Although sleep disturbances in infants and toddlers are common, there is no suitable validated tool in Spanish to evaluate sleep disorders. The Brief Infant Sleep Questionnaire (BISQ) is a well-established multidimensional questionnaire widely used internationally.
ObjectivesTo adapt the BISQ questionnaire to Spanish and analyse its reliability and validity. To explore its feasibility, both in the clinical context, and in epidemiological research.
MethodsParticipants were parents of children between 3 and 30 months of age. The adaptation to Spanish (BISQ-E) was achieved by using both back translation and consensus, following the international guidelines.Reliability was determined by means of test–retest and measurement of agreement (Kappa value) between 2 forms of administration of the questionnaire (self-administration and clinical interview). Construct validity was established by analysing its correlation with a sleep diary.
ResultsA total of 87 families/children participated. The test–retest reliability undertaken in 60 subjects was r=0.848 (P<.001). The kappa value was 0.939 (95% CI: 0.858–1.00, P<.001).The agreement between BISQ-E and the sleep diary was analysed in 27 families/children, with statistically significant values being obtained for the following variables: bedtime (r=0.731), hours of night sleep (r=0.726), hours of daytime sleep (r=0.867), and number of nocturnal awakenings (r=0.888) (P<.001).
ConclusionsThe Spanish adaptation of the BISQ shows overall adequate validity and reliability for the evaluation of sleep in infants and pre-school children. Its use as a clinical tool, or for clinical-epidemiological research studies, is feasible.
Aunque las alteraciones del sueño en lactantes y preescolares son comunes, no se dispone de un instrumento en español adecuadamente validado para su estudio. El Brief Infant Sleep Questionnaire (BISQ) es un cuestionario multidimensional bien establecido con este fin en el ámbito internacional.
ObjetivosAdaptar el BISQ al español y analizar su fiabilidad y validez. Explorar su viabilidad en el contexto asistencial y de investigación.
Participantes y métodosSe incluyeron niños de 3 a 30 meses de edad. La adaptación al español (BISQ-E) se efectuó mediante técnica bilingüe de retrotraducción y consenso, siguiendo las recomendaciones internacionales. Se evaluó la fiabilidad mediante análisis de los resultados del test–retest del BISQ-E y de la concordancia de las respuestas a 2formas de administración (autoadministración y entrevista clínica). La validez de constructo se estableció analizando su correlación con un diario de sueño.
ResultadosParticiparon un total de 87 familias/niños. La correlación global test–retest en 60 sujetos fue de r=0,848 (p<0,001). El índice de kappa entre las 2formas de administración fue de 0,939 (IC 95%: 0,858–1,00; p<0,001).La correlación BISQ-E-diario de sueño se analizó en 27 familias/niños y fue estadísticamente significativa para las variables estudiadas: hora de acostarse (r=0,731), horas de sueño nocturno (r=0,726), horas de sueño diurno r=0,867) y número de despertares nocturnos (r=0,888) (p<0,001).
ConclusionesLa adaptación española del BISQ presenta unas características de validez y fiabilidad adecuadas para la evaluación del sueño en lactantes y preescolares. Su utilización como instrumento clínico o para estudios de investigación clínico-epidemiológica resulta factible.
Sleep disturbances in children are among the most frequent reasons for consultation in paediatric clinical practice.1,2 Previous studies report that between 25% and 46% of the paediatric population may experience some type of sleep disturbance during childhood or adolescence.3,4 The prevalence reported in the literature for children aged less than 3 years ranges between 11% and 40%.5,6 Many sleep disturbances are behavioural in nature (difficulty falling asleep, difficulty staying asleep or poor sleep hygiene),7 so their prevention and management should start as early as possible and should be pursued from the field of primary care.
