Lower respiratory tract infections (LRTIs), including bronchiolitis, community-acquired pneumonia, wheezing bronchitis and other unspecified infections, are the leading cause of hospital admission in children. Most have a viral etiology and do not require antibiotic treatment.1 However, unnecessary use of antibiotherapy is frequent in these patients.2 Such inappropriate prescribing may stem from circumstances related to the disease, the patients or the health care setting (severity, comorbidities, available resources), but it may also result from clinical practices associated with overtesting and overtreatment.3 The aim of our study was to measure the frequency of antibiotic prescribing in children admitted to hospital with viral LRTIs and explore factors associated with this treatment.
We conducted a study in a cohort of children (aged 21 days-14 years) who were admitted to hospital (between January 2019 and January 2023) from the emergency department in a tertiary care hospital, with a primary diagnosis of LRTI, who did not require intensive care (although may have needed noninvasive ventilation) and with a positive results in a polymerase chain reaction (PCR) test for detection of respiratory viruses (influenza, respiratory syncytial virus [RSV], adenovirus, bocavirus, coronavirus [NL63, 229E, OC43], enterovirus, parainfluenza, metapneumovirus, rhinovirus and, since 2020, SARS-CoV-2). We excluded patients who only tested positive for SARS-CoV-2, with complex chronic conditions, with a concurrent diagnosis of infection of probable bacterial etiology or with positive results in any bacteriological tests on a biological sample. In our hospital, early PCR results (firs24 h) are only available for influenza, RSV and SARS-CoV-2 PCR tests. We collected data on clinical outcomes, diagnostic tests and treatment from the health records.
The association of antibiotherapy with variables related to disease severity and the use of diagnostic tests was assessed by means of the χ2 or the Mann–Whitney U test. The variables found to be significantly associated with antibiotherapy in the bivariate analysis (P < .05) were included in a multivariate logistic regression model. We then carried out a sensitivity analysis, fitting the multivariate model in specific subsets of the sample.
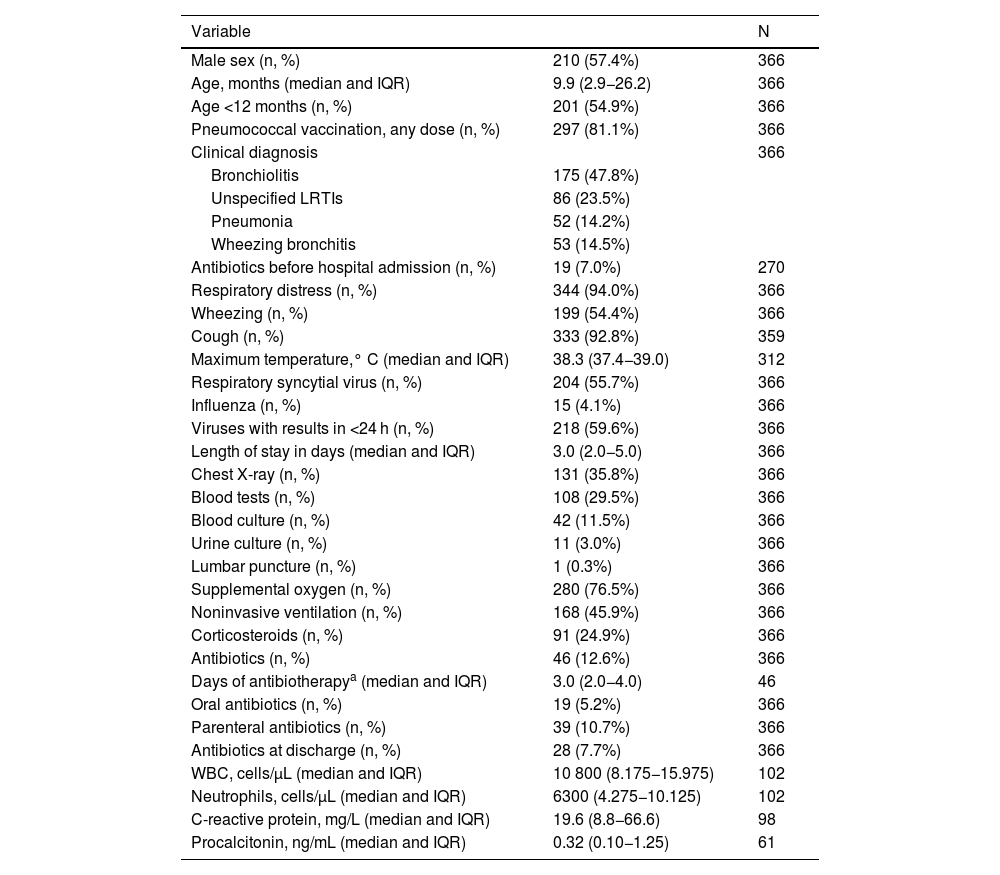
Of the 490 children admitted due to LRTI, we excluded 109 because either no virus or only SARS-CoV-2 had been detected in testing, 6 for requiring intensive care, 2 due to detection of bacterial coinfection and 7 due to having chronic complex conditions, so the final sample included 366 patients. Table 1 summarizes the characteristics of the sample. All the included patients had a positive PCR test result, most frequently for RSV (41.7%) or rhinovirus (21.0%).
