The latest scientific literature considers early diagnosis of deafness as key element to define the educational prognosis and inclusion of the deaf child, as advantage can be taken in the critical period of development (0–4 years).
Highly significant differences exist between those deaf persons who have been stimulated early and those who have received late or inappropriate intervention.
Early identification of late-onset disorders requires special attention and knowledge of all childcare professionals. Programs and additional actions beyond neonatal screening should be designed and planned in order to ensure that every child with a significant hearing loss is detected early.
For this purpose, the Committee for the Early Detection of Deafness (CODEPEH) would like to highlight the need for continuous monitoring on the hearing health of children. And, for this reason, CODEPEH drafts the recommendations included in the present document.
La literatura científica más reciente señala el diagnóstico precoz de la sordera como elemento fundamental para definir el pronóstico educativo y de inclusión del niño sordo, pues permite aprovechar el periodo crítico de su desarrollo (0-4 años).
Existen diferencias altamente significativas entre las personas sordas estimuladas tempranamente y las que han recibido esta atención específica de forma más tardía y/o inadecuada.
La identificación temprana de los trastornos diferidos requiere de una especial atención y conocimientos entre todos los profesionales que atienden a los niños durante su infancia. Se trata de diseñar programas y de planificar acciones adicionales más allá del cribado neonatal para asegurar que todos los niños con una hipoacusia significativa sean detectados pronto.
Con este propósito, la Comisión para la Detección Precoz de la Hipoacusia (CODEPEH) quiere poner de relieve la necesidad de un seguimiento continuado sobre la salud auditiva de los niños. Y establece para ello las recomendaciones contenidas en el presente Documento.
The latest scientific literature identifies early diagnosis of deafness as the key to defining the prognosis for the education and inclusion of deaf children, as it makes it possible to take advantage of the critical period of development (the first 3 or 4 years of life). This is the age at which brain plasticity is at its highest and the child acquires certain cognitive and linguistic abilities that are difficult to recover if the opportunity to act in this period is missed.
Deafness meets all the minimum requirements for conditions suitable for screening through early detection programmes; furthermore, it has been demonstrated and recognised that treatments capable of preventing the consequences of deafness, or at least of mitigating them significantly, can be instituted at an early stage.1–3
Critical period of child developmentIn the case of deaf children it is vital to take advantage of the critical period of development, since this is when the foundations are laid for communicative development and oral language acquisition, as well as the maturation of auditory perception and of all the abilities and skills that are derived from it and affect neurological maturation processes.
There is growing scientific evidence indicating that when identification and intervention take place no later than six months of age, the child will achieve better results (by between 20 and 40 percentile points) in his or her language and communication ability: vocabulary, articulation and intelligibility of speech, social adjustment and behaviour.1,4,5
It is therefore an irretrievable period, in which the auditory information required for the brain to develop and for oral language to be comprehensively and automatically acquired needs to be available.
Only thus is it possible for deaf children to internalise phonological patterns, linguistic elements and the structure of oral language in a natural way and at an early stage, by sharing normal, spontaneous communicative interactions with their parents, using the same code, without restrictions of content or form.6–13 And consequently the risk of hearing loss having a permanent effect on the child's development, and more specifically on oral language development and the learning and communication abilities that depend on it, will be avoided.
This explains the highly significant differences between deaf children that have been stimulated early and those that have received this specific kind of attention later and/or in an inappropriate way.14
It is important to stress the crucial importance of adopting a comprehensive, holistic and coordinated approach with a defined protocol for action on deaf children and their families, taking account of all areas of development, beyond clinical issues and the provision of hearing aids.15
The experience of thousands of families in Spain underlines the fact that the time when the condition is diagnosed and the taking of immediate action on adapting to hearing aids and beginning speech-language rehabilitation are crucial in the life of a deaf person.16 Today we can say that the implications of deafness have changed substantially thanks to early intervention and advanced hearing-aid technology, normalising the educational situation of children with hearing loss and their emotional development, as well as the experience and behaviour of families.17
CODEPEH recommendationsThe CODEPEH recommendations document for 2010 recalled that the ultimate aim of all screening and early treatment of congenital hearing loss is to optimise communication and social, academic and professional development in every child with permanent hearing loss, as well as to facilitate early and natural access to oral language through hearing, taking advantage of brain plasticity in the first years of life and stimulating the child's communicative and language development.
