Bronchiolitis poses a considerable challenge during its seasonal peak, overwhelming the material and human resources available to care for affected patients. As a result, interhospital transfers increase exponentially. We did not find any studies analysing the characteristics of patients with bronchiolitis managed in out-of-hospital urgent care (OHUC) services and the impact of the COVID-19 pandemic on the epidemiology of bronchiolitis.
ObjectiveTo establish the characteristics of paediatric and neonatal patients with acute bronchiolitis (AB) managed in OHUC services in the Community of Madrid and to analyse the impact of the COVID-19 pandemic on the epidemiology of bronchiolitis.
MethodsRetrospective cross-sectional observational and descriptive study carried out in OHUC settings in the Community of Madrid between 2016 and 2023. We included patients with a diagnosis of acute bronchiolitis based on the ICD-10 codes documented in the electronic records of urgent care visits and interhospital transports. We collected data on sociodemographic, clinical and treatment (ventilation and medication) variables.
ResultsThe sample included 630 patients with AB: 343 managed in non-neonatal OHUC (non-neo) services and 287 by the mobile neonatal intensive care unit transport team (NTT). The median age was 3.7 months (IQR, 2.8–4.7) in patients in the non-neo OHUC group and 19 days (IQR, 14.2−23.7) in the NTT group. There was a statistically significant increase in age in the 2020/2021 season in the non-neo OHUC group. The severity score was significantly higher in the NTT group. There was an unusual peak in bronchiolitis cases in June 2021, coinciding with the end of the 4th wave of the COVID-19 pandemic. The incidence of bronchiolitis was highest after the 6th wave of the pandemic (13.5 cases per 10 000 children aged < 2 years).
ConclusionsThe median age of paediatric patients with AB managed in OHUC services increased following the end of the lockdown imposed due to the COVID-19 pandemic, which was probably associated with the lack of exposure to the viruses that cause it. This also may explain why the incidence of bronchiolitis was highest in the season following the 6th wave of the pandemic. The severity score was higher in neonatal patients. Epidemiological surveillance, the introduction of protocols and the implementation of an ongoing training programme for non-specialized health care staff involved in the transport of these patients could improve their management.
La bronquiolitis se convierte en todo un reto durante su pico estacional, desbordando los recursos materiales y humanos para poder atender los pacientes afectados. A consecuencia de ello, se multiplican exponencialmente los traslados interhospitalarios. No se han encontrado estudios que hayan analizado las características de los pacientes con bronquiolitis aguda (BA) en los Servicios de Urgencias Extrahospitalarios (SUEH) y la influencia de la pandemia en su epidemiología.
ObjetivoConocer las características de los pacientes pediátricos y neonatales con bronquiolitis en los SUEH de la Comunidad de Madrid y analizar la influencia de la pandemia COVID-19 en su epidemiología.
Material y métodosEstudio observacional descriptivo, transversal y retrospectivo realizado en los SUEH de la Comunidad de Madrid entre 2016–2023. Se incluyeron pacientes con diagnóstico de BA según CIE-10 en la Historias Clínicas de las asistencias y traslados interhospitalarios. Se registraron variables sociodemográficas, clínicas y de tratamiento (ventilatorio y farmacológico).
ResultadosSe incluyeron 630 pacientes con BA: 343 atendidos por los SUEH no especializados en neonatología (no-neo) y 287 por el equipo de transporte neonatal (TN). La mediana de edad fue de 3,7 meses [2,8–4,7] en SUEH no-neo y de 19 días [14,2–23,7] en TN. Hubo un aumento de la edad estadísticamente significativa en la temporada 2020/2021 en el grupo de SUEH no-neo. La escala de gravedad fue estadísticamente mayor en el grupo de TN. Hubo un pico inusual de casos de bronquiolitis en junio de 2021 coincidiendo con el fin de la 4ª ola de COVID-19. La incidencia de bronquiolitis, tras la 6ª ola de pandemia, fue la mayor de todas las temporadas (13,5 casos por cada 10.000 niños ≤ 2 años).
