Breastfeeding (BF) has a considerable impact in terms of reducing infant and maternal mortality, with a dose-effect relationship based on its duration.1 The Baby-Friendly Hospital Initiative (BFHI, or IHAN in Spain) proposes a series of strategies to improve BF rates. One of the most important ones is monitoring the prevalence of BF at different timepoints in the life of the infant.2 However, the data on BF rates for different geographical areas is limited or outdated.3 In this context, the Region of Murcia is developing a First 1000 days programme that includes surveillance of BF indicators and related practices.
To this end, we conducted an observational study in the newborns and infants managed in every public health care facility of the public health care system of the region of Murcia (6 hospitals providing paediatric care and 85 primary care centres grouped into 9 health care areas). The study period spanned 12 months (January to December 2023). We excluded infants who required admission to the neonatal unit during the maternal hospital stay in the postpartum period and cases for which we were unable to retrieve the records. We analysed BF rates through age 24 months and indicators with a potential impact on BF rates. We collected data through the standard forms of the primary care and hospital electronic health record systems of the Region of Murcia.4
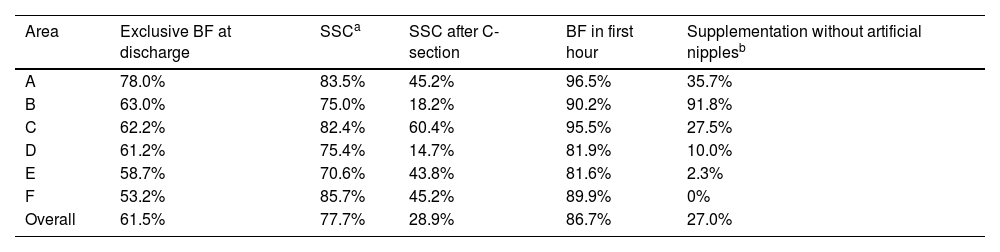
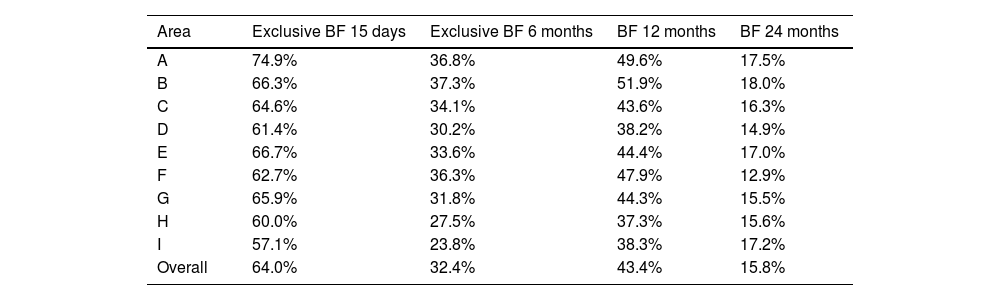
We collected data for 97.8% of infants (n=10 323) at the time of hospital discharge, 99.2% at 15 days post birth (n=13 825), 83.4% at 6 months (n=11 574) and 86.2% and 64.4% at 12 and 24 months, respectively (n=12 742 and n=9516). We found that 61.5% were exclusively breastfed through discharge from the maternity ward and 95.7% had breastfed at some point during this time interval. The frequency of strict adherence to skin-to-skin contact recommendations was 77.7%, and BF was initiated within an hour of birth in 86.7% of infants. Breastfeeding rates declined progressively: 92.9% at 15 days (exclusive BF, 64%), 58.3% at 6 months (exclusive BF, 32.4%), 43.4% at 12 months and 15.8% at 24 months. The exclusive BF rate was 64.0% at 15 days and 32.4% at 6 months. Tables 1 and 2 expand on this information and break it down by health care area.
Indicators of breastfeeding during the hospital stay.
| Area | Exclusive BF at discharge | SSCa | SSC after C-section | BF in first hour | Supplementation without artificial nipplesb |
|---|---|---|---|---|---|
| A | 78.0% | 83.5% | 45.2% | 96.5% | 35.7% |
| B | 63.0% | 75.0% | 18.2% | 90.2% | 91.8% |
| C | 62.2% | 82.4% | 60.4% | 95.5% | 27.5% |
| D | 61.2% | 75.4% | 14.7% | 81.9% | 10.0% |
| E | 58.7% | 70.6% | 43.8% | 81.6% | 2.3% |
| F | 53.2% | 85.7% | 45.2% | 89.9% | 0% |
| Overall | 61.5% | 77.7% | 28.9% | 86.7% | 27.0% |
BF, breastfeeding; SSC, skin-to-skin contact.
Breastfeeding rates after hospital discharge.
| Area | Exclusive BF 15 days | Exclusive BF 6 months | BF 12 months | BF 24 months |
|---|---|---|---|---|
| A | 74.9% | 36.8% | 49.6% | 17.5% |
| B | 66.3% | 37.3% | 51.9% | 18.0% |
| C | 64.6% | 34.1% | 43.6% | 16.3% |
| D | 61.4% | 30.2% | 38.2% | 14.9% |
| E | 66.7% | 33.6% | 44.4% | 17.0% |
| F | 62.7% | 36.3% | 47.9% | 12.9% |
| G | 65.9% | 31.8% | 44.3% | 15.5% |
| H | 60.0% | 27.5% | 37.3% | 15.6% |
| I | 57.1% | 23.8% | 38.3% | 17.2% |
| Overall | 64.0% | 32.4% | 43.4% | 15.8% |
BF, breastfeeding.
Strategies aimed at improving the prevalence of BF, such as skin-to-skin contact and the timing of the first placement of the infant at the breast5 must be monitored to assess their impact on health promotion in any given geographical area. The First 1000 days programme in Murcia allows standardised and ongoing surveillance of these variables. The World Health Organization (WHO) has established increasing the rate of exclusive BF at 6 months to 50% for its 2025 development agenda and to 70% for its 2030 development agenda. The rates in our region are far from these targets, which is consistent with the data reported in most regions in Spain6 and other developed countries.3 There is a dearth of data on the interventions related to BF, despite the evidence on their impact on BF, and there is significant variability based on the care that is routinely delivered in each centre.
The main limitation of our study is the risk of inaccuracy in the documentation of the outcomes of interest on the part of health care professionals. In addition, the loss to follow-up at 24 months was substantially larger compared to all other time points, which limits the generalizability of the results for this age group. Obtaining real-life evidence for each region and health care areas in relation to the aspects discussed above helps gain a more up-to-date perspective of the current reality in Spain. We believe that the implementation of the universal surveillance model of the public health administration of Murcia could contribute to the introduction of similar strategies in other regions.
We thank all the health care professionals that collaborate with the First 1000 days care programme of the health care administration of the Region of Murcia.