In January 2019, the Community of Madrid’s Health Department published a guide about the use of antimicrobials in outpatient children. Taking this regional Guide as reference, this study was aimed at estimating the adequacy of the antimicrobial stewardship at discharge from a pediatric Emergency Department (ED). Secondarily, the differences in adequacy according to the diagnosis and the prescriber were studied, and the agreement between this Guide and the protocols of the ED was assessed.
Material and methodsAn observational, descriptive, retrospective study was conducted on patients under 16 years old, with a diagnosis included in the regional Guide who were discharged from a pediatric ED between March of 2018 and February of 2019. Prescription was considered adequate when the indication, the antibiotic and the posology (dosage, dosing interval, length of treatment and route of administration) were correct.
Results165 out of 648 (25,5%) infectious diseases processes analyzed received antimicrobial treatment. In 23 processes treated with antimicrobial, the adequacy could not be evaluated due to the absence of data necessary to assess any aspect of posology. Therapy was considered appropriate in 550/625 processes (88.0%). When antimicrobial treatment was prescribed, 70/142 (49.3%) were appropriate and no statistically significant differences in adequacy were found between prescribers. Posology was the worst handled point of the prescription (26.3%). Tract urinary infection, conjunctivitis and otitis media were the pathologies with the lowest adecuacy (44.4%; 50.0% and 52.2%) and presented the highest discrepancy between the Guide and the center protocols (κ = 0.308; κ = 0.000; κ = 0.586).
ConclusionsThe adequacy of the management of infectious processes to the reference Guide in our pediatric ED was high, but it was below 50% when antimicrobial treatment was required. The degree of adequacy to the local protocols of the center was greater than to the regional Guide. This reveals a discrepancy between the 2 documents that should be analyzed and corrected according to the available scientific evidence.
En enero del 2019 la Consejería de Sanidad de la Comunidad de Madrid publicó una guía acerca del uso de antimicrobianos en niños con tratamiento ambulatorio. El objetivo de este trabajo fue estimar la adecuación de la prescripción de antimicrobianos al alta desde el Servicio de Urgencias Pediátricas (SUP) en pacientes con enfermedades infecciosas, tomando como referencia esta guía regional. Secundariamente, se estudió la variación en la adecuación según el diagnóstico realizado y el facultativo prescriptor, y se valoró la concordancia entre dicha guía y los protocolos del centro.
Material y métodosEstudio observacional, descriptivo y retrospectivo en el que se incluyó a pacientes de 0-16 años con diagnóstico al alta del SUP incluido en la guía regional, entre marzo del 2018 y febrero del 2019. La prescripción se consideró adecuada cuando lo era la indicación, y en su caso, el fármaco elegido, la posología (dosis, intervalo y duración) y la vía de administración.
ResultadosSe obtuvo una muestra de la que se analizaron 648 procesos infecciosos, siendo tratados con antimicrobianos 165 (25,5%). En 23 procesos no pudo evaluarse la adecuación a la guía por ausencia de algún dato posológico de la prescripción de antimicrobiano. El manejo terapéutico fue adecuado globalmente en 550/625 procesos (88,0%). En los procesos tratados con antimicrobiano, la adecuación fue de 70/142 (49,3%), sin encontrarse diferencias estadísticamente significativas entre facultativo prescriptor. El motivo de inadecuación más frecuente fue el error posológico (26,3%). Infección urinaria, conjuntivitis y otitis media aguda fueron las entidades clínicas con peor adherencia (el 44,4, el 50,0 y el 52,2% respectivamente) y en las que existió una mayor discrepancia entre guía y protocolos (κ = 0,308; κ = 0,000; κ = 0,586).
ConclusionesLa adecuación a las guías de referencia del manejo de procesos infecciosos en el SUP de nuestro centro fue elevada, pero fue inferior al 50% cuando se precisó tratamiento antimicrobiano. El grado de adecuación a los protocolos del centro fue mayor que a la guía de la Comunidad de Madrid, revelando una discrepancia entre ambos que debería ser analizada y corregida de acuerdo con la evidencia científica disponible.