ConclusionesLa mediana de edad en los pacientes pediátricos con bronquiolitis aguda en los SUEH aumentó tras finalizar el confinamiento de la pandemia COVID-19, en probable relación con la ausencia de exposición a los virus causantes de la misma. Esto podría explicar también que la incidencia de bronquiolitis tras la 6ª ola de pandemia fue la mayor de todas las temporadas. La escala de gravedad fue mayor en los pacientes neonatales. La vigilancia epidemiológica, implantación de protocolos e implementación de un programa de formación continuada a los profesionales no especializados encargados de los traslados de este tipo de pacientes podría mejorar su manejo.
Out-of-hospital urgent care (OHUC) services, like in-hospital emergency services, require up-to-date knowledge and skills. Specifically, training on the management of critically ill children is particularly important in OHUC delivery. In particular, acute bronchiolitis (AB) becomes a significant challenge during the seasonal peak, overwhelming human and material resources. In addition to an increase in home visits due to this condition, the frequency of interhospital transport grows exponentially. Such transports involve the transfer of patients from sending hospitals without a paediatric intensive care unit (PICU) to hospitals offering higher levels of care. The OHUC teams of the Community of Madrid provide the following services: (1) primary care: management of the patient at home or in the community, and (2) interhospital transport. Primary care can be delivered through a mobile medical unit (MMU), in the case of non-emergency conditions, or by a mobile intensive care unit (MICU) if the patient requires emergency care. Interhospital transports, depending on the condition and age of the patient, can be carried out in a basic life support ambulance, MICU or by a specialised neonatal transport team (NTT) that, in turn, comprises 2 units: (1) an advanced life support (ALS) team composed of two emergency medical technicians (EMTs) and an OHUC nurse and (2) a unit composed by a neonatologist (routinely involved in the delivery of level III neonatal care and trained in neonatal transport) and one OHUC EMT with specific training in neonatal care.
Thus, primary care is provided by OHUC teams not specialised in neonatology (non-neonatal OHUC) and interhospital transport carried out non-neonatal OHUC teams (patients aged ≥ 29 days) or the NTT (patients aged ≤ 28 days and/or < 44 weeks of postmenstrual age).
Out-of-hospital urgent care settings exclude outpatient urgent health care facilities (hospitals and primary care centres), and only include mobile care teams/ambulances.
During the COVID-19 pandemic, there was a shift in the epidemiology of bronchiolitis, with a sharp drop in the frequency of paediatric hospital admissions for this cause,1–4 with no evidence of increased severity in children with coinfection.4 Most hospital-based studies4–6 compared the characteristics of the patients and their respiratory infections before and during the COVID-19 pandemic. However, despite the abundance of evidence on the impact of the pandemic on the hospital setting, little is known about its impact on OHUC. It would also be interesting to know the impact of the COVID-19 pandemic on the epidemiology of AB, the patient characteristics and neonatal and paediatric transport at the OHUC level. All this information could help organise and manage resources more efficiently during epidemics, in addition to the establishment of effective preventive strategies to control outbreaks.
Thus, the aim of our study was to establish the incidence of bronchiolitis in the different periods between 2016 and 2023 and the main characteristics of neonatal and paediatric patients transported by the OHUC teams of the Community of Madrid, in addition to assessing whether the COVID-19 pandemic has changed epidemiological trends and the characteristics of patients with bronchiolitis.
Material and methodsStudy designWe conducted a cross-sectional, retrospective observational and descriptive study in the OHUC teams of the Community of Madrid (Spain) covering the period between 2016 and 2023.
Study sample and data collectionWe included every patient with a diagnosis of bronchiolitis based on the International Classification of Diseases 10th Revision (ICD-10) code aged less than 24 months who had received home care or transported between hospitals between years 2016 and 2023 (both included).
We collected data through the electronic health record (EHR) database, facilitated by the information and technology support team and NTT of the OHUC system of the Community of Madrid.
The 2016–2023 period included 7 bronchiolitis seasons. The seasons were defined as spanning from September through August of the following year (both included), in accordance with the general consensus of the medical literature.
