This document is the result of previous work carried out by different expert groups and submitted to multidisciplinary debate at a conference about controversial, deficient, or new aspects in the field of neonatal palliative care, such as: 1) the deliberative decision-making process, 2) hospital and domiciliary palliative care, 3) donation after controlled cardiac death, and 4) moral stress in professionals.
The most relevant conclusions were: the need to instruct professionals in bioethics and in the deliberative method to facilitate thorough and reasonable decision-making; the lack of development in the field of perinatal palliative care and domiciliary palliative care in hospitals that attend newborns; the need to provide neonatal units with resources that help train professionals in communication skills and in the management of moral distress, as well as delineate operational procedure and guidelines for neonatal organ donation.
El presente documento es fruto del trabajo previo realizado por diferentes grupos de expertos y presentado a debate multidisciplinar en unas jornadas sobre aspectos controvertidos, deficientes o nuevos en el cuidado paliativo neonatal, como son: 1) el procedimiento deliberativo en la toma de decisiones; 2) el cuidado paliativo hospitalario y domiciliario; 3) la donación en asistolia controlada, y 4) el estrés moral en los profesionales.
Las conclusiones más relevantes fueron la necesidad de que los profesionales adquieran formación en bioética y se ejerciten en la práctica de la metodología deliberativa para facilitar la toma de decisiones prudentes y razonables; la falta de desarrollo en los hospitales que atienden recién nacidos, del cuidado paliativo perinatal y del cuidado paliativo domiciliario neonatal; la necesidad de facilitar a las Unidades Neonatales recursos que ayuden a capacitar a los profesionales en técnicas de comunicación y de gestión del estrés emocional, así como delinear procesos operativos y protocolos para la donación de órganos.
There are instances in which newborns present with problems that threaten their independent life in the first days or weeks of life. On such occasions, health professionals experience concerns as how to act in the best interest of the newborn and the family, continuing life-sustaining treatment or transitioning to palliative care (PC). Thus begins the challenging process of decision making, which involves the participation of the parents as well as every professional who provides care to the child, and requires the consideration of cultural, social and religious factors, among others.1,2
In 2013, the Working Group on Ethics of the Sociedad Española de Neonatología (Spanish Society of Neonatology) published an article with recommendations for end-of-life care (EoLC).3 However, there are still challenges in neonatal units regarding the availability of protocols and guidelines on how to facilitate the delivery of the best possible integral care to patients eligible for PC and their families. On the other hand, some novel and specific aspects associated with neonatal PC, such as home-based PC, organ donation and emotional support for health care professionals, have received little attention and are not known by many neonatology professionals.