Infectious diseases are the underlying cause of a large proportion of the presenting complaints in visits to paediatric emergency departments (PEDs).1–3 Antibiotics are among the most frequently used drug classes, as they are prescribed to up to 15%–20% of managed patients according to several recent studies.1–3 The excessive use of antibiotic agents and their inappropriate prescription in terms of dosage or duration have been associated with an increase in the prevalence of antimicrobial resistance,4–6 changes in the microbiota, an increased frequency of allergies to antimicrobials and an increased risk of asthma and obesity.3
The assessment and monitoring of the appropriateness of antibiotic prescription is essential for the purpose of detecting possible deficiencies in prescription and implementing measurements to improve the quality of antibiotherapy. However, few studies have assessed the appropriateness of antibiotic prescription in the PED setting,3,7 finding highly variable proportions of inappropriate prescription, and most have focused on specific infectious diseases.8
In recent years, several guidelines and consensus documents have been published in Spain with the aim of standardising empirical antibiotherapy in the paediatric population.9–12 In 2012, a nationwide survey was conducted to evaluate the selection of agents for empirical antibiotherapy in children based on current recommendations. The responses to the survey showed that 85% of prescribers adhered to the current guidelines.13
In January 2019, the Department of Health of the Autonomous Community of Madrid (ACM) published a guideline for the use of antimicrobials in paediatric patients at the outpatient level (ACM guideline),14 although we do not know the extent to which clinical practice in the region adhered to its recommendations.
The primary objective of our study was to evaluate the appropriateness of antimicrobial prescription at discharge from the PED of patients with infectious diseases using the ACM guideline as the reference.
The secondary objective was to analyse variations in the appropriateness of prescriptions based on the diagnosis of the patient and the type of provider that made the prescription. We also assessed the adherence of discharge prescriptions to the protocols of our hospital and the agreement between the reference guideline14 and our hospital protocols.15
Material and methodsWe conducted a retrospective, observational and descriptive study between March 2018 and February 2019 in the PED of a tertiary care hospital in Madrid that manages medical and surgical patients. In this PED, the physicians that manage the patients are mainly paediatrics specialists and medical residents in paediatrics and family and community medicine (FCM).
The study was approved by the Ethics Committee for Research with Medicines of our hospital and conducted in adherence with the principles of the Declaration of Helsinki.
Sample selectionWe included patients aged 0–16 years discharged home from the PED with a diagnosis matching any of the infectious diseases contemplated in the ACM guideline. For the purpose of the analysis of the appropriateness of prescription, we treated suspected diagnoses as confirmed diagnoses. We excluded children with infectious diseases that were not included in the protocols or guideline, immunosuppressed patients, patients that received a prescription of antibiotherapy before the visit to the PED and patients that were admitted to hospital.
In the sample size calculation, we determined that we would need 600 patients to achieve our primary objective with a precision of 4% and a level of confidence of 95%. Given that a proportion of appropriate antibiotic prescription at discharge from the emergency department had not been published in the past, we calculated the sample size assuming the worst possible statistical scenario, with an expected proportion of appropriate prescription of 50%. To estimate the number of emergency care episodes required to meet the necessary sample size, we performed an exploratory analysis in a sample of emergency visits managed in the PED on the 13th of each month in the 12 months preceding the start of the study period. We found that 704 patients met the inclusion criteria. Since that selection allowed us to prevent biases associated with seasonal patterns, to randomly include both weekday and weekend visits and to assume losses of up to 15% due to exclusion criteria, we decided to use the exploratory sample in the study.
Independent variablesWe analysed demographic variables such as age, sex, weight and the presence of allergies; clinical and treatment variables such as diagnostic category (grouped according to the ACM guideline classification: ear–nose–throat [ENT], respiratory, ophthalmologic, oral, genitourinary, cutaneous or gastrointestinal), prescription of antimicrobial therapy (yes/no), prescribed antibiotic agent, route, dose, interval between doses, duration; prescribing physician (adjunct or resident) and speciality of prescriber (paediatrics, FCM, other).
We analysed demographic variables relative to the total number of patients included in the study, and clinical and treatment variables relative to the total number of episodes that met the inclusion criteria and were considered independent and valid for recruitment, so that different episodes could correspond to the same patient.
