Burnout syndrome refers to a maladaptive response to chronic stress at work.1 It is an important problem in the health care field that has negative consequences for the professionals that suffer from it and for the patients, who are considered the secondary victims of burnout.1,2
Health care professionals employed in intensive care units and emergency departments are a collective that is particularly at risk of suffering burnout syndrome due to the specific characteristics of these settings (such as high caseloads, insufficient staff, rotating shift schedules).1–3 In Spain, no studies have been conducted to analyse this subject in the paediatric emergency department (PED) setting, and therefore the prevalence of burnout in these departments is unknown.
Thus, we conducted a study with the following objectives: 1) to determine the prevalence of burnout syndrome in paediatricians staffing PEDs in Catalonia, and 2) to investigate risk factors for burnout.
We designed a multicentre descriptive study that involved collection of data by means of a questionnaire. In September 2018, se emailed the heads of the PEDs of 21 Catalan hospitals requesting participation of the emergency department staff in the study. The study included physicians (adjunct physicians and residents in training) and nursing staff (nurses and nursing assistants).
Those respondents that consented to participate completed the questionnaire anonymously (through an online GoogleDocs® form). We collected the following information through the questionnaire:
Personal characteristics: sex, age, professional category.
Professional characteristics: years worked in emergency department, work schedule in the PED (full time, part time or only on-call shifts), hours worked each week, shift structure, type of activity (exclusively clinical versus mixed activity). We defined mixed activity as participation in other type of activity such as administration, research and/or teaching.
Answers to the Maslach Burnout Inventory adapted to the Spanish population4: the questionnaire comprises 22 items in 3 scales that address different dimensions of burnout, emotional exhaustion (9 items), depersonalization (5 items) and personal accomplishment (8 items). Based on the score obtained, each scale can be categorised in 3 levels (low, medium and high). We defined burnout in health care professionals as high emotional exhaustion, high depersonalization and low personal accomplishment. We defined absence of burnout as low emotional exhaustion, low depersonalization and high personal accomplishment.
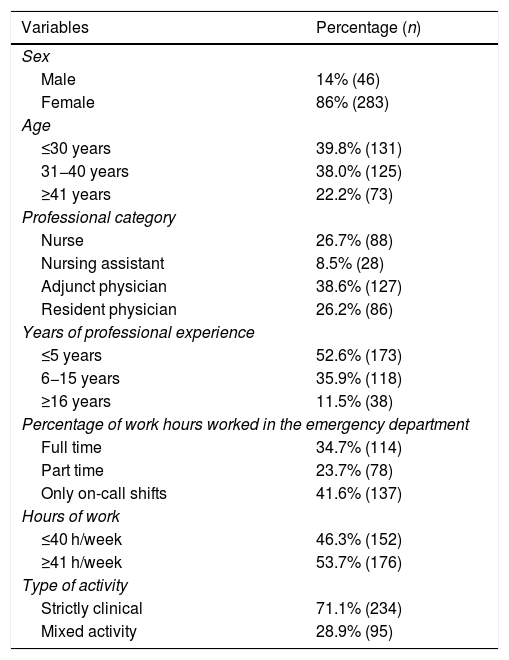
We received 329 questionnaires from 18 hospitals. The median age of respondents was 33 years (interquartile range, 28–40). Table 1 summarises the personal and professional characteristics of respondents. Of all respondents, 71.1% worked exclusively in care delivery (34.6% in emergency care only, the rest in a combination of settings); 40.1% also engaged in some form of nonclinical work (teaching in 56.1%, research in 25.7% and administrative tasks in 18.2% of cases).
Personal and professional characteristics of participants in the study (N = 329).
| Variables | Percentage (n) |
|---|---|
| Sex | |
| Male | 14% (46) |
| Female | 86% (283) |
| Age | |
| ≤30 years | 39.8% (131) |
| 31−40 years | 38.0% (125) |
| ≥41 years | 22.2% (73) |
| Professional category | |
| Nurse | 26.7% (88) |
| Nursing assistant | 8.5% (28) |
| Adjunct physician | 38.6% (127) |
| Resident physician | 26.2% (86) |
| Years of professional experience | |
| ≤5 years | 52.6% (173) |
| 6−15 years | 35.9% (118) |
| ≥16 years | 11.5% (38) |
| Percentage of work hours worked in the emergency department | |
| Full time | 34.7% (114) |
| Part time | 23.7% (78) |
| Only on-call shifts | 41.6% (137) |
| Hours of work | |
| ≤40 h/week | 46.3% (152) |
| ≥41 h/week | 53.7% (176) |
| Type of activity | |
| Strictly clinical | 71.1% (234) |
| Mixed activity | 28.9% (95) |
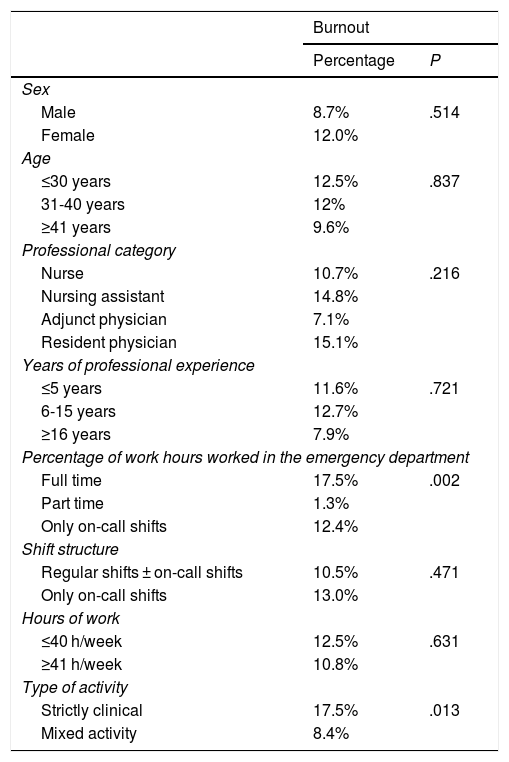
Thirty-eight participants met the criteria for burnout, corresponding to a prevalence of burnout syndrome of 11.6% (95% CI, 8.5–15.5). We found that 33.1% (109 participants) had a high level of emotional exhaustion, 6.4% (21 participants) a high level of depersonalization, and 27,4% (90 participants) a low level of personal accomplishment. On the other hand, 10.9% (36 participants) did not have a significant score in any of the 3 scales. Table 2 presents the distribution of burnout based on different variables under study.
