The aim of the study was to describe the neuropsychological profile of patients with attention deficit hyperactivity disorder (ADHD) and the impact of the disorder on executive functioning and academic performance.
Patients and methodsWe conducted a retrospective observational and analytical study. The sample consisted of 24 children with a diagnosis of ADHD (aged 6–15 years) without pharmacological treatment and 24 controls without ADHD (aged 7–15 years). A comprehensive neuropsychological evaluation was carried out, encompassing major cognitive domains, in addition to assessment of executive functioning and psychopathological symptoms through the administration of questionnaires to parents and teachers.
ResultsThe cognitive profile of the ADHD group was characterized by overall scores (including executive functions and academic abilities) in the normal range (z scores between −1 and 1), although significantly lower compared to the control group. Over half of the patients with ADHD (58%) had associated specific learning disorders. Furthermore, teachers tended to report executive function difficulties more frequently in male students.
ConclusionsIn the study sample, the group of patients with ADHD exhibited cognitive performance within the normal range, although with lower scores compared to controls. Behavioural rating scales provide valuable information about functioning outside the clinic, but may yield biased results on account of the focus on externalising symptoms. The neuropsychological evaluation is a useful tool that can facilitate the diagnosis of ADHD and an effective response to the needs and characteristics of patients and families.
El objetivo del presente estudio es describir el perfil neuropsicológico de los pacientes con trastorno por déficit de atención con hiperactividad (TDAH) y su impacto en las funciones ejecutivas y académicas.
Pacientes y métodosSe realizó un estudio analítico, observacional y retrospectivo. La muestra está compuesta por 24 sujetos con diagnóstico de TDAH (6–15 años) sin tratamiento farmacológico y 24 controles (7–15 años) sin TDAH. Se realizó una evaluación neuropsicológica completa que abarcase los principales dominios cognitivos, así como la evaluación mediante cuestionarios a padres y profesores del funcionamiento ejecutivo y sintomatología psicopatológica.
ResultadosEl perfil cognitivo del grupo con TDAH se caracteriza por presentar puntuaciones globales (incluidas funciones ejecutivas y habilidades académicas) dentro del rango de la normalidad (puntuaciones z entre −1 y 1), aunque significativamente menores que las del grupo. Más de la mitad de los sujetos (58%) con TDAH presentan trastornos específicos de aprendizaje de manera comórbida. Por otro lado, los profesores tienden a informar de más dificultades de tipo ejecutivo cuando los sujetos son varones.
ConclusionesEn nuestro grupo de estudio los pacientes diagnosticados con TDAH se caracterizan por presentar un rendimiento cognitivo dentro de la normalidad, aunque con menores puntuaciones que los controles. Los cuestionarios de conducta proporcionan información muy valiosa sobre el funcionamiento en entornos fuera de la consulta, pero pueden presentar sesgos al predominar los síntomas externalizantes. La evaluación neuropsicológica es una herramienta útil que puede facilitar el diagnóstico del TDAH y dar una respuesta eficaz a las características y necesidades de los pacientes y sus familias.