The data were collected through the review of electronic health records in the hospital health information system (HP-HCIS®, DXC IT Corporate Solutions).
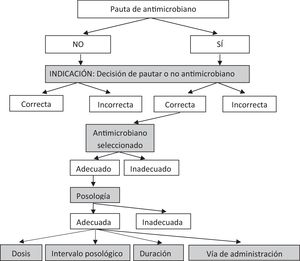
Outcome variablesThe primary outcome was the appropriateness of antibiotic prescription based on the ACM guideline and the secondary outcome the appropriateness of prescription based on hospital protocols. To determine the appropriateness of prescription, we applied 3 steps sequentially, so that if one step was found to be inappropriate, we did not assess the steps that followed: indication of treatment (disease warranting antibiotherapy), selection of the appropriate antimicrobial, and dosage (taking into account the dose, interval between doses, duration of treatment and route of administration). If a prescription was inappropriate in any of these aspects, we considered it inappropriate overall. If any of these prescription variables had not been documented, we treated the prescription event as missing data and did not take it into account in the analysis of overall appropriateness. To assess the appropriateness of antimicrobial selection, we considered appropriate selection of the first-line drug and also of second-line drugs in case it was justified (allergy to first-line drug or contraindication of first-line drug) (Fig. 1).
A resident in paediatrics and a resident in pharmacy, both in the 4th year of their residencies, were responsible for the initial determination of the appropriateness of prescriptions, and their conclusions were then cross-checked by 2 specialists in hospital pharmacy and 2 specialists in paediatric emergency medicine. In the case of disagreement, the prescription event was discussed between the senior paediatrics and pharmacy specialists.
Statistical analysisThe data were processed and analysed with the statistics software SPSS® 21.0 (IBM, Armonk, NY, USA).
We have expressed categorical variables as absolute frequencies and percentages and performed the inferential analysis with a 95% level of confidence. We expressed quantitative variables as median and interquartile range (IQR) due to the skewed distribution of the data.
We compared qualitative data with the Pearson χ2 test and considered p-values of less than 0.05 statistically significant.
We assessed the adherence of prescriptions to the ACM guideline and hospital protocols using the Cohen kappa coefficient, considering agreement poor for kappa values under 0.20; weak for kappa values between 0.21 and 0.40; moderate for values of 0.41–0.60; good for values of 0.61–0.80 and very good for values of 0.81–1.00.16
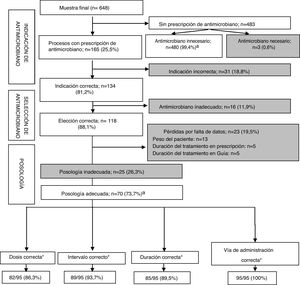
ResultsIn the period under study, the PED managed a total of 56,998 emergency visits, of which 1917 took place in the selected dates. Of these visits, 875 (45.6%) were due to infection, and in this subset, 704 (80.5%) corresponded to infectious diseases contemplated in the ACM. The final sample included 648 care episodes corresponding to 593 patients (Fig. 2).
In the final sample, 55.3% of patients were male (n = 328), and the median age was 2.6 years (IQR, 0.9–4.6 years) (Table 1).
Sociodemographic variables.
| Variable | Total, N = 593 patients, n (%) | Antimicrobial prescribed: n = 157 patients, n (%) | No antimicrobial prescribed: n = 436 patients, n (%) |
|---|---|---|---|
| Sex | |||
| Male | 328 (55.3%) | 77 (49.0%) | 251 (57.6%) |
| Female | 265 (44.7%) | 80 (51.0%) | 185 (42.4%) |
| Agea | |||
| Neonate | 5 (0.8%) | 2 (1.3%) | 3 (0.7%) |
| Young infant | 21 (3.6%) | 1 (0.6%) | 20 (4.6%) |
| Infant/toddler | 244 (41.1%) | 52 (33.1%) | 192 (44.0%) |
| Child/adolescent | 323 (54.5%) | 102 (65.0%) | 221 (50.7%) |
| Allergy to antimicrobialsb | 3 (0.5%) | 1 (0.6%) | 2 (0.4%) |
| Aminopenicillins | 3 | 1 | 2 |
| Cephalosporins | 2 | – | 2 |
| Non-beta-lactam antibiotics | – | – | – |
We considered the care episode corresponding to the first visit to the PED (except in patients that did not receive a prescription in the first visit but did in a later visit). Age groups: neonate, 0–2 7 days; young infant, ≥28 days and <3 months; infant/toddler, ≥3 months and <24 months; child/adolescent, ≥24 months and <16 years.