Percentage of professionals with and without burnout in the different groups under study. The percentage distribution of professionals meeting the criteria for burnout is given for each of the variables under study.
| Burnout | ||
|---|---|---|
| Percentage | P | |
| Sex | ||
| Male | 8.7% | .514 |
| Female | 12.0% | |
| Age | ||
| ≤30 years | 12.5% | .837 |
| 31-40 years | 12% | |
| ≥41 years | 9.6% | |
| Professional category | ||
| Nurse | 10.7% | .216 |
| Nursing assistant | 14.8% | |
| Adjunct physician | 7.1% | |
| Resident physician | 15.1% | |
| Years of professional experience | ||
| ≤5 years | 11.6% | .721 |
| 6-15 years | 12.7% | |
| ≥16 years | 7.9% | |
| Percentage of work hours worked in the emergency department | ||
| Full time | 17.5% | .002 |
| Part time | 1.3% | |
| Only on-call shifts | 12.4% | |
| Shift structure | ||
| Regular shifts ± on-call shifts | 10.5% | .471 |
| Only on-call shifts | 13.0% | |
| Hours of work | ||
| ≤40 h/week | 12.5% | .631 |
| ≥41 h/week | 10.8% | |
| Type of activity | ||
| Strictly clinical | 17.5% | .013 |
| Mixed activity | 8.4% | |
Chi square and Fisher exact test.
Statistical significance defined as P < .05.
The prevalence of burnout in the care staff of Catalonian PEDs included in the study was high: approximately 1 in 10 health care workers met the criteria for burnout and more than 2/3 had an abnormal result in at least one scale (most frequently a high level of emotional exhaustion). In the field of paediatrics, the prevalence of burnout is lower compared to adult care, approximately ranging from 35% to 40% of paediatricians3 and 25% of paediatric emergency physicians.5 The low prevalence found in our study may be explained by different factors: on one hand, our sample was younger compared to other studies, and on the other we defined burnout as an altered score in all three scales (other authors considered an altered score in any scale sufficient to consider the syndrome to be present).1,5,6
The risk factors for developing burnout syndrome are working full time in the emergency department and having an exclusively clinical role. Protective factors described in the previous literature (that were not assessed in our study) were continuing education of health care professionals, work-life balance, teamwork and specific personality traits.2,6
Lastly, some authors have suggested that burnout should be perceived as a manifestation of a dysfunctional health care system, and that measures should be taken at the individual and collective level. Given the current professional trend of exclusive, specialised dedication to emergency care, protective strategies must be developed to prevent job burnout: strategies aimed at improving care pathways, reducing the burden of bureaucratic tasks, avoiding long work days and facilitating the wellbeing, work-life balance and personal development of emergency care staff.2,3,5,6
We thank the administrators and health care staff that have participated in the study from the following hospitals: Carles Luaces Cubells (Hospital Sant Joan de Déu), Sebastián González Peris (Hospital Universitari Vall d’Hebron), Neus Pociello (Hospital Universitari Arnau in Vilanova de Lleida), Eva Botifoll García (Hospital Sant Joan de Déu in Manresa), Abel Marínez Mejías (Consorci Sanitari of Terrassa), Toni de Francisco (Hospital Universitari Germans Trias i Pujol), Xavier Codina Puig (Hospital General de Granollers), Sandra Moya Villanueva (Hospital Parc Taulí of Sabadell), Ester Castellarnau Figueras (Hospital Universitari de Tarragona Joan XXIII), Montse Gispert-Saüch (Hospital Universitari Doctor Josep Trueta), Elisabet Coca Fernández (Hospital de la Santa Creu i Sant Pau), Fernando David Panzino (Hospital General del Parc Sanitari Sant Joan de Déu), Matilde Viñas Viña (Hospital Universitari Dexeus), Amaia Bilbao Garitagoitia (Parc de Salut Mar), Pablo Ercoli (Fundació Sant Hospital La Seu d’Urgell), Hospital de Santa Caterina and Clínica Sant Josep.
Please cite this article as: Parra Cotanda C, de la Maza VTS, Luaces Cubells C. Burnout en los pediatras de urgencias. An Pediatr (Barc). 2020;93:200–202.
Previous presentations: this study was presented as an oral communication at the XXIV Annual Meeting of the Sociedad Española de Urgencias de Pediatría; May 9–11, 2019; Murcia, Spain.