We took into account the six waves of the COVID-19 considering the cumulative incidence in 14 days in Spain from March 2020 to March 20227 to assess the potential impact of the pandemic on the epidemiology of bronchiolitis. We obtained these data from the notification of COVID-19 cases to the National Epidemiological Surveillance Network (RENAVE) through the online platform SiViES (Sistema de Vigilancia de España, Spanish Surveillance System) managed by the Centro Nacional de Epidemiología (CNE, National Centre of Epidemiology). This information was obtained through the epidemiological questionnaire that each autonomous community completed once a COVID-19 case was identified. The recorded starts of the 6 waves correspond to April 2020 (1st), September 2020 (2nd), January 2021 (3rd), April 2021 (4th), July 2021 (5th) and January 2022 (6th).
We obtained the size of the population used to estimate incidence values from official municipal population census data as of January 1 published by the Instituto Nacional de Estadística (INE, National Institute of Statistics) of Spain8 for each year under study.
The last season, corresponding to 2022/2023, could not be included in the descriptive analysis due to missing data for many variables, as the EHR databases update their statistical data once the year has come to an end.
We made a descriptive analysis of two groups of patients: (1) those managed by the NTT and (2) those managed by OHUC teams not specialised in neonatal care (non-neonatal OHUC).
Study variablesWe collected data for 21 variables classified as: (1) general characteristics of the patient: age, sex and preterm birth (gestational age < 37 weeks); (2) health care team that managed the patient: MMU, MICU or NTT; (3) clinical condition of the patient at the beginning of the care episode: oxygen saturation (SatO2), chest wall retractions, vital signs for patient age (tachypnoea, tachycardia, hypotension) and modified Tal severity score9; (4) respiratory support: conventional oxygen therapy, high-flow oxygen therapy (HFOT) delivered with nasal prongs, non-invasive mechanical ventilation (NIMV) and invasive mechanical ventilation (IMV), and (5) pharmacological treatment: sedation (midazolam, morphine hydrochloride or fentanyl), salbutamol and budesonide.
We chose the modified Tal score because, out of the available validated bronchiolitis severity scores,10 it is the most suitable for the out-of-hospital setting.
Statistical analysisFirst, we conducted a descriptive analysis, expressing qualitative data as absolute frequencies and percentages and quantitative data as median and interquartile range (IQR). We compared qualitative or categorical variables with the Pearson χ2 test and quantitative variables with the Student t-test (comparison of 2 variables) or analysis of variance (ANOVA) (comparison of 3 or more variables) if they followed a normal distribution, and otherwise with the Mann–Whitney U test (2 variables) or the Mood median test (3 or more variables). For categorical independent variables, we used the χ2 test of independence, grouping categories with expected values of less than 5 together and obtaining a single P value for the whole. We fitted different linear regression models to assess the main independent factors that could be associated with or have an effect on the modified Tal severity score.
To estimate the incidence of bronchiolitis in the population, we used the data for the paediatric population aged 24 months or less provided by the INE,8 establishing the month of January as the cut-off point. We calculated the estimated incidence using the number of cases of bronchiolitis per year per 10 000 inhabitants ≤ 2 years, to facilitate comparisons with other studies
The statistical analysis was carried out with the STATA software (Statistical software for data science [https://www.stata.com]), version 17.0.
Ethical considerationsThe study adhered to the principles of the Declaration of Helsinki and was approved by the regional ethics committee of the Community of Madrid. Since the data were anonymised end encrypted upon retrieval from the EHR database, signed informed consent by the parents or legal guardians of the patients was not required.
ResultsGeneral characteristicsThe study included 630 patients with bronchiolitis managed between September 2016 and August 2023: 343 (54.4%) were managed by non-neonatal OHUC teams and 287 (45.6%) by the NTT. Tables 1 and 2 present the general characteristics of each of the groups by season. In the non-neonatal OHUC group (Table 1) the median age in the 2020/2021 season was significantly greater compared to all other seasons (6.9 months [5.4−8.4]). The use of salbutamol was also less prevalent in the last two seasons compared to the rest. In the NTT group (Table 2), we found statistically significant differences in: lower frequency of preterm birth in the last two seasons compared to the rest (2 [7.1%]); a lower frequency of tachycardia (34 [63.0%]) and continuous positive airway pressure (CPAP) (10 [18.5%]) in the 2019/2020 season compared to the rest, as opposed to IMV, the use of which was more frequent in the 2017/18 season (8 [12.7%]). In the 2016/2017 and 2020/2021 seasons, the use of salbutamol decreased (0 [0.0%]) compared to all other seasons.