Current sleep recommendations and guidelines are mainly based on expert opinion and consensus, as there is little experimental evidence in this field.2,8 Notwithstanding, the available literature evinces a growing interest in the essential link between sleep and adequate physical, cognitive and psychosocial development, including its impact on family dynamics.9–11 The sleep-onset time and the total duration of sleep in the first years of life are considered predictors for features of anxiety (separation anxiety, introversion)12,13 and have been associated with an adequate acquisition of healthy eating habits14 and increased inactivity and obesity in toddlers.15
In light of their importance, routine screening of sleep disturbances would be helpful for their early detection, which would allow appropriate intervention and thus improvement of psychosocial and cognitive outcomes in the paediatric population.16
The multidimensional nature of sleep poses challenges to its evaluation. Polysomnography and actigraphy contribute relevant data,11,17 but their usefulness is limited due to their low feasibility in large-scale population-based studies. Furthermore, they offer little towards the assessment of some behavioural factors that play important roles in sleep.1 This is why it is important to develop questionnaires that can assess subjective variables such as the restorative quality of sleep and the potential impact on the family.
The Brief Infant Sleep Questionnaire (BISQ) is one of the most widely used questionnaires currently available for the assessment of sleep in early childhood (Table 1).18 It was designed to be administered to parents of children aged 3–30 months of age. This questionnaire stands out because it is a robust instrument of proven reliability and validity, easy to use and brief (14 items), and thus could be used as a screening tool.1,7,16,19 The BISQ has been widely used in countries such as the United States and China.20–23 In addition to the English version, it has been translated to Portuguese,24 Turkish,25 Chinese21 and Nepalese.26
Instruments to assess sleep in infancy and early childhood.
| Instrument (acronym) | Author, year | Age | Dimensions assessed | Items | Assessment period |
|---|---|---|---|---|---|
| Infant Sleep Questionnaire (ISQ) | Morrell, 1999 | 12–18 months | Tool to screen for difficulty falling asleep and duration of night-time sleep | 10 | 1 month |
| Maternal Cognitions about Infant Sleep Questionnaire (MCISQ) | Morrell, 1999 | 12.9–16.8 months | Sleep habits, parent attitudes towards difficulties falling and staying asleep, demographic variables | 20 | Not specified |
| Obstructive Sleep Apnea (OSA) | Franco, 2000 | 6 months–12 years | Breathing pattern during sleep, mood, daytime sleepiness, parental anxiety | 18 | 4 weeks |
| Sleep and Settle Questionnaire (SSQ) | Matthey, 2001 | 6 weeks–6 months | Instrument to assess difficulties falling asleep, duration of night-time sleep and daytime behaviour | 34 | 1 week |
| Parental Interactive Bedtime Behaviour Scale (PIBBS) | Morrell, 2002 | 12–19 months | Method to help child fall asleep | 22 | Not specified |
| Brief Infant Sleep Questionnaire (BISQ) | Sadeh, 2004 | 0–30 months | Instrument to assess duration of sleep, duration of sleep by circadian rhythm and night-time awakenings | 13 | 2 weeks |
| Tayside Children's Sleep Questionnaire (TCSQ) | McGreavey, 2005 | 1–5 years | Instrument for screening difficulties falling and staying asleep | 10 | 3 months |
| Children's Sleep Status Questionnaire (CSSQ) | Xiao, 2009 | 0–5 years | Bedtime routines, sleep patterns, sleep disorders, sleep habits, demographic characteristics | 47 | 1 month |
The Spanish primary care clinical practice guideline on sleep disorders in children and adolescents proposes this instrument as the preferred choice for screening of sleeping disorders in early childhood.27
To date, there is no version translated to Spanish and adapted to the Spanish population with an appropriate methodology, including assessment of its psychometric properties. Our hypothesis was that it would be possible to develop a Spanish version of the BISQ that would retain its good psychometric properties. Consequently, the aim of our study was to translate and adapt the original versions and analyse the reliability and validity of the new questionnaire in Spanish.