The most frequent diagnostic group was respiratory infection (n = 330; 50.9%), with a predominance of upper respiratory tract infections (n = 238; 36.7%) (Table 2).
Diagnoses and prescribed antimicrobials.
| Total N = 648 episodes, n (%) | Antimicrobial prescribed: n = 165 episodes, n (%) | No antimicrobial prescribed: n = 483 episodes, n (%) | |
|---|---|---|---|
| Diagnosis group | |||
| Respiratory infection | 330 (50.9%) | 19 (11.5%) | 311 (64.4%) |
| ENT infection | 152 (23.5%) | 97 (58.8%) | 55 (11.4%) |
| Gastrointestinal infection | 100 (15.4%) | 1 (0.6%) | 99 (20.5%) |
| Ocular infection | 25 (3.9%) | 18 (10.9%) | 7 (1.4%) |
| Genitourinary infection | 19 (2.9%) | 12 (7.3%) | 7 (1.4%) |
| Cutaneous infection | 15 (2.3%) | 14 (8.5%) | 1 (0.2%) |
| Oral infection | 7 (1.1%) | 4 (2.4%) | 3 (0.6%) |
| Diagnosis subgroup | |||
| URTI | 238 (36.7%) | – | 238 (49.3%) |
| Gastroenteritis | 99 (15.3%) | – | 99 (20.5%) |
| Acute otitis media | 77 (11.9%) | 68 (41.2%) | 9 (1.9%) |
| Acute pharyngitis | 69 (10.6%) | 25 (15.2%) | 44 (9.1%) |
| Laryngitis | 40 (6.2%) | – | 40 (8.3%) |
| Bronchiolitis | 33 (5.1%) | – | 33 (6.8%) |
| Conjunctivitis | 18 (2.8%) | 11 (6.7%) | 7 (1.4%) |
| Pneumonia | 17 (2.6%) | 17 (10.3%) | – |
| UTI | 9 (1.4%) | 9 (5.5%) | – |
| Other | 48 (7.4%) | 35 (21.2%) | 13 (2.7%) |
ENT, ear–nose–throat; URTI, upper respiratory tract infection; UTI, urinary tract infection.
Of the total care episodes analysed, 466 (71.9%) were managed by physicians of the department of paediatrics: 350 (75.1%) were residents in paediatrics, and 116 (24.9%) paediatricians. Other physicians involved in care delivery were residents in FCM and other departments, such as paediatric surgery.
In 165 care episodes (25.5%; 95% confidence interval [CI], 22.1%–28.8%) at least one antimicrobial agent was prescribed at discharge: antibiotics in 156 cases, antifungals in 8 and an antiparasitic agent in 1. In most cases, the prescription was for administration via the oral route (81.8%). When it came to antibiotic prescription, penicillins were the predominant group, prescribed in 121 of the care episodes (73.3%): amoxicillin was prescribed most frequently, in 100 care episodes (60.6%), followed by amoxicillin–clavulanic acid in 20 (12.1%) and penicillin v in 1 (0.6%) (Appendix B).
Adherence to the ACM guidelineOverall, we found adherence to the ACM guideline in every aspect (indication, selection, dose, dose interval, duration of treatment and route of administration) in 550 of the 625 episodes (88.0%; 95% CI, 85.5%–90.6%) (Table 3). We considered another 23 episodes, all treated with antimicrobials, losses to follow-up due to the absence of data required to assess aspects of antibiotic dosage. Fig. 3 presents the stepwise evaluation of antibiotic prescription appropriateness. In 591 episodes (94.6%), adherence to the guideline was considered adequate, in 3 (0.5%) inadequate due to failure to prescribe antibiotherapy in cases in which it was indicated (submandibular lymphadenopathy, conjunctivitis and animal bite) and in 31 (5.0%) inadequate due to unnecessary antibiotic prescription.