In November 2015, a series of scientific meetings of national scope were held and attended by professionals in neonatology, psychology and bioethics to debate the challenges and emerging issues in the practical delivery of neonatal PC. Four workgroups were established with the purpose of developing recommendations based on the scientific literature, ethical principles and personal experience, and this document presents the conclusions that they reached in relation to: 1) the deliberative process in decision making; 2) hospital-based PC and home-based PC; 3) controlled donation after cardiac death and 4) moral distress in health care professionals.
MethodsIn the months that preceded the meetings, the coordinator (JA) met regularly with the head of each workgroup (JCT, SC, MM, MTM). Each group summarised the current experience in their field and the evidence found in databases such as PubMed, EMBASE and the Cochrane library. The day of the scientific meetings, brief presentations were made on each topic, specifying the most controversial points, and allowing time for the reflections of the experts in attendance.
In the elaboration of this article, we have used the summary made by each workgroup, the information obtained during the debates and the recordings of the meetings. We have summarised the information in a brief text, presenting the framework of each subject and highlighting the most important contents. We have produced figures and tables to summarise and supplement aspects subject to the most debate or consideration.
Deliberation as a process for decision making in neonatal careHealth professionals devoted to the care of ill newborns often face complex decisions with a high clinical and ethical uncertainty. One such scenario is that of patients with a poor prognosis eligible for treatment with aggressive and invasive procedures, but whose potential benefits are questionable and that carry a high risk of causing pain and discomfort, prolonging the dying process unnecessarily or greatly impairing the patients’ quality of life.1,3
In neonatal medicine, the professionals that care for the patient and the parents are the individuals responsible for making decisions based on the “best interest” of the patient. However, when it comes to severely ill newborns, there may be widely different views on what may be best for the patient, as the values of the individuals responsible for making the decision come into play in defining such best interest.4
This gives rise to the difficulties involved in making the best decision in the context of ethical uncertainty as to what constitutes the best interest. Medicine, like clinical ethics, is a practical discipline based on the logic of probability as opposed to the logic of certainty. This means that while uncertainty should be reduced to the minimum possible in decision making, it cannot be eliminated completely. Thus, the goal is not to achieve certainty, which does not exist, but to manage uncertainty rationally and make a sensible decision. This is attained through a process of deliberation.5–7
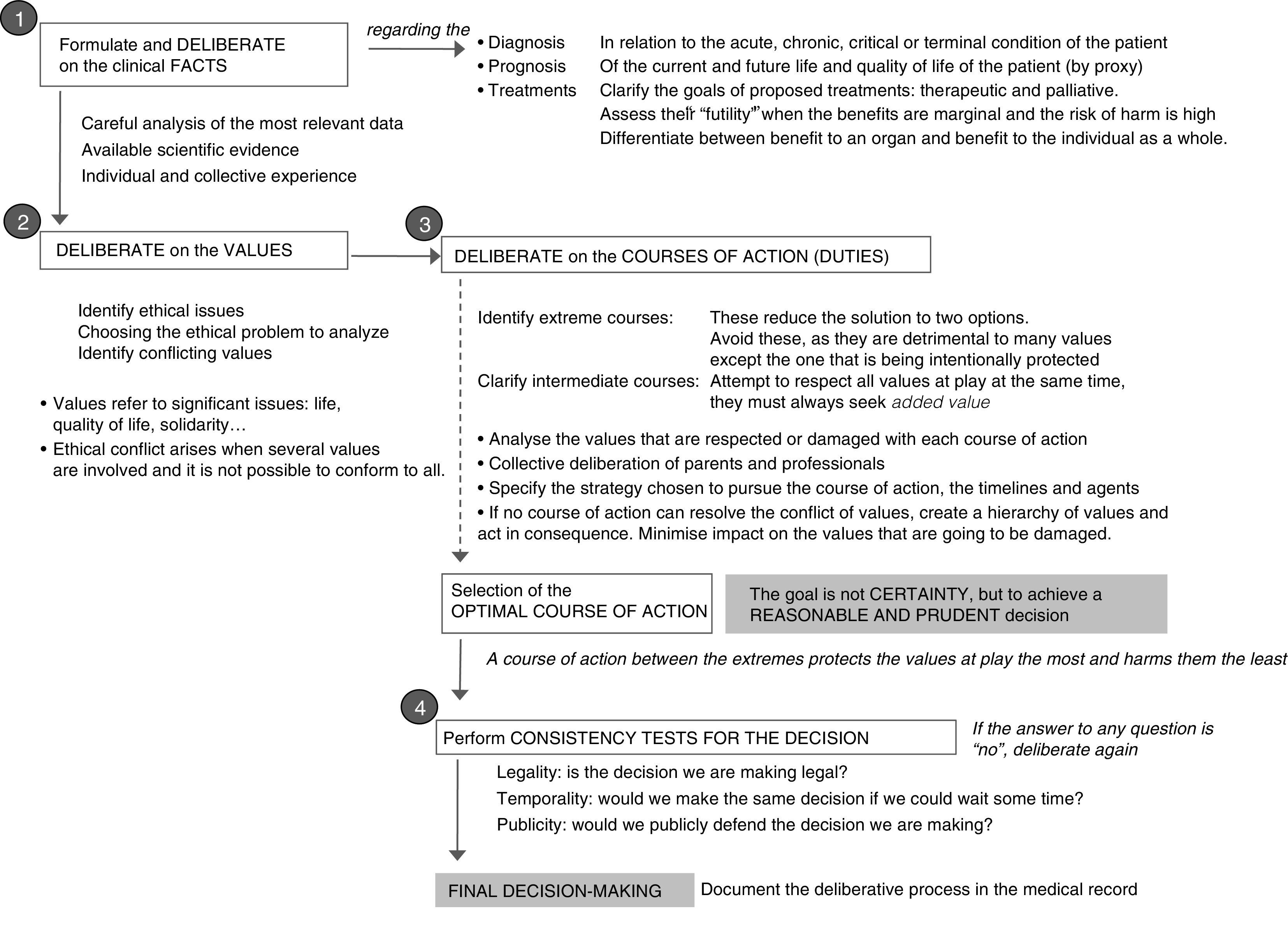
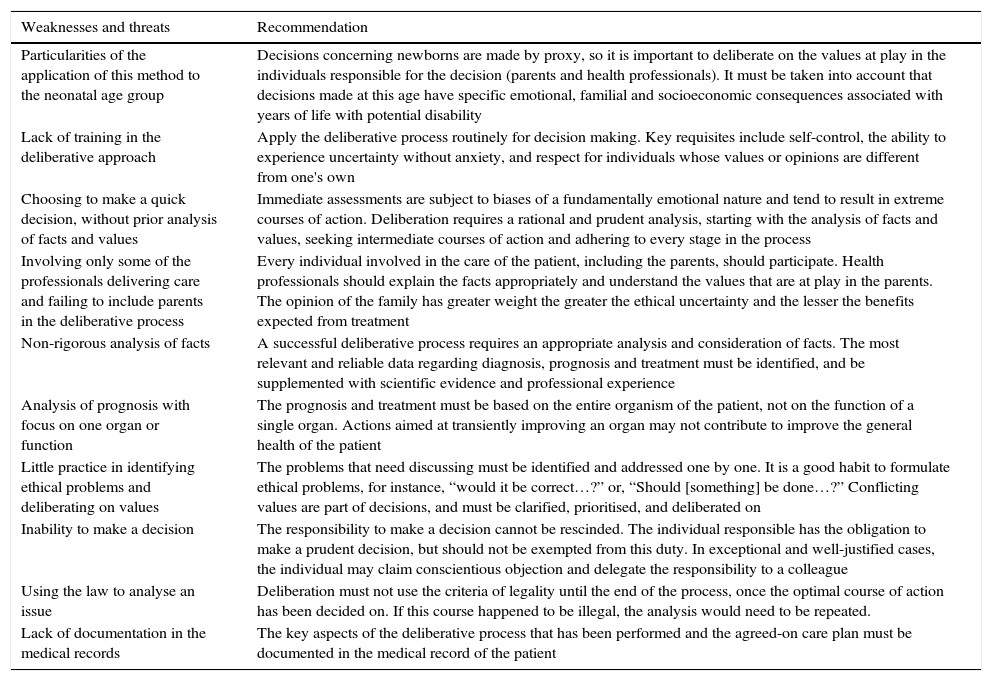
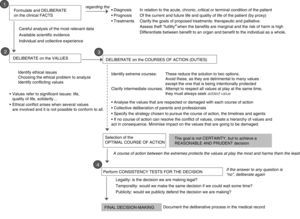
The systematic use of the deliberative process is a tool that can be very useful in clinical decision making in the field of neonatology, but it requires learning and practice.7 This tool is not restricted to ethics committees, but is available to health professionals facing conflict-ridden situations, especially if there is ethical uncertainty. This process entails an ordered sequence of actions that can be summarised into deliberating on: 1) the facts, 2) the conflicting values and 3) the possible courses of action, as well as the circumstances and predicted consequences of the decision to be made (Fig. 1 and Table 1).
Challenges associated with the deliberative process in the Neonatal Unit.