Descriptive analysis of patients with bronchiolitis managed by non-neonatal OHUC teams.
| Season | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21 | 2021/22 | P |
|---|---|---|---|---|---|---|---|
| n | 69 | 74 | 56 | 66 | 37 | 41 | |
| Epidemiological data | |||||||
| Age (months), median [IQR] | 3.6 [2.8−4.4] | 3.9 [3.2−4.6] | 1.3 [0.9−1.7] | 4.9 [3.1−6.7] | 6.9 [5.4−8.4] | 3.2 [2.4−4.0] | 0.02 |
| Female sex, n (%) | 31 (44.9%) | 40 (54.1%) | 38 (67.9%) | 43 (65.2%) | 22 (59.5%) | 22 (53.7%) | 0.37 |
| Clinical presentation | |||||||
| Tachypnoea, n (%) | 40 (58.8%) | 41 (56.2%) | 35 (62.5%) | 38 (57.6%) | 22 (59.5%) | 20 (48.8%) | 0.73 |
| Tachycardia, n (%) | 44 (64.7%) | 47 (64.4%) | 38 (67.9%) | 38 (57.6%) | 24 (64.9%) | 21 (51.2%) | 0.72 |
| Chest retractions, n (%) | 11 (15.9%) | 27 (36.5%) | 20 (35.7%) | 24 (36.4%) | 13 (35.1%) | 10 (24.4%) | 0.05 |
| Modified Tal severity score | 0.9 | ||||||
| Mild, n (%) | 46 (67.6%) | 46 (63.0%) | 37 (66.1%) | 42 (63.6%) | 24 (64.9%) | 28 (68.3%) | |
| Moderate, n (%) | 18 (26.5%) | 21 (28.8%) | 16 (28.6%) | 17 (25.8%) | 9 (24.3%) | 10 (24.4%) | |
| Severe, n (%) | 4 (5.9%) | 6 (8.2%) | 3 (5.4%) | 7 (10.6%) | 4 (10.8%) | 3 (7.3%) | |
| Respiratory support | |||||||
| Oxygen therapy, n (%) | 32 (46.3%) | 37 (50%) | 29 (52.7%) | 25 (4.9%) | 11 (2.7%) | 13 (31.8%) | 0.5 |
| High-flow oxygen, n (%) | 0 (0.0%) | 0 (0.0%) | 1 (1.8%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.4 |
| NIMV-CPAP, n (%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (2.4%) | 0.2 |
| NIMV-BiPAP, n (%) | 1 (1.4%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 1 (2.4%) | 0.45 |
| IMV, n (%) | 3 (4.3%) | 2 (2.7%) | 2 (3.6%) | 6 (9.1%) | 4 (10.8%) | 3 (7.3%) | 0.39 |
| Pharmacotherapy | |||||||
| Salbutamol, n (%) | 12 (17.4%) | 21 (28.4%) | 11 (19.6%) | 10 (15.2%) | 3 (8.1%) | 3 (7.3%) | 0.03 |
| Sedation (midazolam or opiates), n (%) | 3 (4.3%) | 2 (2.7%) | 2 (3.6%) | 8 (12.1%) | 5 (13.5%) | 4 (9.8%) | 0.7 |
BiPAP, bilevel positive airway pressure; CPAP, continuous positive airway pressure; IQR, interquartile range; IMV, invasive mechanical ventilation; NIMV, non-invasive mechanical ventilation; OHUC, out-of-hospital urgent care.
Results that are statistically significant compared to all other seasons are presented in boldface.