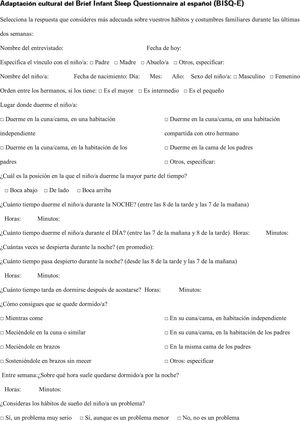
Patients and methodsThe BISQ comprises 14 items: 4 on the demographic characteristics of the child and 10 on sleep habits. There are 4 multiple-choice single-answer questions and 6 open-ended questions about the timing and duration of sleep. To adapt these items, we followed the general recommendations of the International Test Commission guidelines for test translation and adaptation28 as well as specific recommendations for adapting health-related quality of life (HRQoL) assessment tools.29,30
First phase: transcultural translation and adaptation to the Spanish populationAfter obtaining permission from the author of the original BISQ,18 we followed a process of forward-backward bilingual translation and adaptation by consensus. Thus, 3 members of the research team produced 3 translations to Spanish of the original instrument, independently and blinded to each other's work. This was followed by the collaborative development of a single integrated version, reaching a consensus on the wording of each item on the scale. This preliminary version was submitted to a native English speaker that was not acquainted with the original English version and produced a backward translation. After analysing these versions in a consensus meeting, additional changes were made. Finally, we performed a pilot test of the translation in 5 families, which resulted in subtle adaptations and the definitive version of the Spanish BISQ (BISQ-E) (Appendix A).
Second phase: validation of the questionnaireTo determine whether the psychometric properties of the translated questionnaire were acceptable, we assessed its reliability and validity.
To assess its reliability, we analysed two components: (A) interobserver reliability and (B) intraobserver reliability.
- A)
We measured the agreement of the answers obtained with the BISQ-E when it was self-administered compared to when it was administered by an interviewer.
We selected an item of the questionnaire that was important in the interpretation of results18 (Do you consider your child's sleep habits a problem?) and compounded the two affirmative answer choices into a single one to turn the answer into a dichotomous variable (yes/no).
A total of 60 families completed the BISQ-E before their appointment in the referral hospital where the questionnaire was validated. Later on, a member of the research team asked the aforementioned question (administration by interviewer) to assess the degree of agreement of the two answers obtained for this item. We estimate that approximately 20–30min passed between the two interventions.
- B)
We performed correlation analysis to assess test–retest reliability, for which we administered the BISQ-E to a group of 27 families at 2 time points: during the first contact of the families with the research team (T1), and after a period of at least 1 week from the first test (T2).
To analyse construct validity, we compared the results of the BISQ-E questionnaire with the records of a sleep diary. The diary was formatted as a table and was used to collect different variables related to sleep-wake cycle patterns for 7–14 days: bedtime, sleep-onset time, night-time awakenings (number and duration), time of final awakening and hours of daytime sleep. The sleep diary is a valid and independent instrument to assess sleep patterns in children and is considered the gold standard for subjective sleep assessment.31 To compare the two measures, we asked the 27 families that had completed the BISQ-E to fill out the sleep diary for 7 consecutive days (diary adapted from Richman32).
Study population and participantsTo assess reliability, we included 60 child/family by consecutive sampling. For the assessment of validity, we selected a convenience sample of 27 individuals. Overall, the study included 87 healthy children aged 3–30 months (60 in the assessment of reliability and 27 in the assessment of validity) included in the outpatient caseload of the department of paediatrics of the Hospital Universitario General de Catalunya. The inclusion criteria were to have an age in the established range and consent from the parents or legal tutors to participate in the study. The exclusion criteria were presence of a language barrier and refusal to participate.
The field work took place between October 2016 and April 2017.
Statistical analysisTo assess interobserver agreement, we analysed the concordance between the 2 modes of administration (self-administered and administration by interviewer) by calculating the kappa statistic for the dichotomous answer variable. To assess validity, we calculated the Pearson correlation coefficient for the comparison of BISQ-E variables and the records of the sleep diary.