| Weaknesses and threats | Recommendation |
|---|---|
| Particularities of the application of this method to the neonatal age group | Decisions concerning newborns are made by proxy, so it is important to deliberate on the values at play in the individuals responsible for the decision (parents and health professionals). It must be taken into account that decisions made at this age have specific emotional, familial and socioeconomic consequences associated with years of life with potential disability |
| Lack of training in the deliberative approach | Apply the deliberative process routinely for decision making. Key requisites include self-control, the ability to experience uncertainty without anxiety, and respect for individuals whose values or opinions are different from one's own |
| Choosing to make a quick decision, without prior analysis of facts and values | Immediate assessments are subject to biases of a fundamentally emotional nature and tend to result in extreme courses of action. Deliberation requires a rational and prudent analysis, starting with the analysis of facts and values, seeking intermediate courses of action and adhering to every stage in the process |
| Involving only some of the professionals delivering care and failing to include parents in the deliberative process | Every individual involved in the care of the patient, including the parents, should participate. Health professionals should explain the facts appropriately and understand the values that are at play in the parents. The opinion of the family has greater weight the greater the ethical uncertainty and the lesser the benefits expected from treatment |
| Non-rigorous analysis of facts | A successful deliberative process requires an appropriate analysis and consideration of facts. The most relevant and reliable data regarding diagnosis, prognosis and treatment must be identified, and be supplemented with scientific evidence and professional experience |
| Analysis of prognosis with focus on one organ or function | The prognosis and treatment must be based on the entire organism of the patient, not on the function of a single organ. Actions aimed at transiently improving an organ may not contribute to improve the general health of the patient |
| Little practice in identifying ethical problems and deliberating on values | The problems that need discussing must be identified and addressed one by one. It is a good habit to formulate ethical problems, for instance, “would it be correct…?” or, “Should [something] be done…?” Conflicting values are part of decisions, and must be clarified, prioritised, and deliberated on |
| Inability to make a decision | The responsibility to make a decision cannot be rescinded. The individual responsible has the obligation to make a prudent decision, but should not be exempted from this duty. In exceptional and well-justified cases, the individual may claim conscientious objection and delegate the responsibility to a colleague |
| Using the law to analyse an issue | Deliberation must not use the criteria of legality until the end of the process, once the optimal course of action has been decided on. If this course happened to be illegal, the analysis would need to be repeated. |
| Lack of documentation in the medical records | The key aspects of the deliberative process that has been performed and the agreed-on care plan must be documented in the medical record of the patient |
The uncertainty regarding the outcome of many illnesses has been described as one of the most frequent barriers experienced by professionals when it comes to initiating PC. However, there are many diseases that, once diagnosed, should lead to a palliative approach due to their life-threatening or life-altering nature, without waiting for the patient to arrive to the final stage when approaches other than PC have been exhausted.8 The neonatal period is the period in childhood when the risk of death is highest, mainly on account of congenital anomalies, preterm birth and its consequences, and perinatal asphyxia.3,9 There are 3 general areas in which PC is required: foetuses/newborns with fatal congenital anomalies, preterm newborns at the limit of viability, and those that do not respond to intensive care.
Despite the advances in perinatal PC in recent decades, there is not a standardised best care model for it.10 In recent years, emphasis has been placed on the importance of initiating PC at an early stage, even before birth.10–12 In perinatal PC (“perinatal hospice”), neonatologists and obstetricians need to establish an interdisciplinary care plan with the agreement of the parents and before birth. Although perinatal PC is not practiced in every hospital, there is evidence of benefits to patients and their parents in its implementation, especially in that it facilitates bonding, parting, and bereavement.10,11,13–15
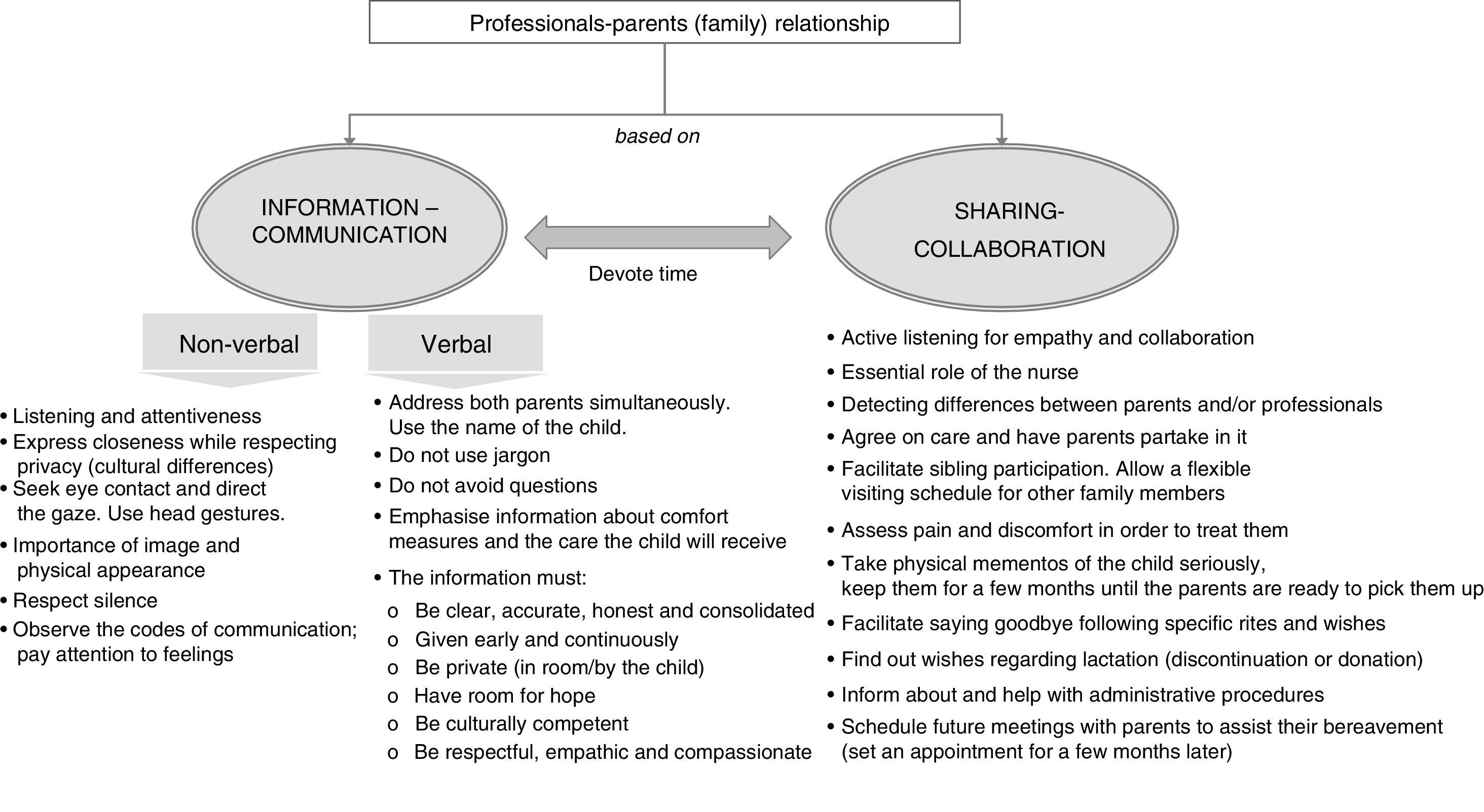
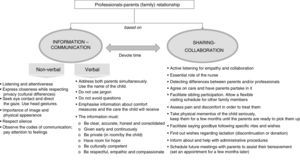
One of the cornerstones of PC is establishing trust through verbal as well as nonverbal communication.2,3,13,16 Such communication requires dedication, empathy and patience, helping parents understand what is happening, the changes that are going to take place and the resources that are available. We need to be empathic in promoting the bonding of parents with the child, so that they partake in the care and in decision making. We need to engage in active listening to learn about their fears, wishes and expectations, allowing them to express their feelings and identifying what matters to them, so that we can establish a therapeutic partnership that takes into account spiritual particularities and anticipate their requests2,13,16,17 (Fig. 2).
