A previously healthy girl aged 2 years exhibited gradual impairment in her walking ability over a one-month period, which was initially interpreted as transient synovitis of the hip. Progressive muscle weakness ensued, culminating in flaccid paraplegia, with absence of reflexes in the lower limbs, sensory changes below the D10 level and urinary and faecal retention. There was no recent history of trauma or infection. A contrast-enhanced magnetic resonance scan of the spine revealed an intramedullary arteriovenous malformation at D10 (Fig. 1). There was a paternal family history of hereditary haemorrhagic telangiectasia (HHT). A spinal angiogram was performed, but endovascular treatment attempts were unsuccessful. The decision was made to delay treatment, to be delivered at a specialized hospital. The patient underwent a course of steroid therapy combined with physical therapy and exhibited some marked motor improvements, gaining the ability to sit without imbalance and get on her knees and crawl. After three months, the patient underwent endovascular treatment, which was successful (Fig. 2). Subsequent follow-up evinced recovery of independent ambulation, spontaneous urinary function and regular bowel movements. Genetic testing confirmed the diagnosis of HHT, with detection of a heterozygous mutation in the endoglin gene (c.777_778dup(p.Ser260Cysfs*100)).
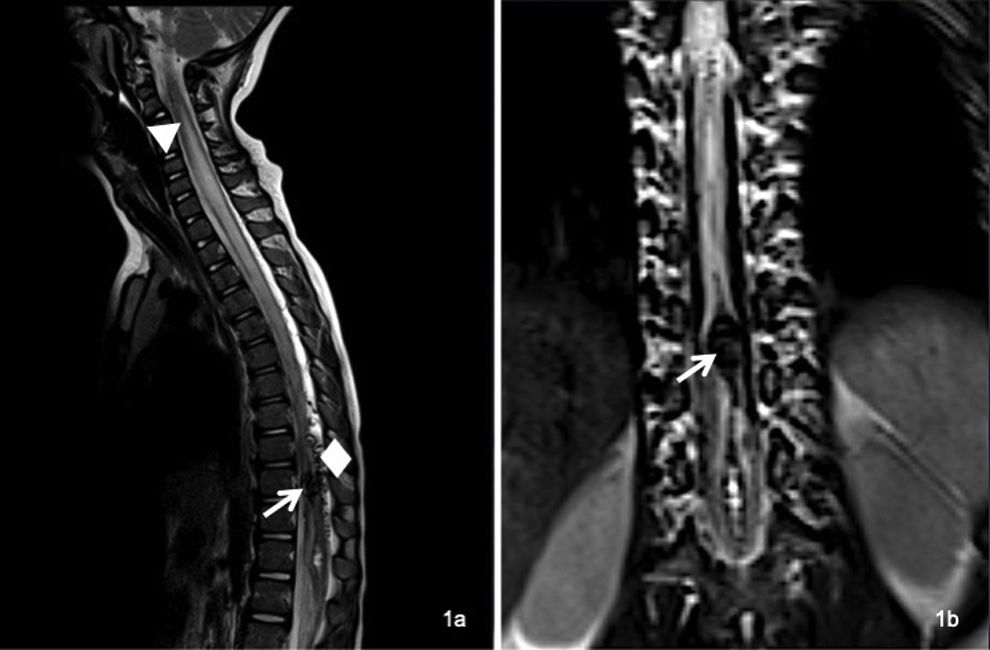
Magnetic resonance imaging of the spine revealing an intramedullary arteriovenous malformation at the D10 level (arrow), characterized by venous ectasia and haematomyelia. The haematomyelia appeared hypointense in T2-weighted imaging, extending through the central canal superiorly up to D9 and inferiorly down to the conus medullaris. At the same time, there was extensive intramedullary hyperintensity, visualized up to the level of C2, attributed to venous congestion (triangle), along with dilatation of the posterior perimedullary veins (diamond).
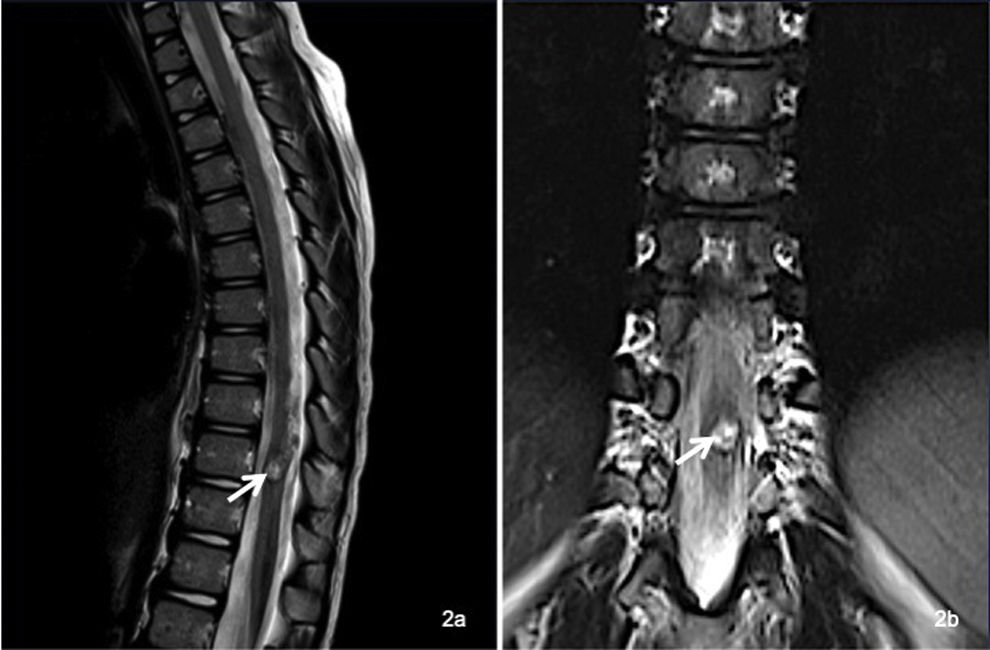
Follow-up imaging after endovascular treatment revealed intra- and perimedullary heterogeneous signal intensity in T2-weighted images at the D10 level, indicating the presence of embolic material and a post-treatment intravascular thrombus (arrow). Residual haemosiderin staining was visualized in the spinal cord, attributed to prior bleeding. There was also evidence of oedema reabsorption, with no evidence of dilation of the posterior perimedullary veins or any other abnormal vascular structures.
This case highlights the importance of a high index of suspicion in children with a family history of HHT, given their susceptibility to develop spinal arteriovenous malformations.1,2
We express our heartfelt gratitude to the Hôpital Necker-Enfants Malades for its invaluable collaboration in the treatment of the patient. The dedication and expertise of the medical team were crucial to the successful outcome of this case.