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by inattention, hyperactivity and impulsivity. The symptoms can affect the areas of cognition, behaviour, emotion and social functioning.1
Attention deficit hyperactivity disorder is fairly prevalent in children and adolescents. The global prevalence ranges between 5.9% and 7.1%, and it has been estimated at 6.8% in Spain.2 It is generally more prevalent in boys compared to girls, with a ratio that ranges from 2:1 to 9:1.3 Longitudinal studies suggest that one to two thirds of individuals given a diagnosis of ADHD in childhood continue to have symptoms in adulthood.4 When it comes to the core symptoms, differences based on sex have been reported, as boys are more likely to exhibit a hyperactive pattern and tend to have poorer response inhibition and cognitive flexibility compared to girls.5
In the field of neuropsychology, the role of frontal neural networks and executive functions, especially in attentional control, cognitive flexibility, planning and vigilance. Research has shown that young children with ADHD have problems doing tasks that require attentional control, including the abilities to stay focused, switch tasks and avoid distractions.6 There is also evidence of a decreased cognitive flexibility in individuals with ADHD, which is reflected in difficulty adjusting behaviour to different situations or shift cognitive sets.7 The impact of ADHD on executive functions can have important repercussions on the development and wellbeing of children. Individuals with difficulties in reading and writing usually have underlying impairments in phonological processing but also in other processes, including executive functions. In fact, the association between ADHD and reading and writing learning disabilities is frequent, with the prevalence of such comorbidities estimated at 15%–30%.8
One of the key elements in the diagnosis of ADHD is the assessment of the symptoms in different settings, that is, at school and at home. One of the greatest challenges of neuropsychological evaluations is the ecological validity of the tests, that is, the differences that may exist between what is measured by the applied tests and actual functioning outside the care setting.9 In many cases, test scores are not an accurate reflection of the actual difficulties experienced by individuals with ADHD, as the structure of the tests may facilitate performance and mask problems. For the purpose of assessing the degree of the problems that children experience at school and at home and the resulting impact, in addition to the interview, it may be helpful to use standardised questionnaires to document and quantify these difficulties.10
The primary objective of our study was to improve our knowledge of the cognitive phenotype of patients with a diagnosis of ADHD. To this end, we assessed the impact of ADHD on cognitive functions (including executive functions), and, given the known association with learning disorders, the incidence of difficulties in the basic areas of learning in boys and girls with ADHD. Due to the different presentation described in relation to sex in children and adolescents, we also decided to assess whether there were differences based on sex in the information provided by parents and teachers in the questionnaires for the ADHD group. Our aim is to increase our understanding of ADHD, as it does not focus solely on executive functions, but entailed an exhaustive evaluation encompassing the main domains of cognition.
Sample and methodsWe conducted a retrospective observational and analytical study. The total sample (N = 48) comprised 2 groups: a group of children with a diagnosis of ADHD (n = 24) referred to our centre for evaluation, and a control group of neurotypical children (n = 24) without a diagnosis of ADHD, selected from the database of the child and adolescent clinical psychology outpatient clinic of our hospital.
The criteria for inclusion in the ADHD group were: (1) Age 6–18 years, (2) having received a diagnosis of ADHD based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria, and not having received another psychiatric diagnosis (except for ADHD and specific learning disorders as defined in the DSM-5. The exclusion criteria were: (1) having significant and uncorrected sensory disorders that could have been a source of bias evaluation, (2) having any form of neurologic disease or medical condition (including intellectual disability or other neurodevelopmental disorders) that could affect the results of the evaluation, (3) being in treatment with psychotropic medication at the time of the evaluation (4) not having ever received any form of medication for ADHD and (5) abnormal behaviour during the assessment that could have affected the results.
The inclusion criteria for the neurotypical control group were: (1) age 6–18 years and (2) not having received a diagnosis of ADHD based on the DSM-5 criteria. The exclusion criteria were: (1) having significant and uncorrected sensory disorders that could have been a source of bias evaluation, (2) having any form of neurologic disease or medical condition (including neurodevelopmental disorders) that could affect the results of the evaluation, (3) being in treatment with psychotropic medication at the time of the evaluation and (4) abnormal behaviour during the assessment that could have affected the results.
We reviewed the health records of the patients who came to our clinic for evaluation between January 2018 and January 2023, collecting data on sociodemographic and family characteristics and the diagnosis based on the DSM-5. The patients who underwent assessment were not currently receiving nor had ever received pharmacological treatment for ADHD. The neuropsychological evaluation was carried out by a clinical psychologist with specialised training on clinical neuropsychology. The evaluation protocol comprised validated individual tests and batteries applied domestically and internationally to assess the main cognitive domains and self-report questionnaires for parents and teachers to assess executive functioning and behavioural and emotional problems in the child. Table 1 details the cognitive domains assessed in the evaluation and the tests that were used for the purpose.