Descriptive analysis of patients with bronchiolitis managed by the specialised neonatal transport team.
| Season | 2016/17 | 2017/18 | 2018/19 | 2019/20 | 2020/21 | 2021/22 | P |
|---|---|---|---|---|---|---|---|
| n | 49 | 63 | 65 | 54 | 28 | 28 | |
| Epidemiological data | |||||||
| Age (months), median [IQR] | 24 [19−29] | 18 [14.5−21.5] | 24 [20.7−27.3] | 18 [15.2−20.8] | 20 [16.2−23.8] | 18 [15.2−21.8] | 0.48 |
| Female sex, n (%) | 22 (44.9%) | 34 (54.0%) | 32 (49.2%) | 21 (38.9%) | 13 (46.4%) | 12 (42.9%) | 0.6 |
| Preterm birth, n (%) | 13 (26.5%) | 18 (28.5%) | 8 (12.3%) | 14 (25.9%) | 2 (7.1%) | 2 (7.1%) | 0.03 |
| Clinical presentation | |||||||
| Tachypnoea, n (%) | 43 (87.8%) | 56 (90.3%) | 57 (87.7%) | 46 (85.2%) | 28 (100.0%) | 27 (96.4%) | 0.41 |
| Tachycardia, n (%) | 42 (85.7%) | 55 (88.7%) | 54 (83.1%) | 34 (63.0%) | 28 (100.0%) | 27 (96.4%) | <0.001 |
| Chest retractions, n (%) | 41 (85.4%) | 45 (71.4%) | 44 (67.7%) | 40 (74.1%) | 26 (92.9%) | 21 (75.0%) | 0.7 |
| Modified Tal severity score | 0.9 | ||||||
| Mild, n (%) | 8 (16.3%) | 10 (16.1%) | 7 (10.8%) | 8 (14.8%) | 4 (14.3%) | 5 (17.9%) | |
| Moderate, n (%) | 17 (34.7%) | 34 (54.8%) | 44 (67.7%) | 34 (63.0%) | 14 (50.0%) | 15 (53.6%) | |
| Severe, n (%) | 24 (49.0%) | 18 (29.0%) | 14 (21.5%) | 12 (22.2%) | 10 (35.7%) | 8 (28.6%) | |
| Respiratory support | |||||||
| Oxygen therapy, n (%) | 9 (18.4%) | 12 (19.0%) | 8 (12.3%) | 11 (20.4%) | 5 (17.9%) | 5 (17.9%) | 0.12 |
| High-flow oxygen, n (%) | 0 (0.0%) | 0 (0.0%) | 5 (7.7%) | 1 (1.9%) | 1 (3.6%) | 1 (3.6%) | 0.9 |
| NIMV-CPAP, n (%) | 26 (53.1%) | 25 (39.7%) | 17 (26.2%) | 10 (18.5%) | 14 (50.0%) | 8 (28.6%) | 0.001 |
| NIMV-BiPAP, n (%) | 10 (20.5%) | 16 (65.1%) | 33 (25.4%) | 34 (63.0%) | 8 (28.6%) | 13 (46.4%) | 0.5 |
| IMV, n (%) | 1 (2.0%) | 8 (12.7%) | 1 (1.5%) | 0 (0.0%) | 1 (3.6%) | 0 (0.0%) | 0.003 |
| Pharmacotherapy | |||||||
| Salbutamol, n (%) | 0 (0.0%) | 8 (12.7%) | 3 (4.6%) | 4 (7.4%) | 0 (0.0%) | 1 (3.6%) | 0.04 |
| Sedation (midazolam or opiates), n (%) | 1 (2.0%) | 1 (1.6%) | 3 (4.6%) | 4 (7.4%) | 1 (3.6%) | 0 (0.0%) | 0.3 |
BiPAP, bilevel positive airway pressure; CPAP, continuous positive airway pressure; IQR, interquartile range; IMV, invasive mechanical ventilation; NIMV, non-invasive mechanical ventilation; OHUC, out-of-hospital urgent care.
Results that are statistically significant compared to all other seasons are presented in boldface.
