Multisystem inflammatory syndrome in children (MIS-C), first described in May 2020, is characterised by a significant inflammatory process with features similar to those of Kawasaki disease. Although the causal relationship has yet to be established, this syndrome exhibits a temporal association with the SARS-CoV-2 pandemic, and in most cases manifests in the context of past or recent infection by this virus.1
There is a dearth of data on cases of MIS-C. Although gastrointestinal symptoms are frequent in affected paediatric patients, there are few data and the literature is scarce on the subject of acute pancreatitis in patients with MIS-C.2–5
We present the case of a boy aged 10 years that presented to the emergency department of a tertiary care hospital with pain in the right abdomen accompanied by vomiting and fever of 9 days’ duration. The patient had an unremarkable previous history other than the diagnosis in the preceding month of acute SARS-CoV-2 infection confirmed by PCR in the context of a self-limited febrile illness. The physical examination revealed generalised macular rash, cracked red lips, bilateral non-suppurative conjunctival injection and abdominal pain with guarding at the level of the right iliac fossa. The patient underwent abdominal ultrasound and computed tomography scans, which did not reveal features compatible with acute abdomen or any other intraabdominal abnormalities, including the region of the pancreas. Blood tests evinced leucocytosis with neutrophilia and marked elevation of cardiac enzymes (Table 1). This prompted performance of an echocardiogram that revealed dilatation of the left coronary artery and mild pericardial effusion. The clinical and laboratory features were indicative of Kawasaki-like MIS-C attributed to coronavirus 2019 disease (COVID-19) due to detection of IgG antibodies against SARS-CoV-2, leading to initiation of treatment with intravenous immunoglobulin and acetylsalicylic acid at an anti-inflammatory dose.
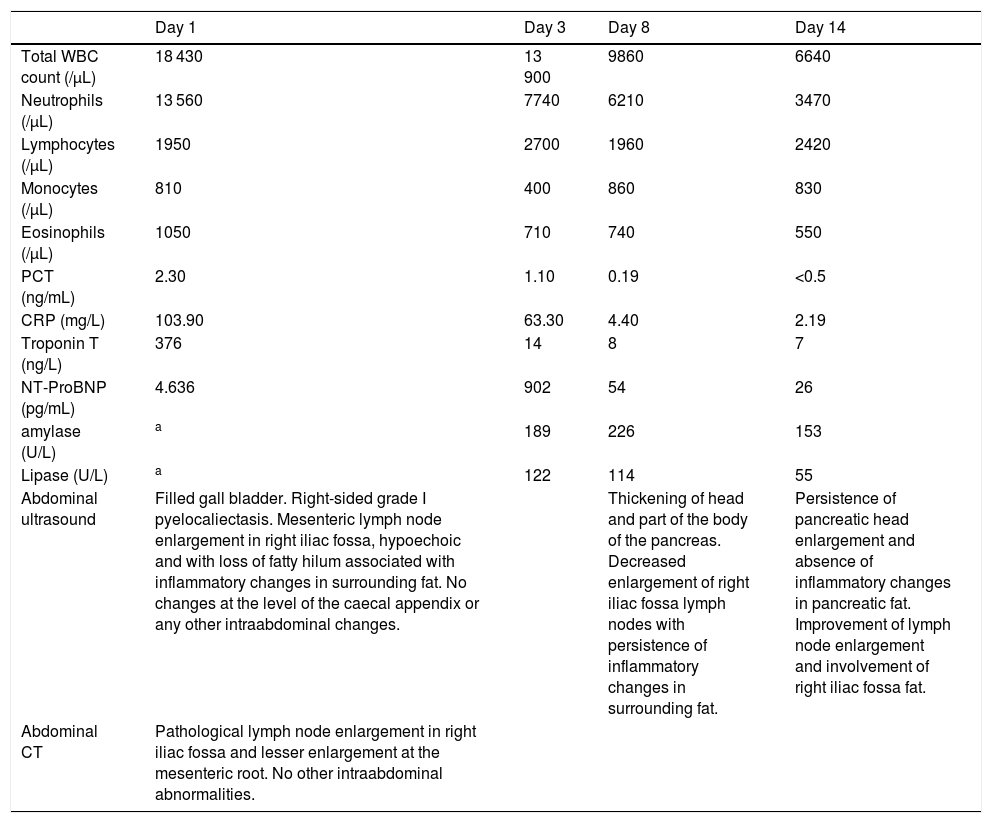
Diagnostic tests performed during the hospital stay of the patient with MIS-C associated with a past SARS-CoV-2 infection.
