palpitations in an 11-year-old boy | |
| II.A.01.02.02.04. | Be able to interpret an electrocardiogram |
| III.A.02.06.c.01. | Be able to identify a benign arrhythmia |
| III.A.02.06.c.02. | Be able to recognise the most common dysrhythmias using ECG |
| Interactive clinical case: football and chest pain: is it what we do not want it to be? | |
| II.A.01.02.02.04. | Be able to interpret an electrocardiogram |
| III.A.02.01.c.03. | Be able to select and interpret appropriate cardiological investigations |
| III.A.02.01.c.04. | Be able to identify the most common ECG abnormalities |
| III.A.02.02.02.a.02. | Recognise the importance of cardiovascular evaluation in patients with chest pain associated with exercise |
| III.A.02.02.02.a.03. | Know the cardiovascular causes of chest pain |
| III.A.02.06.b.01. | Be able to identify the clinical manifestations of the most common cardiac arrhythmias |
| III.A.02.06.c.05. | Be able to identify premature atrial contractions, premature ventricular contractions, supraventricular tachycardia and ventricular tachycardia using electrocardiographic patterns |
| III.A.02.06.d.03. | Be able to plan for the treatment of supraventricular tachycardia |
| Training course: systematic interpretation of a paediatric ECG | |
| II.A.01.02.02.04. | Be able to interpret an electrocardiogram |
| II.A.03.01.01.15. | Be able to successfully perform an electrocardiogram (lead placement, speed and voltage settings, interpretation and evaluation |
| III.A.02.01.c.04. | Be able to identify the most common ECG abnormalities |
| III.A.02.01.c.05.* | Know ECG indications in paediatrics |
| III.A.02.02.02.c.02. | Be able to identify the abnormal ST-T changes on the ECG |
| III.A.02.05.05.c.03.* | Be able to identify electrocardiographic findings suggestive of pericarditis |
| III.A.02.05.06.c.01. | Be able to identify post-operative X-ray and electrocardiographic changes |
| III.A.02.06.c.01. | Be able to identify a benign arrhythmia |
| III.A.02.06.c.02. | Be able to recognise the most common dysrhythmias using ECG |
| III.A.02.06.c.03. | Be able to differentiate arrhythmias that require urgent therapy from those that require chronic therapy or no therapy |
| III.A.02.06.c.04. | Be able to understand the clinical significance of a prolonged corrected QT interval |
| III.A.02.06.c.05. | Be able to identify premature atrial contractions, premature ventricular contractions, supraventricular tachycardia and ventricular tachycardia using electrocardiographic patterns |
| III.A.02.06.c.06.* | Be able to identify ECG abnormalities suggestive of conduction disturbances, complete or incomplete right bundle branch block, left bundle branch block, preexcitation and Wolff-Parkinson-White syndrome |
| III.A.02.06.c.07.* | Be able to identify electrocardiographic findings suggestive of channelopathies: long QT syndrome, short QT syndrome and Brugada syndrome |
| III.A.02.08.c.01. | Be able to identify the diagnostic features of chest X-ray, electrocardiogram and echocardiogram of cardiomyopathies |
| III.A.04.02.10.c.03.* | Know the electrocardiographic changes produced by hypocalcaemia |
| III.A.04.02.11.c.03.* | Know the electrocardiographic changes produced by hypercalcaemia |
| III.B.01.03.02.c.02. | Be able to identify complete heart block from the findings on electrocardiography and physical examination |
| III.B.01.03.02.c.04. | Recognise prolonged QT syndrome in a patient with syncope |
| III.B.04.04.02.b.01. | Know the electrocardiographic changes produced by hypo- and hyperkalaemia |
In addition, the matrix enables students to locate the competencies they are interested in and to look up the activities that the platform offers for acquiring them (www.bit.ly/continuumcompt). They thereby obtain a personalised view of their training curriculum or virtual portfolio (once they have registered and identified themselves), showing the competencies they have covered in each area and those they have yet to attain.
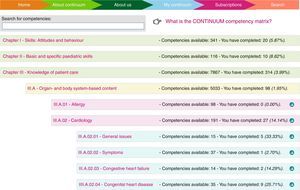
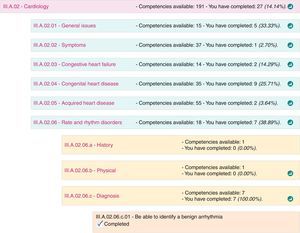
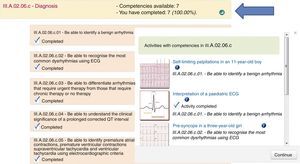
Competencies can be searched for in the matrix in 2 ways, either by expanding the various sections of which it is composed (see Figs. 1–3) or by entering the keyword in the search box (Fig. 4).
Competency matrix in Continuum (www.bit.ly/continuumcompt). Partially expanded view of the competency matrix.
Partially expanded view of the competency matrix (www.bit.ly/continuumcompt). Further expansion of competencies, showing the headings and a specific competency. Each heading has an icon on the right through which the user can access training activities in which that issue is developed in Continuum.
From a teaching point of view, the array of competencies offered by the matrix is essential for those designing and scheduling training activities, since it enables them to tailor their training programmes to the requirements. This same idea was expressed by Le Boterf, the founding father of CBE,4 when he commented that “one has to have a reference framework of the competencies required in order to identify the need for them”.
On an independent basis, as well, trainee professionals and paediatricians that consult the virtual portfolio will be able to find out what knowledge and skills they have to acquire in order to develop and improve their training.
Finally, another way in which it may be useful is by offering members of the Spanish Association of Paediatrics the option of combining the educational and professional spheres and obtaining credits for in-service training that can be presented to any institution as evidence of their professional development and periodically certify their qualification in the future.
In conclusion, the Continuum competency matrix offers the following educational opportunities and innovations:
- -
It formulates a CBE programme, underpinned by a curriculum developed and accepted by internationally recognised experts in paediatrics.
- -
It allows students to manage their own learning according to their needs.
- -
It sets out the road map that tutors and trainee paediatricians can follow to develop their training plan.
- -
It helps users to produce a personalised training portfolio, which can be used as the basis for future recertification.
The education of competent paediatricians must move forward from an exclusively curriculum-based form of training to one focusing on competencies, thus responding to the needs of the current Health System. Acquiring and maintaining professional qualification requires excellent initial training, ongoing professional development and continuous application of learning based on innovation and improvement. To achieve this, the Spanish Association of Paediatrics has made the Continuum platform available to its members, in order to attain the highest level of qualification for the whole professional community and provide the Spanish child and adolescent population with the best possible care.
Conflicts of interestCarlos Ochoa Sangrador and Carmen Villaizán Pérez are Continuum Competency Matrix coordinators; Javier González de Dios and Francisco Hijano Bandera are joint directors of Continuum.
Alberto García Salido, Nuria García Sánchez, José María Garrido Pedraz, Manuel Molina Arias, Carlos Ochoa Sangrador, Rosa Pavo García, F. Javier Pérez-Lescure Picarzo, Manuel Praena Crespo, Carmen Villaizán Pérez.
Please cite this article as: Ochoa Sangrador C, Villaizán Pérez C, González de Dios J, Hijano Bandera F, Málaga Guerrero S, coordinadores de Continuum. Continuum, la plataforma de Formación Basada en Competencias. An Pediatr (Barc). 2016;84:238.e1–238.e8.