Sample characteristics.
| Variable | N | |
|---|---|---|
| Male sex (n, %) | 210 (57.4%) | 366 |
| Age, months (median and IQR) | 9.9 (2.9−26.2) | 366 |
| Age <12 months (n, %) | 201 (54.9%) | 366 |
| Pneumococcal vaccination, any dose (n, %) | 297 (81.1%) | 366 |
| Clinical diagnosis | 366 | |
| Bronchiolitis | 175 (47.8%) | |
| Unspecified LRTIs | 86 (23.5%) | |
| Pneumonia | 52 (14.2%) | |
| Wheezing bronchitis | 53 (14.5%) | |
| Antibiotics before hospital admission (n, %) | 19 (7.0%) | 270 |
| Respiratory distress (n, %) | 344 (94.0%) | 366 |
| Wheezing (n, %) | 199 (54.4%) | 366 |
| Cough (n, %) | 333 (92.8%) | 359 |
| Maximum temperature,° C (median and IQR) | 38.3 (37.4−39.0) | 312 |
| Respiratory syncytial virus (n, %) | 204 (55.7%) | 366 |
| Influenza (n, %) | 15 (4.1%) | 366 |
| Viruses with results in <24 h (n, %) | 218 (59.6%) | 366 |
| Length of stay in days (median and IQR) | 3.0 (2.0−5.0) | 366 |
| Chest X-ray (n, %) | 131 (35.8%) | 366 |
| Blood tests (n, %) | 108 (29.5%) | 366 |
| Blood culture (n, %) | 42 (11.5%) | 366 |
| Urine culture (n, %) | 11 (3.0%) | 366 |
| Lumbar puncture (n, %) | 1 (0.3%) | 366 |
| Supplemental oxygen (n, %) | 280 (76.5%) | 366 |
| Noninvasive ventilation (n, %) | 168 (45.9%) | 366 |
| Corticosteroids (n, %) | 91 (24.9%) | 366 |
| Antibiotics (n, %) | 46 (12.6%) | 366 |
| Days of antibiotherapya (median and IQR) | 3.0 (2.0−4.0) | 46 |
| Oral antibiotics (n, %) | 19 (5.2%) | 366 |
| Parenteral antibiotics (n, %) | 39 (10.7%) | 366 |
| Antibiotics at discharge (n, %) | 28 (7.7%) | 366 |
| WBC, cells/μL (median and IQR) | 10 800 (8.175−15.975) | 102 |
| Neutrophils, cells/μL (median and IQR) | 6300 (4.275−10.125) | 102 |
| C-reactive protein, mg/L (median and IQR) | 19.6 (8.8−66.6) | 98 |
| Procalcitonin, ng/mL (median and IQR) | 0.32 (0.10−1.25) | 61 |
IQR, interquartile range; LRTI, lower respiratory tract infection; WBC, white blood cells.
Forty-six of the patients (12.6%) received antibiotherapy. Most of the prescribed antibiotics (69.6%) were aminopenicillins, but 23.9% of patients received a third-generation cephalosporin. Antibiotherapy was used in 4.0% of cases of bronchiolitis, 5.7% of cases of wheezing bronchitis, 12.8% of cases of unspecified LRTI and 48.1% of cases of pneumonia. In 26 of these 46 patients (60.9%), antibiotherapy continued after discharge, but with a lower frequency in infections with early diagnostic confirmation (RSV and influenza): 45.8% vs. 77.3% (P = .038).