Palliative care must promote and maximise the newborn's wellbeing, provide an appropriate environment for death, ideally in an individual room, and facilitate the rites and customs of each family, taking into account psychological, emotional and spiritual aspects in the child and the family.12 Contact with the child should be promoted (skin-to-skin contact, caresses, holding, etc.) as well as the presence of parents at the time of the child's death.15 We could explicitly ask parents: What would you like to do with your child before we adjust treatment?18 When health care professionals accompany families in this process appropriately, it helps the family come to terms with their loss and initiate a healthy bereavement process (Table 2).2,3,13,16,17 The entire care team must be acquainted with the process that has been agreed with the parents to avoid inconsistencies or dissonance in communication and care.19 The nurse, who is the main link between the parents and the medical team, is key in the communication process, filling gaps in information and ensuring that information is well understood. The unit must be reorganised so that one nurse is exclusively dedicated to the child and his or her family17,19 (Fig. 2).
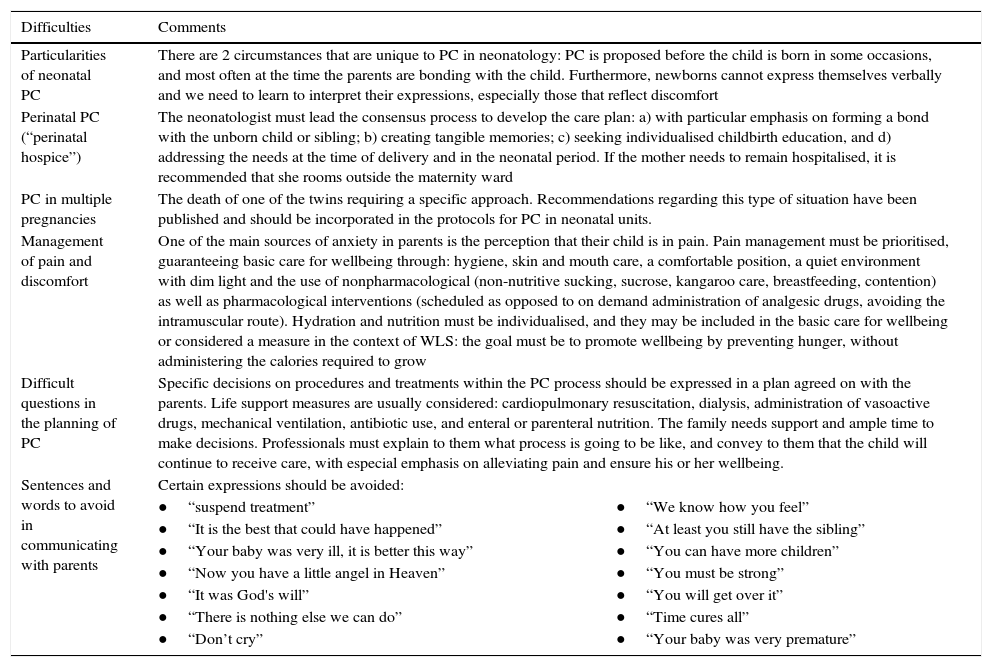
Difficulties and challenges in the implementation of neonatal PC.
| Difficulties | Comments | |
|---|---|---|
| Particularities of neonatal PC | There are 2 circumstances that are unique to PC in neonatology: PC is proposed before the child is born in some occasions, and most often at the time the parents are bonding with the child. Furthermore, newborns cannot express themselves verbally and we need to learn to interpret their expressions, especially those that reflect discomfort | |
| Perinatal PC (“perinatal hospice”) | The neonatologist must lead the consensus process to develop the care plan: a) with particular emphasis on forming a bond with the unborn child or sibling; b) creating tangible memories; c) seeking individualised childbirth education, and d) addressing the needs at the time of delivery and in the neonatal period. If the mother needs to remain hospitalised, it is recommended that she rooms outside the maternity ward | |
| PC in multiple pregnancies | The death of one of the twins requiring a specific approach. Recommendations regarding this type of situation have been published and should be incorporated in the protocols for PC in neonatal units. | |
| Management of pain and discomfort | One of the main sources of anxiety in parents is the perception that their child is in pain. Pain management must be prioritised, guaranteeing basic care for wellbeing through: hygiene, skin and mouth care, a comfortable position, a quiet environment with dim light and the use of nonpharmacological (non-nutritive sucking, sucrose, kangaroo care, breastfeeding, contention) as well as pharmacological interventions (scheduled as opposed to on demand administration of analgesic drugs, avoiding the intramuscular route). Hydration and nutrition must be individualised, and they may be included in the basic care for wellbeing or considered a measure in the context of WLS: the goal must be to promote wellbeing by preventing hunger, without administering the calories required to grow | |
| Difficult questions in the planning of PC | Specific decisions on procedures and treatments within the PC process should be expressed in a plan agreed on with the parents. Life support measures are usually considered: cardiopulmonary resuscitation, dialysis, administration of vasoactive drugs, mechanical ventilation, antibiotic use, and enteral or parenteral nutrition. The family needs support and ample time to make decisions. Professionals must explain to them what process is going to be like, and convey to them that the child will continue to receive care, with especial emphasis on alleviating pain and ensure his or her wellbeing. | |
| Sentences and words to avoid in communicating with parents | Certain expressions should be avoided: | |
| ●“suspend treatment” | ●“We know how you feel” | |
| ●“It is the best that could have happened” | ●“At least you still have the sibling” | |
| ●“Your baby was very ill, it is better this way” | ●“You can have more children” | |
| ●“Now you have a little angel in Heaven” | ●“You must be strong” | |
| ●“It was God's will” | ●“You will get over it” | |
| ●“There is nothing else we can do” | ●“Time cures all” | |
| ●“Don’t cry” | ●“Your baby was very premature” | |
PC, palliative care; WLS, withdrawal of life support.