Cognitive domains and neuropsychological tests.
| Cognitive domain | Neuropsychological tests |
|---|---|
| General cognitive skills | Wechsler Intelligence Scale for Children, Fifth Edition (WISC-V), Wechsler Preschool & Primary Scale of Intelligence, Fourth Edition (WPPSI-IV)11,12 |
| Motor skills | Wide Range Assessment of Visual Motor Abilities (WRAVMA)13 |
| Perceptual reasoning | Batería III of Woodcock-Muñoz14Kaufman Assessment Battery for Children-2 (KABC-2)15 |
| Nonverbal skills | Developmental Neuropsychological Assessment Second Edition (NEPSY-II)16 |
| Rey Complex Figure test17 | |
| Abstract reasoning | Matrix reasoning and similarities subtests (WISC-V)11 |
| Language skills | NEPSY-II16 |
| KABC-215 | |
| Clinical Evaluation of Language Fundamentals, Fifth Edition (CELF-5)18 | |
| Memory skills | California Verbal Learning Test Second Edition (CVLT-II)19Reynolds intellectual assessment scales (RIAS)20NEPSY-II16 |
| Batería III of Woodcock-Muñoz14 | |
| Attention skills | Test of Everyday Attention for Children (TEA-Ch)21WISC-V11Conners Kiddie Continuous Performance Test. 2ndedition (KCPT-2)22Conners Continuous Performance Test, Third Edition (CPT-3)23 |
| Executive functions | NEPSY-II16 |
| Children’s Color Trails Test (CCTT)24 | |
| WISC-V11 | |
| Academic skills | WISC-V11Batería III of Woodcock-Muñoz14 |
| British Ability Scales, Second Edition (BAS II)25 |
The administered tests are used in Spain and internationally in recognised units and have an adequate validity and reliability. All the tests have been validated and standardised in a Spanish sample, except the CCTT, the WRAVMA and the KABC-2.
Although theoretically there are 3 ADHD subgroups (inattentive, hyperactive and combined), we did not identify any patient in the hyperactive group. Given the reported variability of ADHD, and as proposed by other authors,26 we decided to divide the ADHD group into inattentive ADHD and combined ADHD subgroups, based on the DSM-5 criteria, for further comparison.
We have summarised qualitative variables as absolute and relative frequencies. To describe quantitative variables, we used measures of central tendency and dispersion: mean, median, standard deviation (SD) and minimum and maximum values (range). To determine whether the data followed a normal distribution, we used the Shapiro-Wilk test and graphic methods. Scores were normalised, calculating z scores (with mean = 0 and SD = 1) to be able to compare the scores of different tests. We considered that the patient had significant difficulties if the score in the given test was more than 1 SD below the mean (z < −1). To facilitate interpretation, we also recorded intelligence quotient scores (mean = 100; SD = 15). Although most variables fit a normal distribution, given the small sample size, especially in the comparison of the inattentive and combined subgroups, we decided to use nonparametric tests. To analyse the differences between groups, we used to Mann-Whitney U test for independent samples. Along the same lines, given the large number of variables and the sample size, we decided to group variables into cognitive domains based on the underlying theoretical construct of the tests and the mean scores of the different cognitive functions comprising the domain. All comparisons were two-tailed, and the level of significance was set at .05. We calculated the effect size with the formula r = z/√(n1 + n2). We calculated Pearson correlation coefficients and the bilateral P values for the comparisons of the different dimensions assessed with Behavior Rating Inventory of Executive Function, Second Edition (BRIEF2), both in the parent form and the teacher form, in the cognitive dimension “executive functions”. We consider correlations with a raw coefficient equal to or greater than .4 statistically significant. Statistical significance was defined as a two-tailed P value of less than .05. We assessed the association between qualitative variables by means of the Pearson χ2 test or the Fisher exact test (2 × 2). The statistical analysis was carried out with the software package SPSS Statistics, version 27.
The study was evaluated and approved by the Ethics Committee of Research with Medicines of our hospital.