Table 3 compares the characteristics of patients in the NTT and the non-neonatal OHUC groups, showing that in the NTT group, the age was lower (19 days [14.2−23.7]), and the frequency of tachypnoea (257 [89.9%]), tachycardia (240 [83.9%]) and chest retractions (217 [75.9%]) was higher compared to the non-neonatal OHUC group. The use of high-flow oxygen therapy (8 [2.8%]), CPAP (100 ([34.8%]) and bilevel positive airway pressure (BiPAP) (114 [39.7%]) was greater in the non-neonatal OHUC group, while conventional oxygen therapy was less frequent (50 [17.4%]). We found no differences in the use of IMV between groups. We also found a less frequent use of salbutamol in the NTT group (16 [5.6%]).
Comparative analysis of non-neonatal OHUC teams and the specialised neonatal transport team.
| Type of care team | Non-neonatal OHUC | NTT | P |
|---|---|---|---|
| n | 343 | 287 | |
| Epidemiological data | |||
| Age (months), median [IQR] | 112.5 [84.5−140.5] | 19 [14.2−23.7] | <0.001 |
| Female sex, n (%) | 196 (57.1%) | 134 (46.6%) | 0.16 |
| Clinical presentation | |||
| Tachypnoea, n (%) | 196 (57.5%) | 257 (89.9%) | <0.001 |
| Tachycardia, n (%) | 212 (62.2%) | 240 (83.9%) | <0.001 |
| Chest retractions, n (%) | 105 (30.6%) | 217 (75.9%) | <0.001 |
| Modified Tal severity score | <0.001 | ||
| Mild, n (%) | 223 (65.4%) | 42 (14.7%) | |
| Moderate, n (%) | 91 (26.7%) | 158 (55.2%) | |
| Severe, n (%) | 27 (7.9%) | 86 (30.1%) | |
| Respiratory support | |||
| Oxygen therapy, n (%) | 147 (43%) | 50(17.4%) | <0.001 |
| High-flow oxygen, n (%) | 1 (0.3%) | 8 (2.8%) | 0.009 |
| NIMV-CPAP, n (%) | 1 (0.3%) | 100 (34.8%) | <0.001 |
| NIMV-BiPAP, n (%) | 2 (0.6%) | 114 (39.7%) | <0.001 |
| IMV, n (%) | 20 (5.8%) | 11 (3.8%) | 0.25 |
| Pharmacotherapy | |||
| Salbutamol, n (%) | 60 (17.5%) | 16 (5.6%) | <0.001 |
| Sedation, n (%) | 24 (6.9%) | 10 (3.4%) | <0.001 |
BiPAP, bilevel positive airway pressure; CPAP, continuous positive airway pressure; IQR, interquartile range; IMV, invasive mechanical ventilation; NIMV, non-invasive mechanical ventilation; NTT, neonatal transport team; OHUC, out-of-hospital urgent care.
Results that are statistically significant compared to all other seasons are presented in boldface.
Based on the severity scores, the frequency of mild cases was greater and the frequency of moderate and severe cases lower among the patients managed by OHUC teams compared to the NTT.
Association with the severity scoreIn order to identify independent variables associated with the severity score, we fitted linear regression models. Neither age, sex nor preterm birth were associated with the severity score (correlation coefficients < 0.01 with P values > 0.05 and an R2 of 1.1% in the regression model).
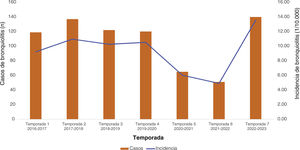
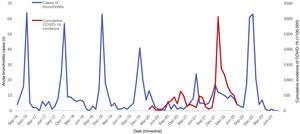
Incidence analysisFig. 1 presents the incidence of AB by season in the 2016–2023 period. The season with the lowest incidence corresponded to 2021/2022, with 4.9 cases per 10 000 children under 2 years. The season with the highest incidence corresponded to 2021/2022, with 13.5 cases per 10 000 children under 2 years.
Fig. 2 presents the number of cases of AB per month in relation to the incidence of COVID-19, showing the 6 main waves of the COVID-19 pandemic, with evidence of an increase in cases after the 6th wave in January 2022, which was also greater compared to all other seasons. It also shows an increase in the cases of bronchiolitis in June 2021 that did not take place in previous seasons, coinciding with the end of the 4th wave of the pandemic.
