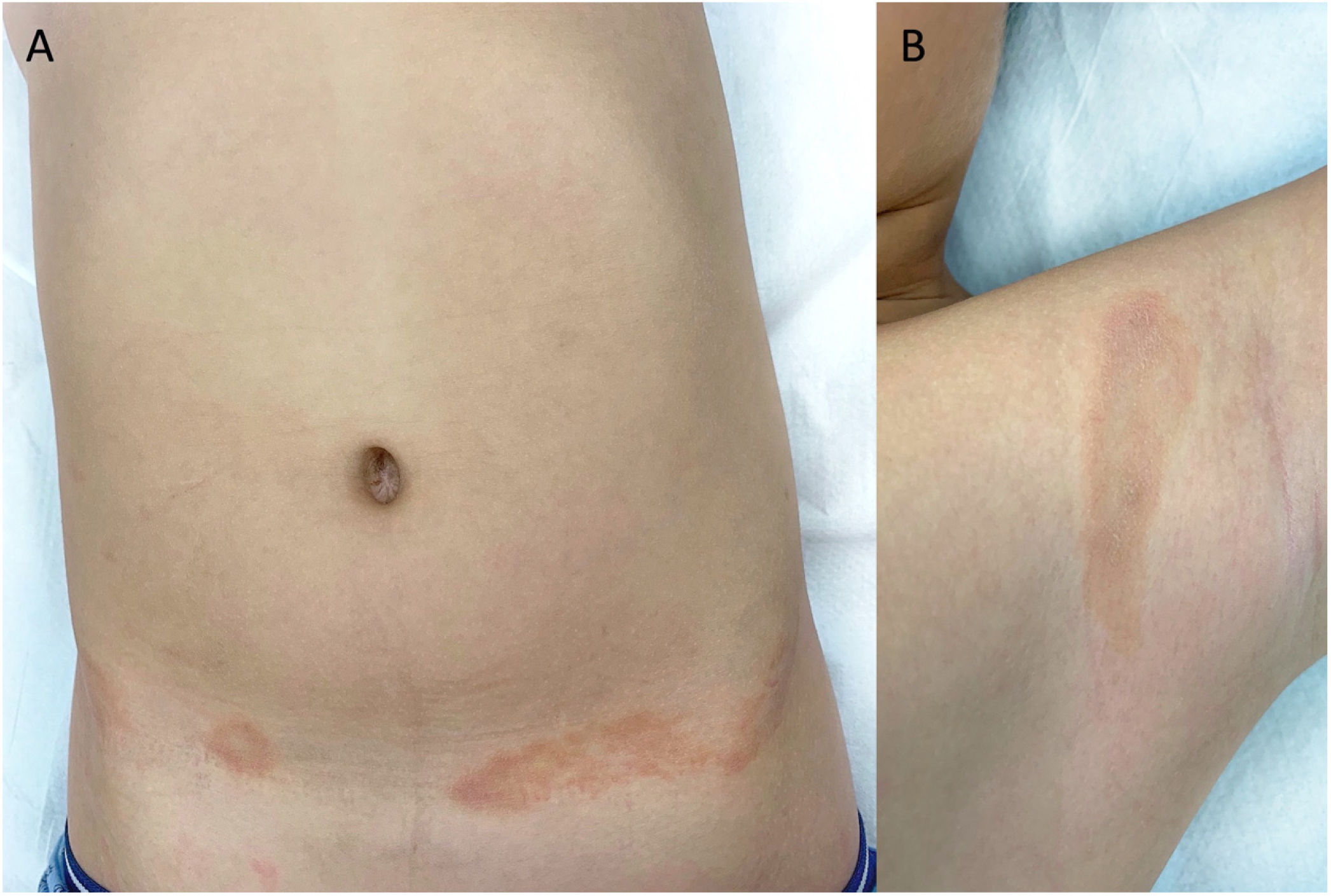
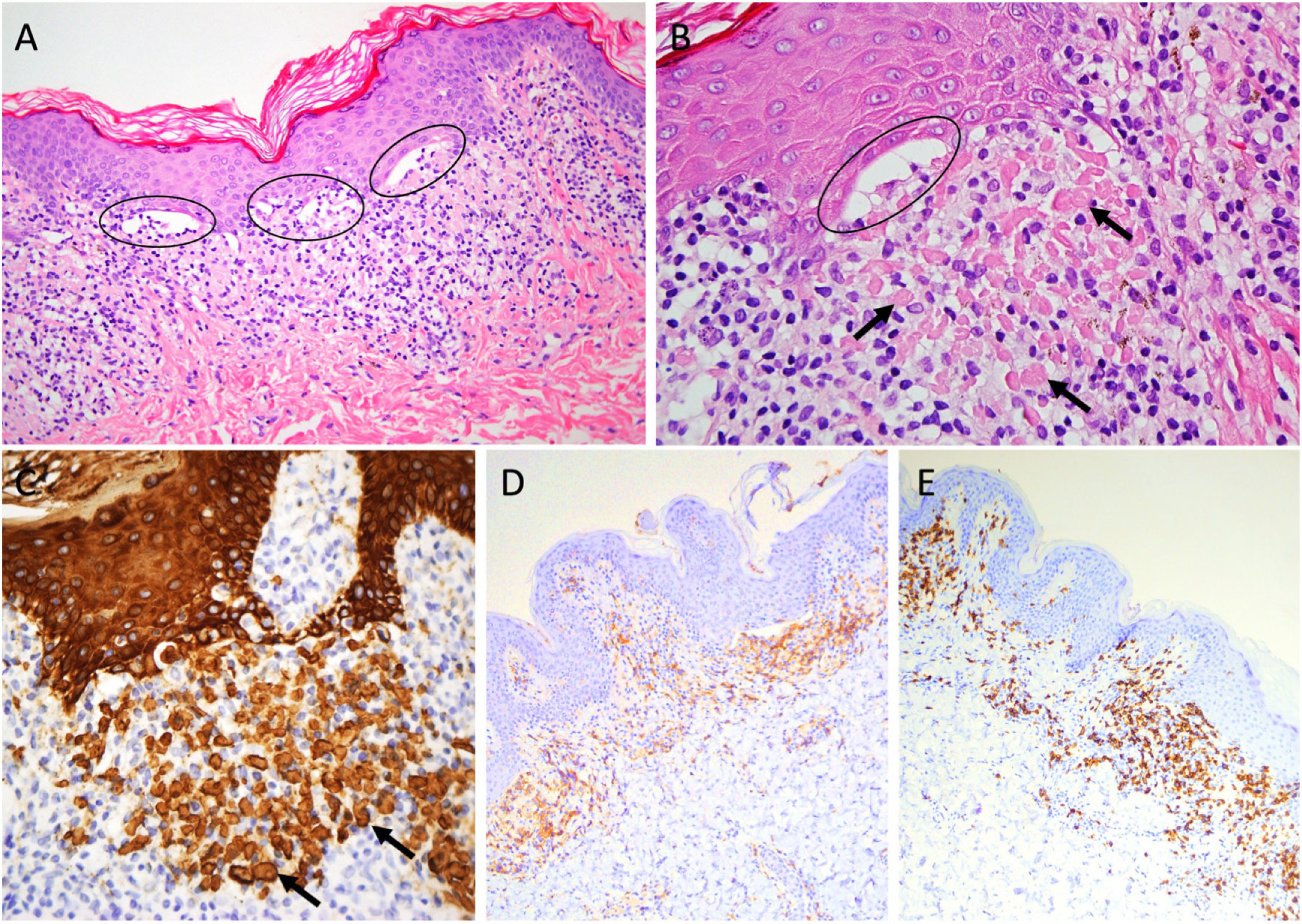
A healthy boy aged 8 years presented with asymptomatic annular lesions with onset one year prior. The physical examination revealed several annular plaques measuring 3–8 cm in diameter, with a brownish erythematous border and a hypopigmented centre (Fig. 1). The lesions were located in the groin, flanks and axillae. The examination of a skin biopsy specimen detected a lymphocytic in the papillary, with changes in the vacuoles of the basal cell layer and apoptotic keratinocytes (colloid bodies), located at the tip of the epidermal ridges, giving them a square appearance (Fig. 2A–C). Immunohistochemical staining evinced a predominance of CD4+ cells and especially CD8+ cells (Fig. 2D–E). Molecular testing revealed a polyclonal T-cell population (T cell receptor analysis). The patient received a diagnosis of annular lichenoid dermatitis of youth and was treated with topical methylprednisolone aceponate cream and tacrolimus 0.1% ointment. At 6 months of follow-up, the lesions had fully regressed.
Band-like lymphocytic infiltration in the papillary dermis, vacuolar alterations in the basal cell layer (ellipses) and necrotic keratinocytes (arrows) at the tip of the epidermal ridges. Haematoxylin-eosin staining: (A) ×20 (B) ×40. Immunohistochemistry: (C) Cytokeratin AE1/AE3, (D) CD4+, (E) CD8+.
Annular lichenoid dermatitis of youth (ALDY) is an infrequent lichenoid dermatosis of unknown aetiology. Since it was first described in 2003, 64 cases have been reported, most in children and adolescents in the Mediterranean region.1,2 Clinically it manifests in the form of spots and plaques with a brownish-red colour with a hypopigmented centre predominantly found in the abdomen, flanks and groin.1 The differential diagnosis includes morphea, inflammatory vitiligo, annular erythema, tinea corporis, purpura annularis telangiectodes of Majocchi and, above all, hypopigmented mycosis fungoides (MF) (cutaneous T-cell lymphoma).1–3 The clinical and histological features that help differentiate ALDY from MF are: annular morphology of the lesions, absence of desquamation, atrophy and induration, distribution in cutaneous folds and sparing the distal portion of the extremities, quadrangular epidermal ridges with necrotic keratinocytes at the tips, absence of epidermotropism and a polyclonal infiltrate.2 Although it is a benign disease, it has a chronic course with frequent recurrences. Regression of the lesions, either spontaneous or following treatment with topical steroids, calcineurin inhibitors or phototherapy has been described.1–3 Follow-up at regular intervals is recommended due to its clinical and histological similarities with MF.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.