Adherence of antimicrobial prescription to the ACM guideline and hospital protocols by diagnosis.
| Adherence by diagnosisa | |||||
|---|---|---|---|---|---|
| Disease (n) | Antimicrobial prescription, n (%) | Reference: ACM guideline | Reference: hospital protocol | ||
| Overall adherence n (%) | Adherence in diseases treated with antimicrobials, n (%) | Overall adherence, nb (%) | Adherence in diseases treated with antimicrobials, nb (%) | ||
| URTI (238) | – | 238/238 (100.0%) | –/– | No protocol | No protocol |
| AGE (99) | – | 99/99 (100.0%) | –/– | 99/99 (100.0%) | –/– |
| AOM (69) | 60 (87.0%) | 36/69 (52.2%) | 27/60 (45.0%) | 50/69 (72.5%) | 41/60 (68.3%) |
| AP/T (65) | 21 (32.3%) | 59/65 (90.8%) | 15/21 (71.4%) | 58/65 (89.2%) | 15/21 (71.4%) |
| Laryngitis (40) | – | 40/40 (100.0%) | –/– | 40/40 (100.0%) | –/– |
| Bronchiolitis (33) | – | 33/33 (100.0%) | –/– | 33/33 (100.0%) | –/– |
| Conjunctivitis (12) | 5 (41.7%) | 6/12 (50.0%) | 0/5 (0%) | 8/12 (66.7%) | 4/5 (80.0%) |
| Pneumonia (16) | 16 (100.0%) | 13/16 (81.2%) | 13/16 (81.3%) | 14/16 (87.5%) | 14/16 (87.5%) |
| UTI (9) | 9 (100.0%) | 4/9 (44.4%) | 4/9 (44.4%) | 3/9 (33.3%) | 3/9 (33.3%) |
| Other (44) | 31/44 (70.5%) | 22/44 (50.0%) | 11/31 (35.5%) | 9/10 (90.0%)a | 5/6 (83.3%)a |
| Total (625) | 142 (22.7%) | 550/625 (88.0%) | 70/142 (49.3%) | 314/353 (89.0%)c | 82/117 (70.1%)c |
AGE, acute gastroenteritis; AOM, acute otitis media; AP/T, acute pharyngitis/tonsillitis; URTI, upper respiratory tract infection; UTI, urinary tract infection.
Appropriateness of antimicrobial prescription in reference to the ACM guideline based on the different assessment steps (indication, selection, dosage). Shaded boxes present inappropriate treatment approaches.
*Overall data, without sequential analysis: some prescriptions were inappropriate in more than one aspect of dosage.
aPrescription considered appropriate; n = 550.
We were able to assess the appropriateness of prescription in 142 episodes treated with antimicrobials, with prescription being appropriate in 70 episodes (49.3%; 95% CI, 41.1%–57.5%), and erroneous dosage being the most frequent reason that prescription was inappropriate (Table 4).
Reasons antibiotic prescription was considered inappropriate based on the ACM guideline and hospital protocols by diagnosis.