DiscussionMultiple studies conducted in the hospital setting have evinced changes in the epidemiology of AB,1–3,11–14 with a nearly negligible incidence in the 2020/2021 season followed by a progressive increase. Although the settings differed, these trends are consistent with the data analysed in our study, which showed a drastic decrease in the incidence of AB during the COVID-19 pandemic, followed by a recovery after the 6th wave, when it increased beyond the incidence of all other seasons under study.
Another interesting phenomenon observed after the pandemic in other countries, like Italy4 or France,14 was the delay in the peak of hospital admissions due to bronchiolitis, also reported in Spain in regions like Andalusia,15 where, in the post-pandemic period, hospital admissions peaked in the summer months, whereas before the COVID-19 pandemic this peak took place in January-February. Our findings were similar, with an unusual surge of cases in June 2021 following the 4th wave of the COVID-19 pandemic.
As for age, after the COVID-19 pandemic, the median age was 18 days in the NTT group and 3.2 months in the non-neonatal OHUC group. Comparing this with other studies, and despite the differences in care setting, the median age observed in the non-neonatal OHUC group was similar to the one reported by Loconsole et al.4 (4 months) and Guitart et al.6 (2 months).
In the non-neonatal OHUC group, the median age increased in the 2020/2021 season, which could be explained by the home confinement measures implemented at the beginning of the pandemic. Since children had not developed immunity against respiratory viruses due to the lockdown, those who would have already had bronchiolitis presented this type of infection once they were exposed to the viruses again, which was later than usual.
Although the percentage of severe cases was greater in the NTT group, our study did not find an association between age or preterm birth and severity, which has been described in previous studies, for instance, by Guitart et al.,6 who found an association between disease severity and preterm birth.
The severity score was higher in the group of neonatal patients transported by the NTT, however, there was a smaller proportion of patients managed with IMV compared to the non-neonatal OHUC group. This can be explained by the fact that OHUC teams chiefly provide primary care, and that, if the patient becomes unstable at home or during transport, these teams do not have the capacity to deliver NIMV to children with weights of less than 5 kg, and thus need to step up to IMV directly. On the other hand, interhospital transports carried out by the NTT sometimes involve tertiary care hospitals with limitations for the delivery of NIMV, leading to the maintenance of HFOT in severe patients. Stabilization with NIMV upon arrival of the NTT would allow improving the clinical condition of the patient without requiring IMV. To this, we must add the experience in the delivery of this modalities of respiratory support and in managing this type of patient of neonatal and paediatric transport teams. This highlights the importance of allocating the necessary material resources to OHUC teams and especially of the training in the management of this type of patients and of diseases.
As regards the use of salbutamol in the non-neonatal OHUC group, it decreased significantly in the last few seasons, but still was used in a percentage that needs to be taken into account. Improved training on the diagnosis of bronchiolitis after the pandemic, including DO NOT DO recommendations, and the frequent use of salbutamol for the bronchial challenge test in out-of-hospital settings in children aged more than 6 months would explain the pattern of use in the last few seasons.
At present, there is no effective pharmacological treatment for AB. The meta-analyses that have analysed the currently used treatment options, like salbutamol, budesonide, adrenaline, hypertonic saline solution, corticosteroids or antibiotics have not found evidence supporting their use.16 As a result, clinical practice guidelines11,17 discourage these treatments. This evinces the importance of developing management protocols for these patients and providing regular training to avoid the use of unnecessary drugs, as has been done in other care settings.16 Such protocols would also help optimise the use of resources during seasonal outbreaks.
In conclusion, based on the reported findings, the following would be important measures to implement in the future: (1) epidemiological surveillance to anticipate surges in health care demand by this type of patients and to improve resource management in each seasonal campaign, optimization of health care and use of preventive measures, such as hand hygiene, face masks and social distancing, and (2) development of training and management protocols for OHUC teams, training professionals to optimise and streamline care delivery in both interhospital transport and primary care interventions. Efforts in these areas would not only have an economic impact through a significant reduction in costs, but could also improve long-term respiratory outcomes in paediatric patients.