Hospital-based PC results in prolonged lengths of stay that have an impact on the child and on family dynamics, so PC should be offered wherever the family desires, be it in a hospital that is closer to the home or in the home itself.20,21 The PC strategy of the Spanish National Health System for the 2013–2016 period explicitly stated the objective of “providing the population of children and adolescents with advanced terminal disease and their families integral assessment and care adapted to present circumstances at all times, and at any point in the course of disease.” However, although the strategic plans of different autonomous communities reflect this need, the reality is that there are hardly any hospitals with integral PC units for the paediatric population.22 This deficit is even more marked when it comes to paediatric home-based PC programmes, which have hardly been introduced, and there are no specific protocols for neonatal patients guaranteeing the continuity of care throughout the process. Home-based EoLC must be planned with the parents, and parents and health professionals must have the necessary skills and equipment to deliver it. Physical, social, emotional and spiritual support must be provided to advance the wellbeing of the child and the family throughout the disease and during the bereavement process after the child's death (Table 2).
Entrance of a child to a PC programme does not end the relationship of the patient with the specialty care team that treats the underlying disease, and a collaborative care approach should be promoted. The entire PC process must be documented in the medical record, including the steps that were taken and any difficulties encountered.
Non-heart beating donation (Maastricht category III)Consideration of organ and tissue donation following death must be part of EoLC. Before implementing a type III neonatal donation programme, it is important that neonatal units have established EoLC programmes with the purpose of guaranteeing optimal EoLC independent of the donation process.
Spain has one of the highest rates of donation worldwide, with the lowest rates of family refusal. However, the gap between the supply and demand of organs for transplantation has been widening due to the decrease in mortality from traumatic brain injury and improvements in the treatment of neurocritical patients, with 7% to 9% of patients dying while on the waiting list each year.23
Infants aged less than 1 year who require a heart transplant are the group with the highest mortality rate among patients in transplant waiting lists. The need to increase donation rates has spurred the development of strategies worldwide, and in Spain in particular, to Plan 40 of the Spanish National Transplant Organization (ONT), to explore new pathways for organ donation and use, including non-heart beating donation. On the other hand, the need for organs in very young children has expanded the scope of this strategy to the paediatric and even the neonatal population.24
Unlike in donation following brain death, in non-heart beating donation the organs are harvested after the onset of ventricular asystole. It is also known as “donation after the circulatory determination of death,” as death is not determined based on the irreversible loss of cardiac function, but on the irreversible loss of circulatory (and respiratory) function.25 Death is confirmed after 5min of apnoea, unresponsiveness and an absent pulse (established by the absence of a curve in blood pressure monitoring or through echocardiography).26 Since the 1995 International Meeting in Maastricht, non-heart beating donors have been classified into four categories, and category III corresponds to donors in who the cessation of circulatory and respiratory function takes place after withdrawal of life support owing to the judgement that such support is futile.25
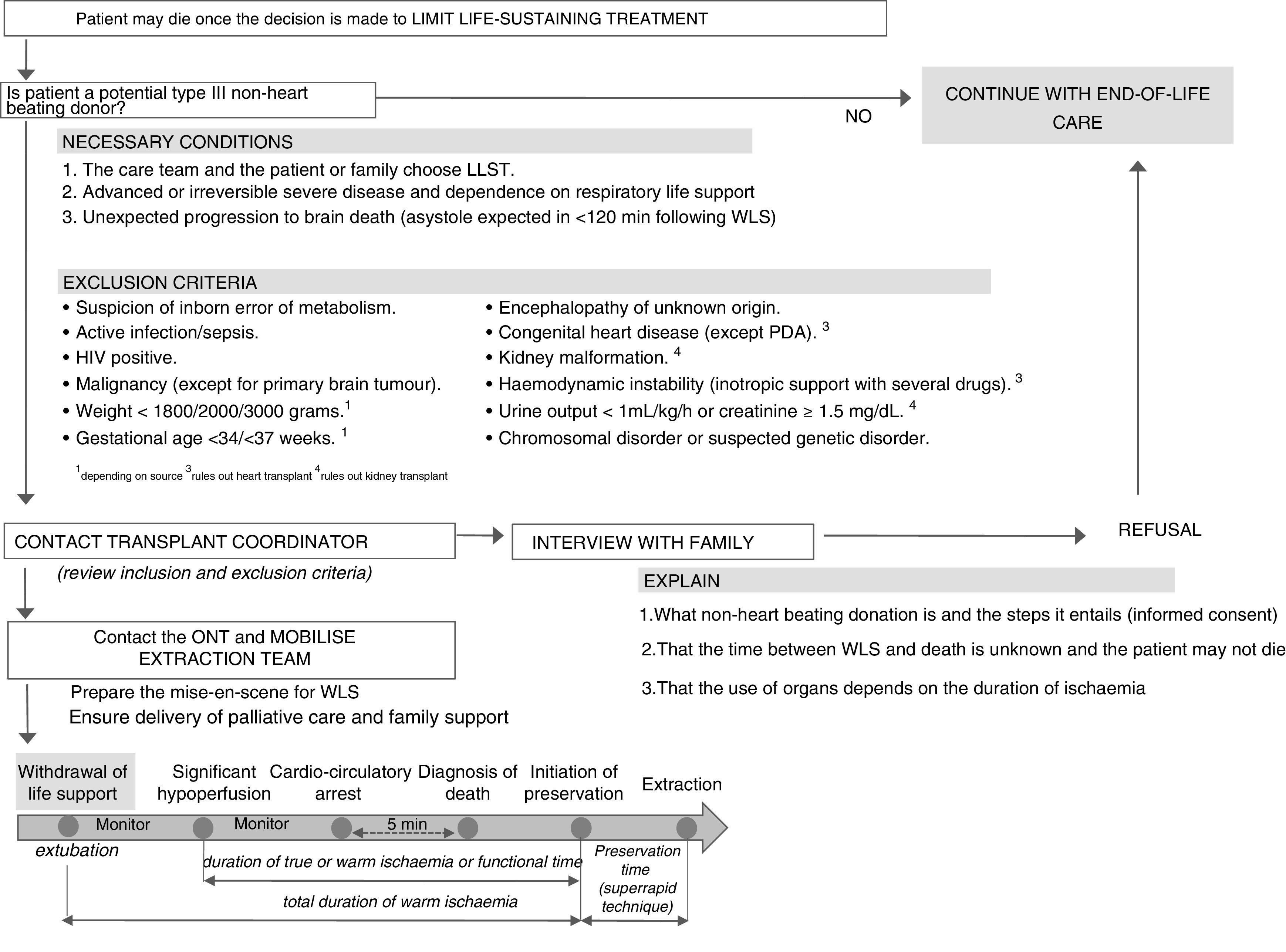
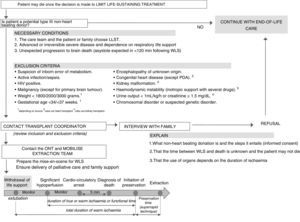
Decisions to withdraw or withhold treatment are currently part of neonatal clinical practice. Many patients die once the care team and the family make the decision to withdraw or withhold treatment. It is in such situations, if a series of requisites are met, that non-heart beating donation can be suggested (Fig. 3).