| Treated episodes with discrepancy in appropriateness category based on applied referencea | ||||||||
|---|---|---|---|---|---|---|---|---|
| Managed episodes (n) | Based on ACM guideline | Based on hospital protocols | ||||||
| Inadequate treatment, n (%) | Reason treatment was inappropriateb | Inadequate treatment, n (%) | Reason treatment was inappropriateb | |||||
| Indication, n (%) | Selection, n (%) | Dosage, n (%) | Indication, n (%) | Selection, n (%) | Dosage, n (%) | |||
| AOM (60) | 33 (55.0%) | 19/60 (31.7%) | 6/41 (14.6%) | 8/35 (22.9%) | 19 (31.7%) | 11/60 (18.3%) | 5/49 (10.2%) | 3/44 (6.8%) |
| AP (21) | 6 (28.6%) | 2/21 (9.5%) | 1/19 (5.3%) | 3/18 (16.7%) | 6 (28.6%) | 0/21 | 3/21 (14.3%) | 3/18 (16.7%) |
| Conjunctivitis (5) | 5 (100%) | 3/5 (60%) | 2/2 (100.0%) | 0/0 | 1 (20.0%) | 1/5 (20.0%) | 0/4 | 0/4 |
| Pneumonia (16) | 3 (18.8%) | 0/16 | 0/16 | 3/16 (18.8%) | 2 (12.5%) | 0/16 | 1/16 (6.3%) | 1/15 (6.7%) |
| UTI (9) | 5 (55.6%) | 0/9 | 2/9 (22.2%) | 3/7 (42.9%) | 6 (66.7%) | 1/9 (11.1%) | 1/8 (12.5%) | 4/7 (57.1%) |
| Other (31)c | 20 (64.5%) | 7/31 (22.6%) | 5/24 (20.8%) | 8/19 (42.1%) | 1/6 (16.7%) | 0/6 | 1/6 (16.7%) | 0/5 |
| Total (142)d | 72/142 (50.7%) | 31/142 (21.8%) | 16/111 (14.4%) | 25/95 (26.3%) | 35/117 (29.9%) | 13/117 (11.1%) | 11/104 (10.6%) | 11/93 (11.8%) |
AOM, acute otitis media; AP, acute pharyngitis/tonsillitis; URTI, upper respiratory tract infection; UTI, urinary tract infection.
In the separate analysis of the indication of antibiotherapy, we found an increased probability of unnecessary antimicrobial prescription in the group of patients under 2 years (16/59 episodes [27.1%] compared to 15/106 episodes [14.2%] in older children and adolescents).
Adherence to ACM guideline by prescriber categoryWe found that overall, prescription practices adhered to the guideline in 85% of cases in paediatricians and residents in paediatrics or FCM, a level of adherence that was significantly greater compared to physicians in other specialities. The adherence was substantially lower in the subset of episodes treated with antimicrobials, without differences based on the type of prescriber (Table 5).
Overall appropriateness and appropriateness of prescribed antibiotherapy based on ACM guideline by type of prescribing physician.
| Department | Prescribing physician | Managed episodesa, n (%) | Overall adherence to guideline, n (%) | p | Episodes with antibiotic prescriptiona, n (%) | Appropriate antibiotic prescription, n (%) | p |
|---|---|---|---|---|---|---|---|
| Paediatrics | Resident | 337 (53.9%) | 299 (88.7%) | 0.003 | 66 (46.5%) | 29 (43.9%) | 0.318 |
| Specialist | 109 (17.4%) | 94 (86.2%) | 0.009 | 31 (21.8%) | 18 (58.1%) | 0.145 | |
| FCM | Resident | 172 (27.5%) | 154 (89.5%) | 0.002 | 40 (28.2%) | 22 (55.0%) | 0.172 |
| Other | Resident or specialist | 7 (1.1%) | 3 (42.9%) | Ref | 5 (3.5%) | 1 (2.0%) | Ref |
| Total | 625 | 550 (88.0%) | 142 | 70 (49.3%) |
FCM, family and community medicine; Ref, reference group.
Tables 3 and 4 summarise the results concerning the appropriateness of antimicrobial prescription by diagnosis. We found that inappropriate prescription practices were most frequent in the management of acute otitis media (AOM), especially in the 0–2 years age group (32.4% of appropriate prescription in these patients vs 52.2% in the overall sample), conjunctivitis and urinary tract infection (UTI) (Table 3).
Table 4 presents the distribution of inappropriately treated episodes by reason prescription was inappropriate (indication, selection or dosage). Conjunctivitis and AOM stood out for the substantial proportion of cases treated with unnecessary antibiotherapy based on the ACM guideline (60.0% and 31.7%, respectively). Three cases of viral conjunctivitis were treated with tobramycin in the absence of manifestations suggestive of bacterial superinfection. In the case of AOM, there was a particularly high frequency of inappropriate prescription in patients aged 0–2 years (13/32 cases; 40.6%) compared to patients aged 2 or more years (6/28; 21.4%).