In the bivariate analysis, the variables significantly associated with the use of antibiotherapy were older age, higher temperature, previous vaccination against pneumococcus, absence of dyspnea, initiation of antibiotherapy prior to hospital admission, diagnosis of pneumonia and performance of blood tests, chest X-ray, urine culture or blood culture (Appendix A, Supplemental material, Tables 1S and 2S). In the subset of patients with blood tests, the neutrophil count, C-reactive protein and procalcitonin levels were higher in the group who received antibiotics. In the subset of patients with a chest radiograph, consolidation was associated with a greater frequency of antibiotherapy (75.0%) compared to normal radiographic appearance (11.1%) or other infiltrates (16.0%) (P < .001).
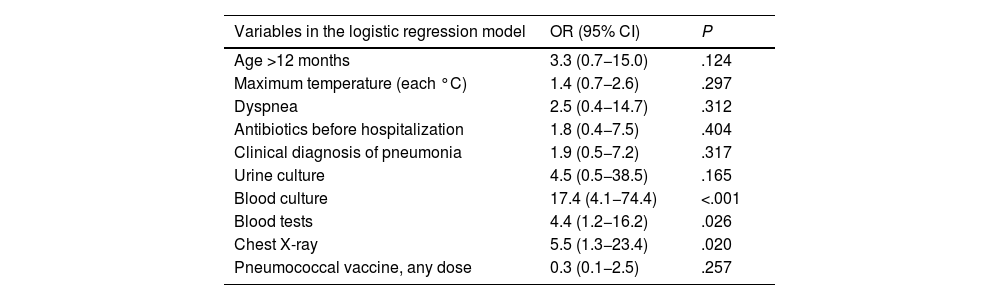
In the multivariate analysis (Table 2), the only variables associated with antibiotherapy were the performance of chest X-ray, blood tests or blood culture. The sensitivity analysis (Appendix A, Supplemental material, Table 3S) confirmed these results. In another regression model, test results were not significantly associated with antibiotherapy (Appendix A, Supplemental material, Table 4S).
Multivariate analysis.
| Variables in the logistic regression model | OR (95% CI) | P |
|---|---|---|
| Age >12 months | 3.3 (0.7−15.0) | .124 |
| Maximum temperature (each °C) | 1.4 (0.7−2.6) | .297 |
| Dyspnea | 2.5 (0.4−14.7) | .312 |
| Antibiotics before hospitalization | 1.8 (0.4−7.5) | .404 |
| Clinical diagnosis of pneumonia | 1.9 (0.5−7.2) | .317 |
| Urine culture | 4.5 (0.5−38.5) | .165 |
| Blood culture | 17.4 (4.1−74.4) | <.001 |
| Blood tests | 4.4 (1.2−16.2) | .026 |
| Chest X-ray | 5.5 (1.3−23.4) | .020 |
| Pneumococcal vaccine, any dose | 0.3 (0.1−2.5) | .257 |
CI, confidence interval; OR, odds ratio.
In conclusion, one in eight previously healthy children admitted to hospital with a viral LRTI and who did not require intensive care received antibiotherapy. Although this percentage was lower compared to the proportions reported in recent studies (25%–75%),4–6 it is important to consider the narrow criteria applied in sample selection, as we excluded patients with potential bacterial coinfection (e.g., with otitis media) and patients with risk conditions.
The factors associated with the use of antibiotherapy were not severity indicators (e.g., need of supplemental oxygen or noninvasive ventilation, body temperature, respiratory symptoms) or health care-related circumstances (e.g., antibiotherapy initiated prior to admission, delayed turnaround of PCR test results for respiratory viruses). In contrast with other studies,5 we did not identify specific blood test or imaging findings independently associated with antibiotherapy. The factors associated with the use of antibiotherapy were the ordering of tests like the chest radiograph, blood tests or blood culture. Our findings seem to indicate that unnecessary antibiotherapy is, above all, the result of a clinical approach characterized by a combination of overtesting and overtreatment.