Management algorithm for a potential type III non-heart beating neonatal donor.
BP, blood pressure; ECG, electrocardiogram; EoLC, end-of-life care; LLST, limitation of life-sustaining treatment; PDA, patent ductus arteriosus; ONT, Spanish National Transplant Organization; WLS, withdrawal of life support.
Taking into account that half of paediatric deaths occur in the neonatal period and that most of them (68%–86%) follow decisions to withdraw or withhold treatment,3,27,28 as well as the difficulty of diagnosing brain death, neonatal intensive care units should consider the possibility of offering the option of controlled non-heart beating donation. Furthermore, the recent international literature includes several reports of successful transplantation of organs from non-heart beating donors,29,30 with statements in support of the incorporation of this type of donation in the neonatal period. It is estimated that between 6% and 8% of admitted newborns could be candidates for non-heart beating donation.24,31,32 On the other hand, there is a debate on some aspects of this type of donation, and of how it should be incorporated in neonatal care (Table 3).33,34
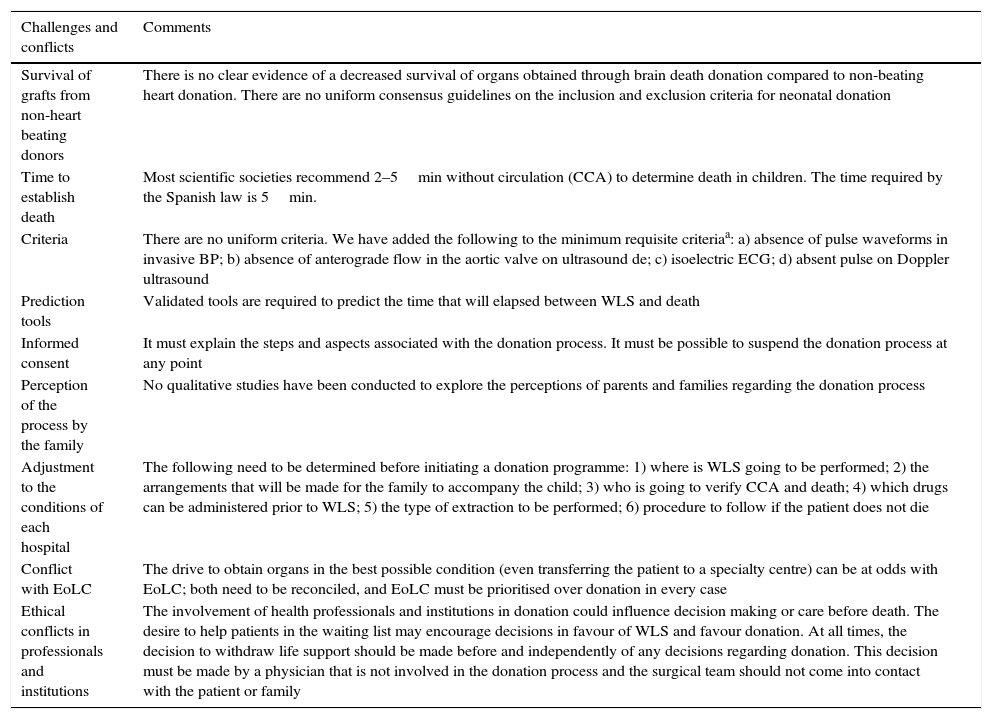
Challenges and conflicts in the incorporation of category III non-beating heart donation in neonatology.
| Challenges and conflicts | Comments |
|---|---|
| Survival of grafts from non-heart beating donors | There is no clear evidence of a decreased survival of organs obtained through brain death donation compared to non-beating heart donation. There are no uniform consensus guidelines on the inclusion and exclusion criteria for neonatal donation |
| Time to establish death | Most scientific societies recommend 2–5min without circulation (CCA) to determine death in children. The time required by the Spanish law is 5min. |
| Criteria | There are no uniform criteria. We have added the following to the minimum requisite criteriaa: a) absence of pulse waveforms in invasive BP; b) absence of anterograde flow in the aortic valve on ultrasound de; c) isoelectric ECG; d) absent pulse on Doppler ultrasound |
| Prediction tools | Validated tools are required to predict the time that will elapsed between WLS and death |
| Informed consent | It must explain the steps and aspects associated with the donation process. It must be possible to suspend the donation process at any point |
| Perception of the process by the family | No qualitative studies have been conducted to explore the perceptions of parents and families regarding the donation process |
| Adjustment to the conditions of each hospital | The following need to be determined before initiating a donation programme: 1) where is WLS going to be performed; 2) the arrangements that will be made for the family to accompany the child; 3) who is going to verify CCA and death; 4) which drugs can be administered prior to WLS; 5) the type of extraction to be performed; 6) procedure to follow if the patient does not die |
| Conflict with EoLC | The drive to obtain organs in the best possible condition (even transferring the patient to a specialty centre) can be at odds with EoLC; both need to be reconciled, and EoLC must be prioritised over donation in every case |
| Ethical conflicts in professionals and institutions | The involvement of health professionals and institutions in donation could influence decision making or care before death. The desire to help patients in the waiting list may encourage decisions in favour of WLS and favour donation. At all times, the decision to withdraw life support should be made before and independently of any decisions regarding donation. This decision must be made by a physician that is not involved in the donation process and the surgical team should not come into contact with the patient or family |
BP, blood pressure; CCA, cardiocirculatory arrest; ECG, electrocardiogram; EoLC, end-of-life care; WLS, withdrawal of life support.
Standard minimum criteria: 1) absence of palpable pulse; 2) absence of lung sounds; 3) absence of heart sounds; 4) absence of respiratory effort or chest wall movements; 5) drop in non-invasive arterial pressure; 6) coma and dilated pupils; 7) pulseless electrical activity. Pulse oximetry is not a reliable indicator to establish the absence of a pulse.