For this reason, in line with its previous recommendations, CODEPEH wishes to emphasise the need for ongoing monitoring of the auditory health of the child population throughout its development.
Although the results confirm the value of universal neonatal screening for hearing loss, the “Achilles heel” of neonatal screening programmes is the rate of loss to followup of children with abnormal results in the tests performed at birth. We need to achieve early diagnosis of hearing loss that appears de novo in infancy in the postnatal period.
These points do not affect the intrinsic justification of universal neonatal hearing screening. On the contrary, what they imply is that we need to take additional actions and design programmes beyond neonatal screening to ensure that all children with significant hearing loss are identified early. This is why many programmes include some kind of rescreening aimed at certain children that show risk factors for late-onset or progressive hearing loss.
However, early identification of these delayed disorders requires special attention and knowledge on the part of the health services, as well as information and awareness-raising among educators, and these must be developed through education programmes and information strategies. Consideration should even be given to pre-school and school screening programmes, which have already demonstrated their usefulness.18,19
In relation to all the foregoing, this Committee considers it appropriate to establish the following recommendations for all professionals working with children in early childhood, divided into 3 spheres of action:
CODEPEH recommendations for the early detection of delayed hearing loss- –
Surveillance needs to be performed in the primary care setting following neonatal screening.
- –
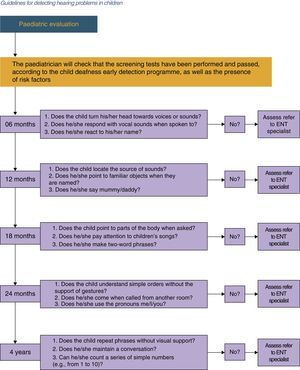
On each regular visit in the “Healthy Child” Programme the child's auditory abilities, middle-ear status and developmental milestones should be assessed. It is advisable to use the algorithm proposed by CODEPEH for application at 6, 12, 18, 24 and 48 months of age (Fig. 1).
If a child does not pass the assessment he or she should immediately be referred to an ear, nose and throat (ENT) specialist or a Children's Hearing Unit for examination.
- –
The state of the middle ear needs to be carefully examined. Children found to have serous otitis media that persists for at least 3 consecutive months must be referred for an otological assessment.
- –
Children with developmental and behavioural abnormalities should be given a hearing evaluation at least once by an ENT specialist, paying special attention in this case to relapsing or persistent serous otitis media that may worsen their prognosis.
- –
All children with a risk indicator for hearing loss (Table 1), regardless of the findings in their followup, must be referred for an audiological assessment at least once between the ages of 24 and 30 months. Children with risk indicators strongly associated with delayed-onset hearing loss, such as extracorporeal oxygenation or a cytomegalovirus (CMV) infection, should be subjected to more frequent audiological assessments.
Table 1.Risk factors for hearing loss in children.
Family suspicion of deafnessa Bacterial meningitisa Family history of deafness Syndromes with deafnessa Hypothyroidism Neurodegenerative diseasesa More than 5 days in NICU Craniofacial abnormalitiesa Exposure to ototoxic substances Extracorporeal membrane oxygenationa Assisted ventilation Severe cranial traumaa Persistent otitis Hyperbilirubinaemia with exchange transfusiona Perinatal infections (CMV, herpes, rubeola, syphilis and toxoplasmosis)a Chemotherapy - –
Confirmation of hearing loss in a child is considered a high risk factor for his or her siblings and they must be subjected to an audiological assessment.
- –
All children in whose families there is significant concern about their hearing or communication should be referred without delay to an ENT specialist or to the Children's Hearing Unit for the appropriate audiological and language assessments, regardless of their age. The same procedure should be followed if the suspicion comes from their educators.
- –
The processes of audiological diagnosis and aural rehabilitation are of equal priority and need to be pursued in the first months of life in order to maximise the child's optimum development. These 2 processes begin sequentially but must be conducted simultaneously.
- –
The follow-up intervals should be:
- -
In the first 18 months of life: continuously, as each situation demands;
- -
From 18 months to 3 years: every 3 months;
- -
From 3 to 6 years: every 6 months;
- -
Over 6 years of age with stable deafness: every year.