ResultsThe ADHD group included 24 patients aged 6–15 years with a mean age of 10.24 years (SD, 2.81). In this group, 13 patients were male (54%) and 11 female (46%). This group was divided into 2 subgroups: inattentive-type ADHD, with 13 patients, and combined-type ADHD, with 11 patients. None of the patients were classified as hyperactive type. In the inattentive group, the mean age was 11.64 years (SD, 2.60) and 7 patients were male (64%) and 4 female (36%). In the combined ADHD subgroup, the mean age was 9.05 years (SD, 2.48) and 6 patients were male (46%) and 7 female (54%). In addition, there was a control group of neurotypical patients without ADHD, comprised of 24 patients aged 7–15 years with a mean age of 11.23 years (SD, 2.74). In the control group, 16 patients were male (67%) and 8 female (33%).
More than half of the patients in the ADHD group (58%) had associated learning disorders. Eight of the 11 patients in the inattentive ADHD subgroup and 6 of the 13 patients in the combined ADHD subgroup had associated learning disorders, and the difference in the prevalence of associated learning disorders between the two subgroups was not statistically significant (Table 2).
Age, sex and presence of associated learning disorders in the groups under study.
| ADHD | Control without ADHD | Inattentive ADHD | Combined ADHD | |
|---|---|---|---|---|
| n | 24 | 24 | 11 | 13 |
| Female | 11 | 8 | 4 | 7 |
| Male | 13 | 16 | 7 | 6 |
| Minimum age | 6.41 | 7.42 | 6.41 | 6.75 |
| Maximum age | 15.00 | 15.75 | 15 | 13.66 |
| Mean age | 10.24 | 11.23 | 11.64 | 9.05 |
| Median age | 9.66 | 10.62 | 12.00 | 8.25 |
| Age SD | 2.81 | 2.74 | 2.60 | 2.48 |