Such a programme requires training, practice, and the design of specific protocols led by a multidisciplinary team with participation of all professionals involved in the process (ONT, neonatologists, paediatric critical care specialists, transplant coordinators, surgeons, anaesthesiologists, nurses etc.). The introduction of donation in neonatal patients must occur in the framework of a nationwide programme in order to allocate the organs to the most suitable patients and to prevent their death while in the waiting list.
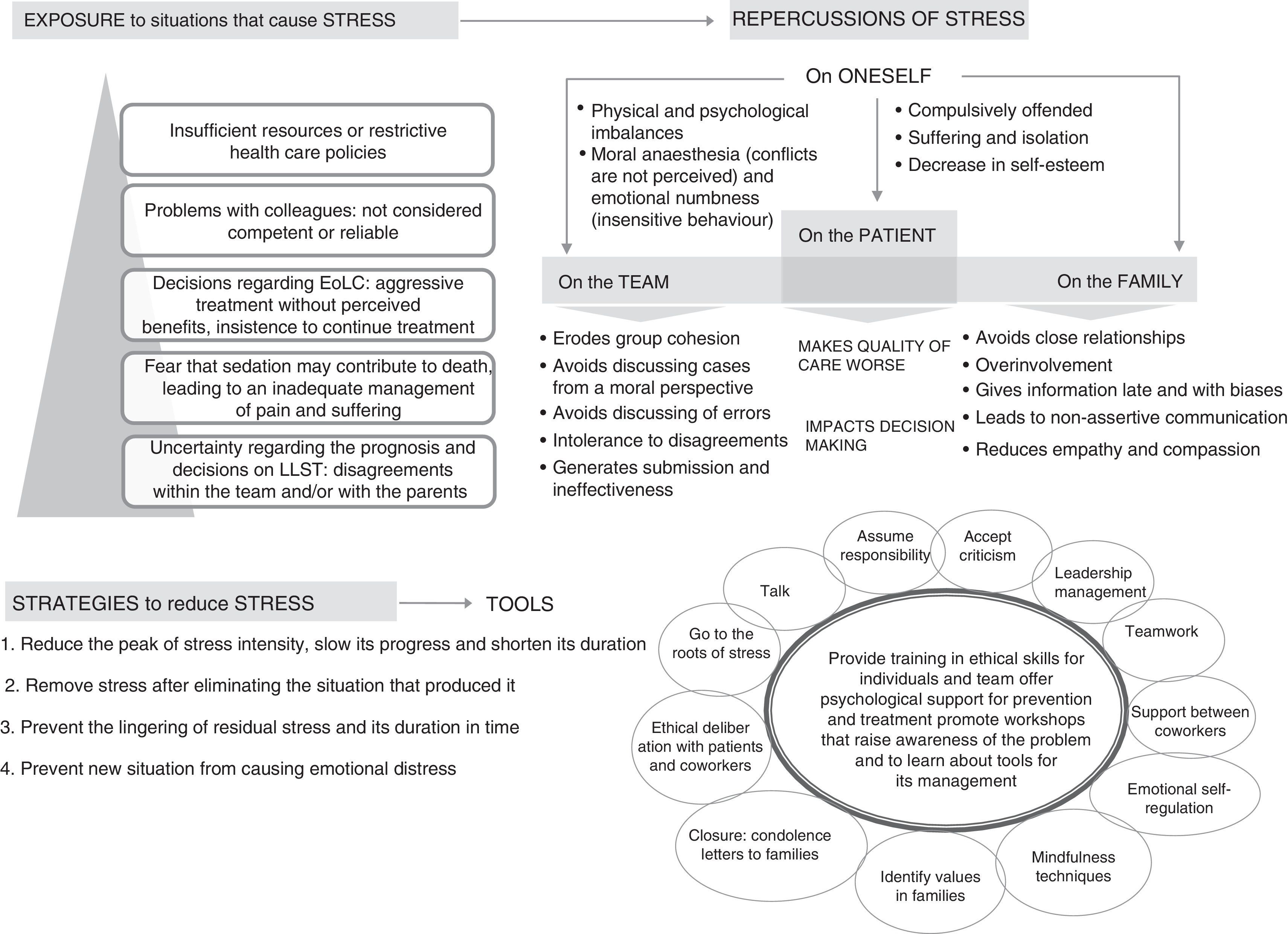
Moral–emotional distress in neonatal care professionalsJameton provided the first definition of moral distress as knowing the right course of action but being unable to pursue it, leading to psychological suffering and/or disturbances in health professionals.35 Thus, moral distress refers to stress associated with ethical concerns and with the perception of being unable to act according to one's conscience.36
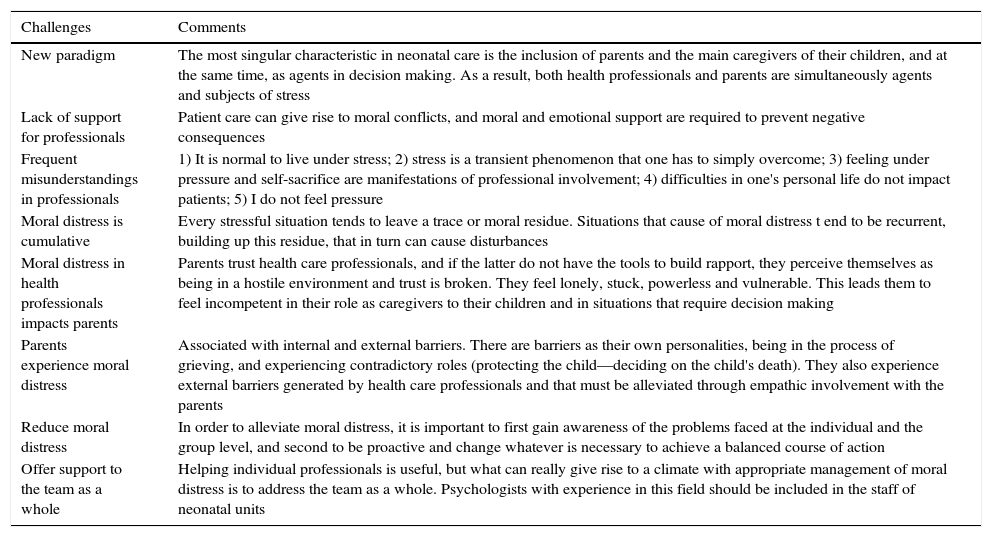
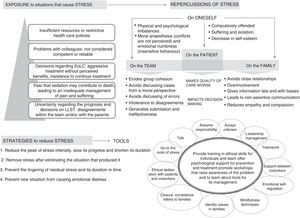
Among the situations that carry a risk of moral distress, some are particularly likely to cause it.37–39 In addition, the distress experienced by a single professional is not contained to the individual, but is conveyed to the team, impacting the care of the patient and the family3 (Fig. 4).