- -
- –
The ENT specialist must be in charge of coordinating the actions of the multidisciplinary team involved in fitting a hearing aid, together with the hearing-aid specialist and the speech therapist, and is responsible for prescribing the hearing-aid treatment.
- –
Working groups, distributed according to the structure of each autonomous community, also need to be formed for comprehensive diagnosis and treatment of children with deafness.
- –
It is essential to involve parents in the process of treating children with hearing deficit, and in order to achieve this throughout the process they must be given abundant, comprehensible and truthful information so as to create accurate expectations regarding the prognosis.
- –
The results of the brainstem auditory evoked potentials (BAEP) test should be supplemented by performing a steady-state auditory evoked potentials (SSAEP) test.
- –
The results obtained in the brainstem and steady-state auditory evoked potentials tests must be completed and confirmed using conduction audiometry appropriate to the age of the child.
- –
For tympanometry in children younger than 4 months of age it is recommended that high-frequency (1000Hz) probes should be used.
- –
The decision to fit a hearing aid should be based on the child's audiological data, language development and family, school and social environment.
- –
Until 10–12 years of age the conventional hearing aid should be behind the ear. Various types of moulds should be available so as to achieve a correct fit of the mould to the external auditory canal, especially in infants.
- –
Hearing aids with omnidirectional microphones are the most suitable for infants, who normally crawl, as they are always in the right position to receive sound.
- –
A binaural fitting should always be carried out, unless the child's behaviour suggests that the fitting in the worse ear impairs overall performance.
- –
Each case should be treated individually, since, among other reasons, there may be children in whom poor performance of the hearing aid can be explained by the presence of an auditory neuropathy or by central lesions in the auditory areas.
- –
Regulating and universalising early care, establishing 0–6 years of age as the care period.
- –
Achieving the necessary coordination between administrations and sectors to ensure joint planning of the services and assistance provided for children and their families, and also compatibility of support and services with the needs of the child and his/her background and development, and with the decisions taken by families.
- –
Providing multiple responses to diversity in care: there is no single pattern of response, and it is important to adapt to individual variability and to new developments in all areas: social, technological, legislative, etc.
- –
Updating the competencies and specialised training of professionals in the various spheres jointly involved in caring for deaf children and their families.
- –
Incorporating families into the systems that concern them regarding their deaf children and involving them at every level of intervention, leading to increased knowledge of family support among all the agents involved.
- –
Establishing easily identifiable and coordinated referral routes and care pathways for children and their families, so as to ensure the continuity of care.
- –
Fostering the participation of the family associations movement, which not only acts as a social agent and network, developing family support programmes, including mutual help groups for families, but also helps to avoid regional inequalities, provides specialised technical advice and promotes necessary change.
- –
Creating a basic common register of the results of applying the Early Detection Programme for child deafness, incorporating data from the various autonomous communities. This will be crucial for conducting epidemiological studies, adopting preventive measures, planning public healthcare and educational resources addressing the needs of the affected population and making it possible to carry out comparative studies at a national and international level, among other things.
- –
Establishing consensus on scientific, terminological, procedural, technical, educational and other issues so as to make it possible to describe and classify the needs that exist among the child population currently affected by auditory problems or at risk of having such problems.
- –
Informing and raising awareness in society and among the agents involved on the vital importance of early detection and diagnosis, monitoring and surveillance of risk factors and the need to act as quickly as possible to institute medical and hearing-aid treatment, together with early speech therapy intervention.
- –
Conducting an ongoing and rigorous assessment of services, resources, procedures and results, with quantitative and qualitative measures in all these areas, through efficacy and success indicators, with respect not only to the level of clinical intervention but also the child's progress and the satisfaction of the family and the professionals, as well as the benefits of the community.
The authors have no conflicts of interest to declare.
Please cite this article as: Núñez-Batalla F, Jáudenes-Casaubón C, Sequí-Canet JM, Vivanco-Allende A, Zubicaray-Ugarteche J. Recomendaciones CODEPEH 2014 para la detección precoz de la hipoacusia diferida. An Pediatr (Barc). 2016;85:215.e1–215.e6.
Previous presentation: This study was presented as “Recommendations CODEPEH 2014: early care and monitoring of hearing loss” at the VIII National Meeting of the Commission for the early detection of hearing loss; November 7 and 8, 2014; Las Palmas, Spain.