A patient aged 20 months with no relevant medical history was brought to the emergency department for assessment of skin lesions with onset 15 days prior. The examination (Figs. 1 and 2) revealed the presence of tense vesicles and blisters clustered around macules or crusts with an arrangement resembling a rosette. The patient was afebrile and there was no mucosal involvement. No exposure to pharmaceuticals or recent vaccination reported.
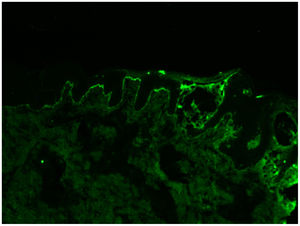
Linear immunoglobulin A bullous dermatosis was suspected. The findings of the histological examination and direct immunofluorescence (DIF) confirmed the diagnosis: subepidermal bullae and visualization on DIF of continuous linear deposition of IgA at the dermoepidermal junction (Fig. 3).
Treatment was initiated with prednisone, adding dapsone after 15 days at a dose of 1mg/kg/day with tapering off of prednisone until its discontinuation. The levels of glucose-6-phosphate dehydrogenase remained in the normal range, and the patient had a favourable outcome.
Linear immunoglobulin A bullous is an acquired blistering dermatosis of an autoimmune aetiology,1 although there can be cases induced by drugs. The main diseases that need to be considered in the differential diagnosis are dermatitis herpetiformis, bullous pemphigoid, lichen planus and toxic epidermal necrolysis.1–3 It is important for paediatricians to know how to recognise the typical rosette or ‘cluster of jewels’ pattern, although the pathognomonic feature is the linear deposit of IgA along the basal membrane. Dapsone is the treatment of choice, and the course of disease is characterised by exacerbation and remission periods until its full resolution.1
FundingThis research did not receive any external funding.