Moral distress is not an occasional time-limited psychological phenomenon. Health professionals face and ‘overcome’ moral and ethical problems frequently. However, each deliberation and each decision have a psychological and moral toll that persists in the form of what Epstein and Hamrictermed amoral residue.40 This moral residue can have a cumulative effect unless individual and group mechanisms are set in place to address and resolve it. Clinical bioethics can be a helpful tool to reduce moral distress insofar as it helps to manage ethical conflicts better.
Individual, group and institutional factors contribute to the development, progression and perpetuation of moral distress. On one hand, an individual's personality and coping skills to face and resolve situations that pose a psychological or moral conflict can act as risk or protective factors for moral distress. On the other hand, workplace-related factors, such as the ethical climate, the internal organisation, communication between professionals or the relationship with the management are elements that can also promote or protect against moral distress in health professionals and in families.
But as is the case of any stress, that is, of any emotional response to an actual event (or the experience of such event), moral distress can be a useful element in improving the status quo. Very low levels or the absence of moral distress could be indicative of low expectations and a greater degree of conformity. Thus, the goal is not to achieve the absence of moral distress, but to detect and manage it at the levels of the individual, the group and the institution, which should be a priority in national public health systems. In this sense, the need for psychological support is not exclusive to patients and their families, but also extends to professionals. Caring for vulnerable patients, especially patients that may die, can have a negative impact on health professionals and therefore reduce or end their motivation and the expectations they have set for themselves both in their personal and professional lives, to the point that it may influence decision making.3 Therefore, the development of specific skills to manage emotions is essential in the health care system at large and in neonatal units in particular. The strategies implementedto control and reduce moral distress must be based on: 1) the need to care for oneself to be able to care for others; 2) the introduction of “self-care” dynamics in teams and 3) improving training on “communication skills”.
Strategies that facilitate the identification and channelling of emotions or the management of their intensity, such as being fully present, or “mindfulness”, can be a great help in retaining composure and empathy, and allow us to choose how to act, as opposed to falling into reactive and automatic patterns of behaviour (Fig. 4 and Table 4).
Challenges associated with moral distress in neonatal care.
| Challenges | Comments |
|---|---|
| New paradigm | The most singular characteristic in neonatal care is the inclusion of parents and the main caregivers of their children, and at the same time, as agents in decision making. As a result, both health professionals and parents are simultaneously agents and subjects of stress |
| Lack of support for professionals | Patient care can give rise to moral conflicts, and moral and emotional support are required to prevent negative consequences |
| Frequent misunderstandings in professionals | 1) It is normal to live under stress; 2) stress is a transient phenomenon that one has to simply overcome; 3) feeling under pressure and self-sacrifice are manifestations of professional involvement; 4) difficulties in one's personal life do not impact patients; 5) I do not feel pressure |
| Moral distress is cumulative | Every stressful situation tends to leave a trace or moral residue. Situations that cause of moral distress t end to be recurrent, building up this residue, that in turn can cause disturbances |
| Moral distress in health professionals impacts parents | Parents trust health care professionals, and if the latter do not have the tools to build rapport, they perceive themselves as being in a hostile environment and trust is broken. They feel lonely, stuck, powerless and vulnerable. This leads them to feel incompetent in their role as caregivers to their children and in situations that require decision making |
| Parents experience moral distress | Associated with internal and external barriers. There are barriers as their own personalities, being in the process of grieving, and experiencing contradictory roles (protecting the child—deciding on the child's death). They also experience external barriers generated by health care professionals and that must be alleviated through empathic involvement with the parents |
| Reduce moral distress | In order to alleviate moral distress, it is important to first gain awareness of the problems faced at the individual and the group level, and second to be proactive and change whatever is necessary to achieve a balanced course of action |
| Offer support to the team as a whole | Helping individual professionals is useful, but what can really give rise to a climate with appropriate management of moral distress is to address the team as a whole. Psychologists with experience in this field should be included in the staff of neonatal units |
Establishing an individualised PC plan requires a previous deliberative process including a rigorous analysis of clinical facts and consideration of the conflicting values to arrive to a prudent and reasonable course of action. This adjustment in patient care requires communication and collaboration between health professionals and parents, with the support of allied care specialists to help manage the resulting moral distress.
There are significant gaps in the clinical bioethics training of professionals involved in care delivery. We would recommend the incorporation of continuing education on the application of the deliberative process to any situation involving ethical uncertainty in clinical practice. We also need specific training in communication skills and the management of moral distress in particularly delicate situations, such as those surrounding PC. Ultimately, it is health care professionals, hospitals and society as a whole that need to facilitate the structural and organisational changes that would allow families to make choices and exert their rights as caregivers and agents in decision-making processes involving their children.
Conflicts of interestThe authors have no conflicts of interest to declare
We thank the professionals that attended the debates in the Scientific Meetings for their contributions, which have enriched the contents of this document. We are also grateful for the interest of the Fundación NeNe in this subject, which led it to organise this Meeting and fund a considerable part of its cost.
Diego Gracia (Universidad Complutense de Madrid), Fermín García-Muñoz (Hospital Universitario [HU] Materno-Infantil de Gran Canaria), Lydia Feyto (Universidad Complutense de Madrid), Miguel García (HUSant Joan de Déu of Barcelona), Carmen R. Pallás (HU 12 de Octubre of Madrid), Sergi Navarro (HUSant Joan de Déuof Barcelona), Pedro Enriquez (HU Río Hortegaof Valladolid), Jesús Sanchez (HU Río Hortegaof Valladolid), Baltasar Pérez (HU Río Hortegaof Valladolid), Francisco Hernández (HU La Paz), Purificación Sierra (UNED andHU 12 de Octubre of Madrid), Helena García (HU La Paz of Madrid), Carolina del Rincón (HU Niño Jesús of Madrid).
Please cite this article as: Arnaez J, Tejedor JC, Caserío S, Montes MT, Moral MT, González de Dios J, et al. La bioética en el final de la vida en neonatología: cuestiones no resueltas. An Pediatr (Barc). 2017;87:356.e1–356.e12.