We calculated the sample size assuming a correlation of .35 for an α level of .05 and a β level of .20. Although the assumed correlation was lower than the correlation reported in previous studies,18 we chose to use a conservative estimate to maximise the sample size and guarantee statistical power.
Ethical considerationsParents received oral and written information and signed an informed consent form. The study adhered to the basic principles of the Declaration of Helsinki, the Council of Europe Convention of Human Rights and Biomedicine, the Universal Declaration on the Human Rights of the UNESCO and Spanish law on biomedical research.
ResultsOnce the BISQ-E questionnaire was developed through the adaptation process described above, which included the adjustment of the time frame considered “night-time” based on Spanish cultural norms and the geographical time zone, we studied its psychometric properties by assessing its validity and reliability.
Eighty-seven families with children aged 3–30 months that resided in the autonomous community of Catalonia participated in the study. The mean age of the children was 17.95 months (SD, 9.04), 59% were male, and 62% were single or first-born children. In addition, 65% were enrolled in child care. The mean age was similar in parents and mothers (36 years), and 58% of parents had a university education.
Of all the families that agreed to participate, only one withdrew from the study.
Assessment of reliability- A)
In the group of 60 families, we analysed the interobserver reliability of the BISQ-E by comparing the answers obtained with the 2 different methods of administration (self-administration versus interview). We found a high level of agreement, with a high kappa value of 0.93 (95% CI, 0.85–1.00; P<.001).
- B)
We measured the test–retest reliability of the BISQ-E administered twice in the same subjects to assess its consistency over time. To do so, we measured the Pearson correlation for the sleep scores obtained in 2 different times that the BISQ-E was administered to each subject, T1 and T2. The mean time elapsed between the 2 time points in the test–retest assessment (T1–T2) was 10 days (range, 8–22 days).
We found a strong correlation in the different variables analysed in the test–retest reliability assessment: bedtime (r=0.735), hours of night-time sleep (r=0.881), hours of daytime sleep (r=0.900) and number of awakenings (r=0.876). All the correlations were statistically significant, with P-values of less than .001; we found a high consistency between the 2 time points in the overall questionnaire (r=0.848) and all the subscale scores. Table 2 presents these results and compares them to the results of the validation study of the original questionnaire.18
Test–retest correlation coefficients for the original BISQ18 and the BISQ-E.
| Original BISQ | BISQ-E | |
|---|---|---|
| Test–retest | Test–retest | |
| Sleep-onset time | r=0.95 (P<.001) | r=0.735 (P<.001) |
| Hours of night-time sleep | r=0.82 (P<.001) | r=0.881 (P<.001) |
| Hours of daytime sleep | r=0.89 (P<.001) | r=0.900 (P<.001) |
| Number of awakenings | r=0.88 (P<.001) | r=0.876 (P<.001) |
r=Pearson correlation coefficient.
We administered the BISQ-E to the 27 families selected by nonprobability sampling. Subsequently, the same families filled out the sleep diary for 7 consecutive nights. We found a high and statistically significant correlation between the two measures for the variables bedtime during weekdays (Monday through Friday) (r=0.731), hours of night-time sleep (between 8 pm and 7 am) (r=0.726), hours of daytime sleep (between 7 am and 8 pm) (r=0.867) and number of night-time awakenings (r=0.888). We also found a moderate correlation for the variable bedtime on weekend days (r=0.692), which was also statistically significant.
DiscussionWe chose the BISQ as the measure to be validated after careful consideration. To make this decision, we performed an exhaustive review of the relevant literature. Among many other studies, we identified 4 recent systematic reviews on the methods used to assess sleep in the paediatric age group.1,16,19,33 The BISQ stood out in the comparative analysis of the psychometric properties of these instruments.1,16,19Table 1 describes the different instruments designed to assess sleep mainly in early childhood that we considered for our study.