| Learning disorder | 14 (58%) | 0 | 8 (73%) | 6 (46%) |
ADHD, attention-deficit hyperactivity disorder; SD, standard deviation.
When it came to the distribution of the ADHD and control groups, we did not find significant differences in age (U = 224.000; P = .187) or sex (χ2 [1, N = 48] = 48.000; P = .314). We also found no significant differences between the inattentive ADHD and combined ADHD subgroups in either sex (χ2 [1, N = 24] = .734; P = .392) or the frequency of associated learning disorders (χ2 [1, N = 14] = 1.731; P = .188), although we did find a difference in age (U = 33.500; P = .026), as the evaluation was performed at an earlier age in the combined ADHD subgroup (mean, 9.05; SD, 2.48) compared to the inattentive ADHD subgroup (mean, 11.64; SD, 2.60).
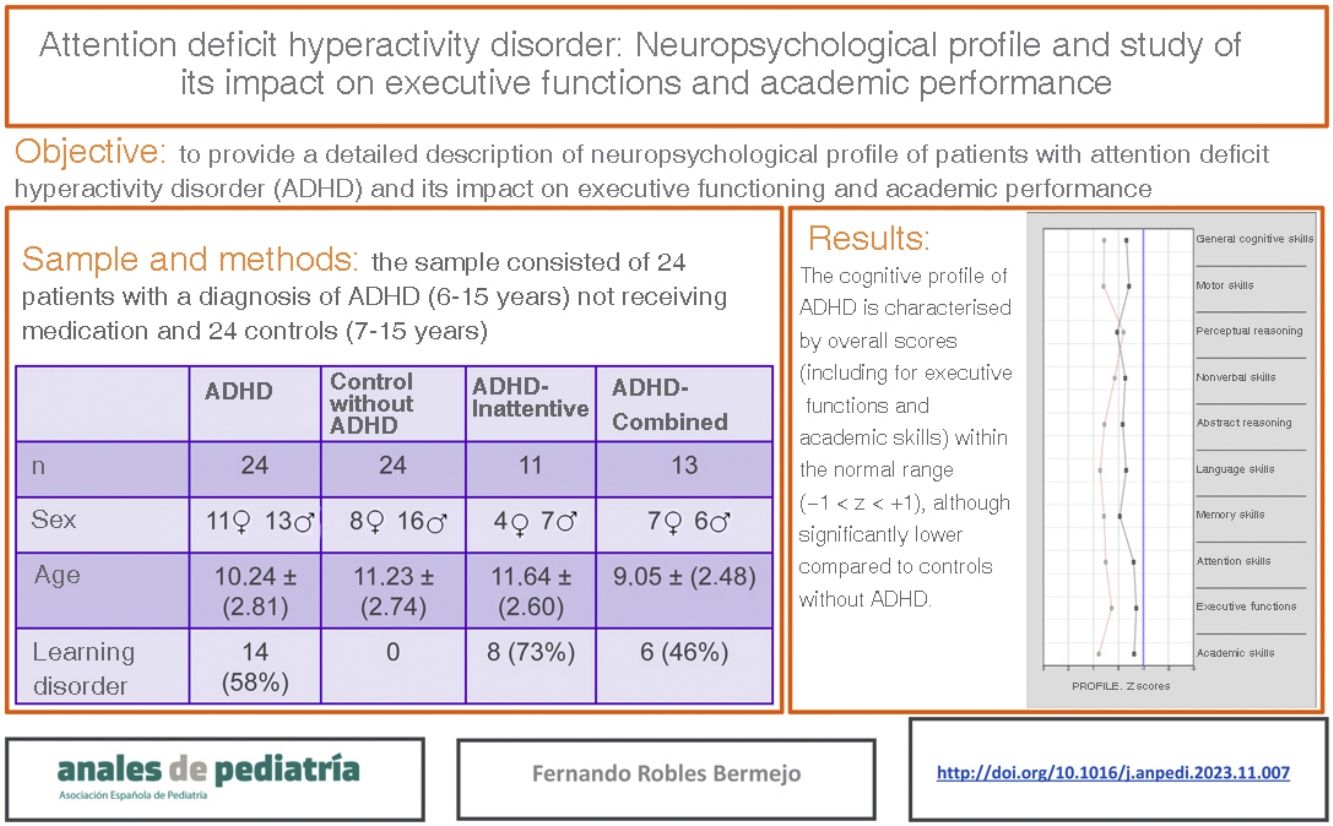
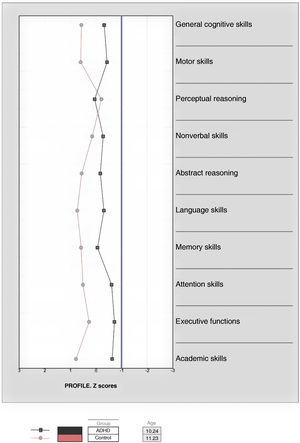
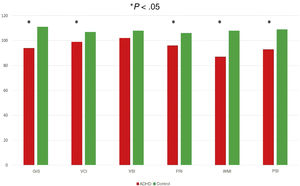
In Fig. 1, it is apparent that patients in the ADHD group had significantly lower scores compared to the neurotypical control group (Table 3) in every cognitive domain (general cognitive skills, measured by the general intelligence score [of which the breakdown by index can be found in Fig. 2], motor skills, nonverbal skills, abstract reasoning, language skills, memory skills, attention skills, executive functions and academic skills), with the exception of perceptual reasoning (U = 203.000; P = .180). Table 4 summarises the results of the post hoc tests analysing the variables that were significant in the previous comparisons, showing that for most, the effect size was moderate or large. We did not find statistically significant differences between the inattentive and combined ADHD subgroups (Fig. 3).