In the 6 cases of AOM with inappropriate prescription due to selection, the error was the prescription of an agent with a spectrum too narrow for empirical therapy in patients aged 6–24 months that required amoxicillin–clavulanic acid due to severe symptoms, recurrent AOM o previous treatment with amoxicillin in the past 30 days. In the case of patients with conjunctivitis, selection errors occurred in 2 infants under 12 months treated with tobramycin, when the guideline recommended prescription of erythromycin or aureomycin, and in cases of UTI, in 2 patients treated with cotrimoxazole instead of fosfomycin.
When it came to dosage, the diseases in which prescription was inappropriate most frequently were UTIs, with 3/7 inappropriate prescriptions (42.9%). In 2 of these cases, fosfomycin sodium, which was indicated, was prescribed to be administered every 6 h, when the recommended dose interval in the guideline is 8 h. There were 6 cases with inappropriate dosage among patients with AOM (22.9%), in 4 cases due to prescription of treatment with amoxicillin–clavulanic acid for too short a duration, and in the rest due to prescription of an inappropriate dose. We did not assess the appropriateness of dosage in cases of conjunctivitis, as the ACM guideline did not specify a recommended duration of treatment for this disease.
Adherence to hospital protocolsWe found that hospital protocols applied to 372 of the 648 episodes (57.4%), and were able to analyse the appropriateness of prescription in 353 (19 episodes lost due to missing data). In this subset, we found an overall frequency of appropriate prescription in every considered aspect of 89.0%. Of all these episodes, 236 (66.9%) were not treated with an antimicrobial, which was the correct approach in 232 episodes (98.3%), while antibiotherapy was indicated but not prescribed in another 4 episodes: 3 of conjunctivitis and 1 of pharyngitis.
Analysing only the 117 treated episodes (33.1%) using hospital protocols as reference, we found that 82 (70.1%) had been managed correctly (Table 3). Errors were distributed uniformly between indication, drug selection and dosage (Table 4). We found a marked proportion of inappropriate prescription in the management of UTIs (57.1%), with poorer adherence relative to hospital protocols versus the ACM guideline because the hospital protocol called for administration of more than 1 dose of fosfomycin trometamol. Contrary to this, prescriptions were for a single dose, as recommended by the ACM guideline.
Comparison of ACM guideline and hospital protocolsWe analysed the agreement between adherence to the ACM guideline and to hospital protocols, and found a good overall agreement (κ = 0.673). The agreement was complete for the most frequent infectious diseases (acute gastroenteritis, laryngitis and bronchiolitis) (κ = 1), and very high in the approach to acute pharyngitis/tonsillitis (κ = 0.915). It was good in the management of pneumonia (κ = 0.765), moderate for AOM (κ = 0.586) and weak for UTIs (κ = 0.308), and there was no agreement when it came to conjunctivitis (κ = 0.000).
DiscussionThis is the first study conducted in Spain to analyse the appropriateness of antimicrobial prescription in the PED of a tertiary care hospital using as reference the most recent guideline for outpatient antibiotherapy of the Department of Health of Madrid.14 Our study allowed us to identify the areas most in need of improvement and that will require more proactive efforts in the implementation of this new guideline.
We found that, overall, antibiotic prescription practices were appropriate in 88.0% of cases, which was consistent with other studies conducted in Spain and abroad (85%13–85.2%17) describing the appropriateness of prescription based on different guidelines.13,17 The percentage of adherence when it came to viral diseases such as acute gastroenteritis, laryngitis and bronchiolitis was high and greater compared to other case series,3,18,19 a relevant finding given that absence of antibiotic prescription for management of viral infections is widely considered a care quality indicator.3
However, when we analysed the episodes treated with antibiotics, adherence dropped to 49.3%, which was consistent with the findings of other studies in Spain both in emergency care3 and primary care17 settings. In these studies, inappropriate prescription was mainly due to prescription of the wrong agent, or an agent that was not indicated (inadequate selection), while the most frequent reason of noncompliance with the guideline in our study was inappropriate dosage.
Previous studies have focused on the problem of excessive antibiotic use. One of them reported that 31.7% of unnecessary prescriptions occurred in patients aged 0–4 years.17 Our study found a lesser frequency of antimicrobial overprescribing, even among neonates, infants and toddlers, the age group in which we found the poorest results (27.1%).