One of the main advantages of the BISQ is that it contributes to the adequate assessment of different aspects of sleep with a multidimensional approach by the use of a single and brief instrument. The different measures that are obtained with the use of the BISQ are: time of sleep onset (hours), duration of night-time sleep (hours), duration of daytime sleep (hours), total sleep duration (hours), night-time awakenings (number), duration of night-time awakenings (hours). The author of the questionnaire18 established 3 criteria to identify children with inadequate sleep patterns: a sustained pattern of more than 3 night-time awakenings, 1 hour of wakefulness during the night-time period, or total duration of sleep of less than 9h in 24h. According to Sadeh, these indicators remain stable in children between ages 6 and 30 months.18 However, given the variability of sleep patterns at these ages and the semiqualitative character of their assessment, the questionnaire cannot be used to diagnose a sleep disorder. Rather, it helps identify early and by simple means those children that could benefit from improvement of sleep habits or require further follow-up.
The BISQ has been used widely to assess the quality of sleep in the healthy paediatric population, and it has also been used to study sleep patterns in specific situations. For instance, it has been used to assess sleep in breastfed infants compared to formula-fed infants,34 in infants with Williams syndrome,35 children that snore36 and preterm infants.21 It has also been used to assess sleep in relation to obesity15 and the use of new information technologies,22 in studies on postpartum depression37 or in relation to diseases such as atopic dermatitis.38 In Spain, it has been used in a cross-sectional study that compared the populations of Asturias and Castilla y León.39
In the validity analysis, the new BISQ-E version exhibited a strong correlation with a detailed and much more labour-intensive method, the sleep diary. This suggests that the BISQ-E provides adequate measures of the dimensions assessed by the sleep diary. Furthermore, when it came to reliability, we found high test–retest correlations with values that were similar to those obtained for the original questionnaire by its author18 (Table 2). Similarly, we found an excellent agreement between the results obtained when the BISQ-E was self-administered and the results obtained when it was administered by an interviewer (questions asked by a clinician). In the sample of 60 families analysed in our study, the parents, accompanied by their children, were able to fill out the questionnaire in the waiting room of the department of paediatrics in approximately 8–10min, a fact that further reinforces that the BISQ-E could be an excellent screening tool in this population.
Among the possible limitations of the study, we ought to mention the relatively small sample size of our study, although it did suffice to obtain statistically significant values in the analysis of psychometric properties. Furthermore, the fact that all the families to which we administered the questionnaire were managed in a single centre could restrict the generalisation of our results to other populations. However, since we used the questionnaire to assess children with no detectable disease and of the ages for which the questionnaire was designed, we think that this will probably not be a relevant factor in the results that may be obtained in other populations. On the other hand, our reliability analysis had sufficient power to estimate correlations, since the correlation we assumed in the sample size calculation was much lower (0.35) than the correlations found in the study (all of which were greater than 0.5). Similarly, the analysis of validity also found strong correlations (all greater than 0.7), so our convenience sample had statistical power for the assumed estimate.
On the other hand, the retrospective assessment of sleep involves a risk of recall bias. However, this limitation is intrinsic to any type of questionnaire, and the BISQ-E has the advantage of being simpler to implement compared to other sleep assessment methods that are prospective and more objective, which makes it particularly suitable for screening at the population level. Given that the evidence in the literature demonstrates that collection of information from parents is an effective method to detect behavioural and sleep problems in children,1,19 we consider the subjective assessments of families highly relevant.
In conclusion, the results of our study allow us to assert that the BISQ-E is a valid and reliable instrument for the assessment of sleep in Spanish children. This questionnaire can be useful for screening of sleep disorders in clinical practice and in epidemiological research.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cassanello P, Díez-Izquierdo A, Gorina N, Matilla-Santander N, Martínez-Sanchez JM, Balaguer A. Adaptación y estudio de propiedades métricas de un cuestionario de valoración del sueño para lactantes y preescolares. An Pediatr (Barc). 2018;89:230–237.
Previous presentation: Parts of this study were presented as an oral communication at the 65th Congress of Sociedad Española de Pediatría; June 1–3, 2017; Santiago de Compostela, Spain.