Descriptive statistics for the cognitive domains of the ADHD and control groups.
| VD | Group | n | Median | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|---|---|---|
| General cognitive skills | ADHDControl | 2424 | −.32.58 | −.32.57 | .43.48 | −.97−.24 | .981.47 |
| Motor skills | ADHDControl | 2424 | −.59.84 | −.43.60 | .60.79 | −1.57−.93 | .842.25 |
| Perceptual reasoning | ADHDControl | 2224 | .01−.16 | .05.21 | .64.46 | −1.39−1.16 | 1.66.57 |
| Nonverbal skills | ADHDControl | 2424 | −.10.17 | −.28.15 | .74.38 | −2.26−.78 | 1.121.06 |
| Abstract reasoning | ADHDControl | 2424 | −.41.58 | −.17.56 | .55.69 | −.83−1 | 11.67 |
| Language skills | ADHDControl | 2424 | −.35.70 | −.31.73 | .59.62 | −1.2−.71 | 12.01 |
| Memory skills | ADHDControl | 2424 | −.11.61 | −.06.58 | .63.49 | −1.65−.60 | 1.041.48 |
| Attention skills | ADHDControl | 2424 | −.66.44 | −.61.51 | .39.68 | −1.66−.67 | 01.78 |
| Executive functions | ADHDControl | 2424 | −.70.47 | −.72.27 | .53.72 | −1.84−1.57 | .201.47 |
| Academic skills | ADHDControl | 2324 | −.59.79 | −.63.78 | .71.44 | −1.95−.05 | .571.47 |
ADHD, attention-deficit hyperactivity disorder.
Total intelligence score and other overall scores in the ADHD and control groups.
We found statistically significant differences (P < .01) with a moderate to large effect size (r > .584) in TIS, VCI, FRI, WMI e PSI between the ADHD group and the neurotypical control group.
GIS, general intelligence score; VCI, verbal comprehension index; VSI, visual-spatial index; FRI, fluid reasoning index; WMI, working memory index; PSI, processing speed index
Post hoc comparisons of the cognitive domains in the ADHD group and the control group without ADHD.
| Mann-Whitney U | Wilcoxon W | z | P | r | |
|---|---|---|---|---|---|
| General cognitive skills | |||||
| Motor skills | 92.500 | 392.500 | −4.031 | <.01 | .582 |
| Perceptual reasoning | 203.000 | 503.000 | −1.342 | .180 | |
| Nonverbal skills | 174.000 | 474.000 | −2.351 | .019 | .339 |
| Abstract reasoning | 115.000 | 415.000 | −3.573 | <.01 | .516 |
| Language skills | 67.000 | 367.000 | −4.557 | <.01 | .658 |
| Memory skills | 119.000 | 419.000 | −3.845 | <.01 | .503 |
| Attention skills | 43.500 | 343.500 | −5.046 | <.01 | .728 |
| Executive functions | 76.000 | 376.000 | −4.371 | <.01 | .631 |
| Academic skills | 19.500 | 295.500 | −5.459 | <.01 | .796 |
ADHD, attention-deficit hyperactivity disorder.
Teachers reported difficulties more frequently in male compared to female patients: inhibit (U = 11.000; P = .030; r = .543), shift (U = 11.000; P = .030; r = .544); initiate (U = 6.000; P = .013; r = .639), task-monitor (U = 7.500; P = .021; r = .594); organization of materials (U = 6.000; P = .013; r = .643) and emotional control (U = 11.500; P = .034; r = .531) scale scores and global executive composite (U = 11.500; P = .034; r = .530). We did not find statistically significant or sufficiently large correlations (≥.4) between the BRIEF2 scales and the results for the executive function domain.
DiscussionThe findings of our study show that the mean general intelligence score (GIS) in the ADHD group was within the normal range (z between –1 and 1, which is equivalent to an IQ score from 85 to 115), and was significantly lower compared to the mean score in the control group without ADHD. This was consistent with the existing evidence, which shows that individuals with ADHD have a GIS in the normal range but lower compared to neurotypical peers.27 In our study, the GIS in the ADHD group was 94 compared to 111 in the control group, so the results were consistent with the previous literature. As regards the other indices, those in which the scores in the ADHD group were lower were the working memory index (WMI = 87) and the processing speed index (PSI = 93), followed by the general intelligence score (GIS = 94), fluid reasoning index (FRI = 96) visual-spatial index (VSI = 102). In every case, the scores were also within the normal range (z between –1 and 1) and significantly lower compared to the scores in the control group without ADHD. Studies that have assessed neuropsychological variables have consistently found that individuals with ADHD scored lower, although within the normal range, not only in general intelligence but also in the rest of the cognitive indices, especially the WMI28 and the PSI.29 Our findings also seem to fit the described trend.