Some studies suggest that the quality of prescribing decreases with increasing years of experience,13,20 which would be attributed to physicians failing to stay updated overtime. However, our study did not find differences in prescribing between resident and adjunct physicians, which may suggest that most physicians that staffed the PED in our hospital knew the guidelines and adhered to the protocols.
The analysis by disease identified AOM, UTIs and conjunctivitis as the infectious diseases in which prescribing practices adhered the least to the reference guideline. The survey published in the context of the ABES study13 applied a reference that only considered prescription of antibiotherapy (with amoxicillin or amoxicillin–clavulanic acid) as the correct empirical treatment for AOM in children aged 0–2 years. In contrast, the ACM guideline considers prescription of empirical antibiotherapy in patients aged 6 months to 2 years inappropriate in the absence of a certain diagnosis of AOM (acute onset with otalgia and otorrhoea or bulging of tympanic membrane) and risk factors. This seems to be one of the main sources of noncompliance with the guideline and contributed to the poor correlation between the adherence to the guideline and the adherence to hospital protocols. When it came to UTIs, the discrepancies would be justified by the selection of the antimicrobial based on local patterns of antimicrobial resistance and the results of urine culture in the patient. We ought to highlight that 90.8% of cases of acute pharyngitis were treated correctly, which stood in contrast to other studies in the paediatric emergency care setting that found that antibiotics were prescribed in up to 40% of patients with a clinical picture indicative of viral infection.3
The overall agreement between the adherence to the ACM guideline14 and the adherence to the protocols of our hospital15 was good, especially for diseases that did not require antibiotherapy. However, we found that 2 bacterial diseases considered potentially serious (pneumonia and UTI) were among the diseases in which the agreement between adherence to the guideline and to hospital protocol was poorest.
These discrepancies in diseases that may be very serious, in addition to other diseases that may have a lesser impact but are more frequent, warrant a systematic review of the current scientific evidence to identify areas in which recommendations conflict and update protocols and guidelines. As Principi and Esposito propose,21 the implementation of antibiotic stewardship measures, such as educational programmes, training of multidisciplinary teams, ongoing monitoring of antibiotic prescription, use of diagnostic tests and knowledge of local resistance patterns could have a significant impact on the rational use of antibiotics in the field of paediatrics.
Beta-lactam antibiotics were prescribed most frequently, and amoxicillin in particular. The prescription of amoxicillin (relative to both total antibiotic prescription and total broad-spectrum antibiotic prescription) is used as an indicator of the quality of prescribing.22 Our study found a lower frequency of amoxicillin–clavulanic acid prescription compared to other case series.3,23 The use of penicillin v for treatment of pharyngitis was infrequent (4.8%), which was consistent with previous findings in Spain (4.0%).8
The main limitation of the study was its retrospective design due to its intrinsic biases and the loss of data that were not documented, such as the body weight of some patients or the duration of treatment. The prescriptions included in the analysis corresponded to the months that preceded the implementation of the new guideline, and there were details of prescription, such as the duration of treatment or the interval between doses, that determined whether prescription was considered appropriate or inappropriate that probably varied depending on the recommendations that were taken as reference. Lastly, the absence of hospital protocols for certain diseases precluded the analysis of the agreement between appropriateness based on hospital protocols versus the ACM guideline in some cases.
To conclude, we may highlight the substantial adherence of pharmacological treatment of infectious diseases managed in the PED of our hospital to the ACM guideline, although this proportion decreased for diseases requiring antimicrobial treatment, with errors in dosage being the main reason for inappropriate prescription. We found a greater adherence to hospital protocols compared to the new ACM guideline, which evinced discrepancies between these 2 references that should be investigated and corrected based on the current scientific evidence and taking into account local trends in antimicrobial resistance.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: García-Moreno FJ, Escobar-Castellanos M, Marañón R, Rivas-García A, Manrique-Rodríguez S, Mora-Capín A, et al. Adecuación de la prescripción de antimicrobianos en procesos ambulatorios atendidos en Urgencias. An Pediatr (Barc). 2022;96:179–189.