| Day 1 | Day 3 | Day 8 | Day 14 | |
|---|---|---|---|---|
| Total WBC count (/µL) | 18 430 | 13 900 | 9860 | 6640 |
| Neutrophils (/µL) | 13 560 | 7740 | 6210 | 3470 |
| Lymphocytes (/µL) | 1950 | 2700 | 1960 | 2420 |
| Monocytes (/µL) | 810 | 400 | 860 | 830 |
| Eosinophils (/µL) | 1050 | 710 | 740 | 550 |
| PCT (ng/mL) | 2.30 | 1.10 | 0.19 | <0.5 |
| CRP (mg/L) | 103.90 | 63.30 | 4.40 | 2.19 |
| Troponin T (ng/L) | 376 | 14 | 8 | 7 |
| NT-ProBNP (pg/mL) | 4.636 | 902 | 54 | 26 |
| amylase (U/L) | a | 189 | 226 | 153 |
| Lipase (U/L) | a | 122 | 114 | 55 |
| Abdominal ultrasound | Filled gall bladder. Right-sided grade I pyelocaliectasis. Mesenteric lymph node enlargement in right iliac fossa, hypoechoic and with loss of fatty hilum associated with inflammatory changes in surrounding fat. No changes at the level of the caecal appendix or any other intraabdominal changes. | Thickening of head and part of the body of the pancreas. Decreased enlargement of right iliac fossa lymph nodes with persistence of inflammatory changes in surrounding fat. | Persistence of pancreatic head enlargement and absence of inflammatory changes in pancreatic fat. Improvement of lymph node enlargement and involvement of right iliac fossa fat. | |
| Abdominal CT | Pathological lymph node enlargement in right iliac fossa and lesser enlargement at the mesenteric root. No other intraabdominal abnormalities. |
During the stay, the patient exhibited significant improvement of clinical manifestations and laboratory markers with pharmacological treatment (Table 1).
However, on day 8 of the stay, the patient developed abdominal pain that radiated from the epigastrium. This prompted the performance of an abdominal ultrasound scan that revealed thickening of the head and body of the pancreas and blood tests that evinced elevation of pancreatic enzymes (Table 1). These findings, combined with the compatible manifestations, met the Arkansas criteria for acute pancreatitis (imaging features compatible with pancreatic involvement, elevation of pancreatic enzymes and abdominal pain in the left hypochondrium/epigastrium). The patient exhibited clinical, laboratory and sonographic improvement in successive follow-up evaluations after conservative management with a soft food diet and partial bed rest, without requiring specific treatment of the pancreatitis. The patient stayed in the inpatient ward for 15 days.
To date, few authors have reported acute pancreatitis in paediatric patients with MIS-C.3–5
The association between acute pancreatitis and SARS-CoV-2 and its pathophysiological mechanism remain unknown. Several studies support the hypothesis of indirect involvement of the pancreas after the virus comes into contact with angiotensin-converting enzyme 2 (ACE2) receptors in pancreatic tissue, although further research is needed to establish the association between acute pancreatitis and SARS-CoV-2 infection in children.6
We need more data for the paediatric population to investigate this new syndrome and its potential complications.
Please cite this article as: Traba Zubiaurre M, Eizaguirre Arocena FJ, Urrutikoetxea Aiartza M, Izquierdo Iribarren A. Pancreatitis aguda en paciente pediátrico afecto de síndrome inflamatorio multisistémico atribuido a COVID-19. An Pediatr. 2022;96:270–272.