Limitations of the studyDue to the retrospective design, we cannot rule out the possibility of undetected confounding factors not accounted for in the analysis that may have biased the results. The continuity of this study through time will provide the opportunity to corroborate the observed trends.
The fact that neither age nor preterm birth appeared to be associated with severity could be explained by two facts: (1) the low frequency of preterm neonate transport, since it was only analysed within the NTT group, and (2) due to the few independent variables that could be added to the model, like comorbidity, birth weight, foetal distress… this would explain the low R2 values and power (1.1%). It would be interesting to conduct a study in the future with the addition of more independent variables in the model that could evince a greater strength in the association.
ConclusionThe median age of paediatric patients with AB managed by OHUC teams in the Community of Madrid increased temporarily following the end of the lockdown imposed due to the COVID-19 pandemic, which was probably associated with the lack of exposure to the viruses that cause it. This also may explain why the incidence of bronchiolitis was highest in the season following the sixth wave of the pandemic.
The severity score was higher in neonatal patients. Epidemiological surveillance, the introduction of protocols and the implementation of an ongoing training programme for non-specialized health care staff involved in the transport of these patients could improve their management.
FundingFundación para la Investigación e Innovación Biomédica de Atención Primaria (FIIBAP, Foundation for Primary Care Research and Biomedical Innovation).
Conflicts of interestThe authors have no conflicts of interest to disclose in relation to the study, of which there are no redundant or duplicated publications.
We thank Juan Pajuelo Ayuso, José Gómez Martínez and Nuria Rodríguez Rogil, from the Information and Communication Technology team of SUMMA 112.
We also thank Sara Pérez-Martínez, methods specialist of the FIIBAP and SUMMA 112.
M. Isabel Pescador-Chamorro, Department of Neonatology, Hospital Gregorio Marañón. Neonatal Transport system of the Community of Madrid-SUMMA 112. Madrid, Spain.
Itziar Marsinyach-Ros, Department of Neonatology, Hospital Gregorio Marañón. Neonatal Transport system of the Community of Madrid-SUMMA 112. Madrid, Spain.
Rocío Mosqueda-Peña, Department of Neonatology, Hospital 12 de Octubre. Neonatal Transport system of the Community of Madrid-SUMMA 112. Madrid, Spain.
Noelia Ureta-Velasco, Department of Neonatology, Hospital 12 de Octubre. Neonatal Transport system of the Community of Madrid-SUMMA 112. Madrid, Spain.
M. José Rodríguez Castaño, Department of Neonatology, Hospital Clínico de San Carlos. Neonatal Transport system of the Community of Madrid-SUMMA 112. Madrid, Spain.
Eva Vierge-Hernán, Department of Neonatology, Hospital Gregorio Marañón. Neonatal Transport system of the Community of Madrid-SUMMA 112. Madrid, Spain.
Ana Sánchez-Torres, Department of Neonatology, Hospital Universitario La Paz. Neonatal Transport system of the Community of Madrid-SUMMA 112. Madrid, Spain.
Jordi Martí-Centeno, Universidad Politécnica de Madrid. Madrid. Spain.
Marina Gómez-Morán Quintana, Medical Emergency System of the Community of Madrid (SUMMA 112). Madrid, Spain.
Soledad Gómez de la Oliva, Medical Emergency System of the Community of Madrid (SUMMA 112). Madrid, Spain.
Beatriz Jiménez Sánchez-Carpio, Medical Emergency System of the Community of Madrid (SUMMA 112). Madrid, Spain.
Ana Torres-Poza, Medical Emergency System of the Community of Madrid (SUMMA 112). Madrid, Spain.
María Isabel Sánchez-Sáenz, Medical Emergency System of the Community of Madrid (SUMMA 112). Madrid, Spain.
Jorge Lorente-Romero, Medical Emergency System of the Community of Madrid (SUMMA 112). Madrid, Spain.
Elena Pastor-Benito, Medical Emergency System of the Community of Madrid (SUMMA 112). Madrid, Spain.
Elizabeth Hoyos-Loya, Escuela de Salud Pública de México. Cuernavaca, Morelos, Mexico.