One of the cognitive domains that has been studied most extensively in ADHD and most strongly correlated with the difficulties experienced by these patients are EFs, in addition to their association with other cognitive functions.30 In our study, executive function was one of the cognitive domains in which patients with ADHD scored significantly lower compared to controls. Overall, scores were within the normal range (z entre –1 y 1), but significantly lower compared to the control group without ADHD. The assessment of EFs is heterogeneous, with application of various tests and indicators of functioning.31 Numerous authors, while referring to different functions (cognitive flexibility, working memory, inhibition…), describe difficulties in this domain,30,32 which our findings were not consistent with. In addition to the identified abnormalities in themselves and the resulting executive functioning problems, the impact of these problems can affect other functions and skills, hindering the academic performance and social development of the heir detection and treatment are essential in order to facilitate adequate coping and functioning in everyday life.33,34
In our study, more than half of the patients (58%) in the ADHD group had learning comorbidities. The school setting and academic performance constitute one of the areas that can be most affected by ADHD. The literature shows that ADHD is frequently associated with other disorders, including specific learning disorders.35 Our findings were consistent with those of other authors who have reported a higher frequency of learning disorders in individuals with ADHD compared to the general population at every developmental stage,36 the detection and treatment of which are of vital importance for adequate academic performance and social adjustment.37,38
Behaviour assessment questionnaires are widely used in research and clinical practice to estimate the level of executive functioning of individuals and have proven very useful for diagnosis of executive function disorders and to differentiate individuals with ADHD from neurotypical individuals.39 It is worth highlighting that in our study, it was teachers, rather than parents, who tended to report more executive functioning problems in male patients. This has been consistently described in the literature, as male individuals tend to exhibit more externalising symptoms compared to female individuals, whose symptoms can be underestimated,5 which can explain the observed differences. This aspect warns us of potential biases in behavioural questionnaires that could result in overdiagnosis of ADHD in male individuals and underdiagnosis in female individuals.40 The neuropsychological assessment can provide an individualised and finetuned clinical picture of women with ADHD, facilitating the detection, diagnosis and treatment of the disorder.
There are several limitations to this study, such as the small sample size, including the sizes of the ADHD and neurotypical control groups, which led us to use nonparametric tests, which carries its own limitations in the analysis and reduces the statistical power. Not including patients receiving pharmacological treatment contributed to reducing the sample size considerably and also hinders the longitudinal follow-up, as many patients will eventually receive medication. In future research, it would be interesting to make a more detailed analysis in different ADHD subtypes and assess the differences between patients receiving pharmacological treatment and unmedicated patients. Similarly, comparison with more than one control groups, including a neurotypical control group and a group with learning disorders, could improve our understanding and therefore our detection tools and treatment strategies. Lastly, it would be useful to obtain more information about the samples, for instance, on socioeconomic characteristics, as these factors can affect diagnosis as well as the experience of living with ADHD.
ConclusionOverall, the cognitive performance of patients with ADHD was poorer compared to the neurotypical group. Attention-deficit hyperactivity disorder has a considerable impact on executive functioning and academic skills, and in our sample, 58% of patients with ADHD had associated learning disorders. Behavioural assessment questionnaires allow evaluation in different settings (school and home) and provide very valuable information about the functioning of the child, but the information obtained through them may be biased, as male subjects tend to exhibit more externalising symptoms. An exhaustive neuropsychological assessment of general cognitive functioning is a useful tool that can facilitate the diagnosis of ADHD and adequate management of patients and families based on their particular characteristics and needs.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.