Recent studies published in Anales de Pediatría have described the impact of the COVID-19 (coronavirus disease 2019) pandemic on the incidence of asthma exacerbations and bronchiolitis in the paediatric emergency department (PED) setting.1,2 However, there is no evidence on its impact on the incidence of acute laryngitis (AL) episodes and their severity.
We conducted a retrospective, cross-sectional study of episodes of AL managed in a PED between January 2018 and December 2022. We analysed the monthly visits due to AL, identified based on code J04.0 of the ICD-10 (International Classification of Diseases 10th Revision) in the records, and the number of hospital admissions. In addition, we compared the characteristics of the episodes of AL in the epidemic seasons before and after the pandemic: clinical presentation, treatment and outcome. To carry out this comparison, we obtained a stratified random sample. The statistical analysis was performed with the STATA software, version17. The protocol for the management of AL at the PED did not change during the study period.
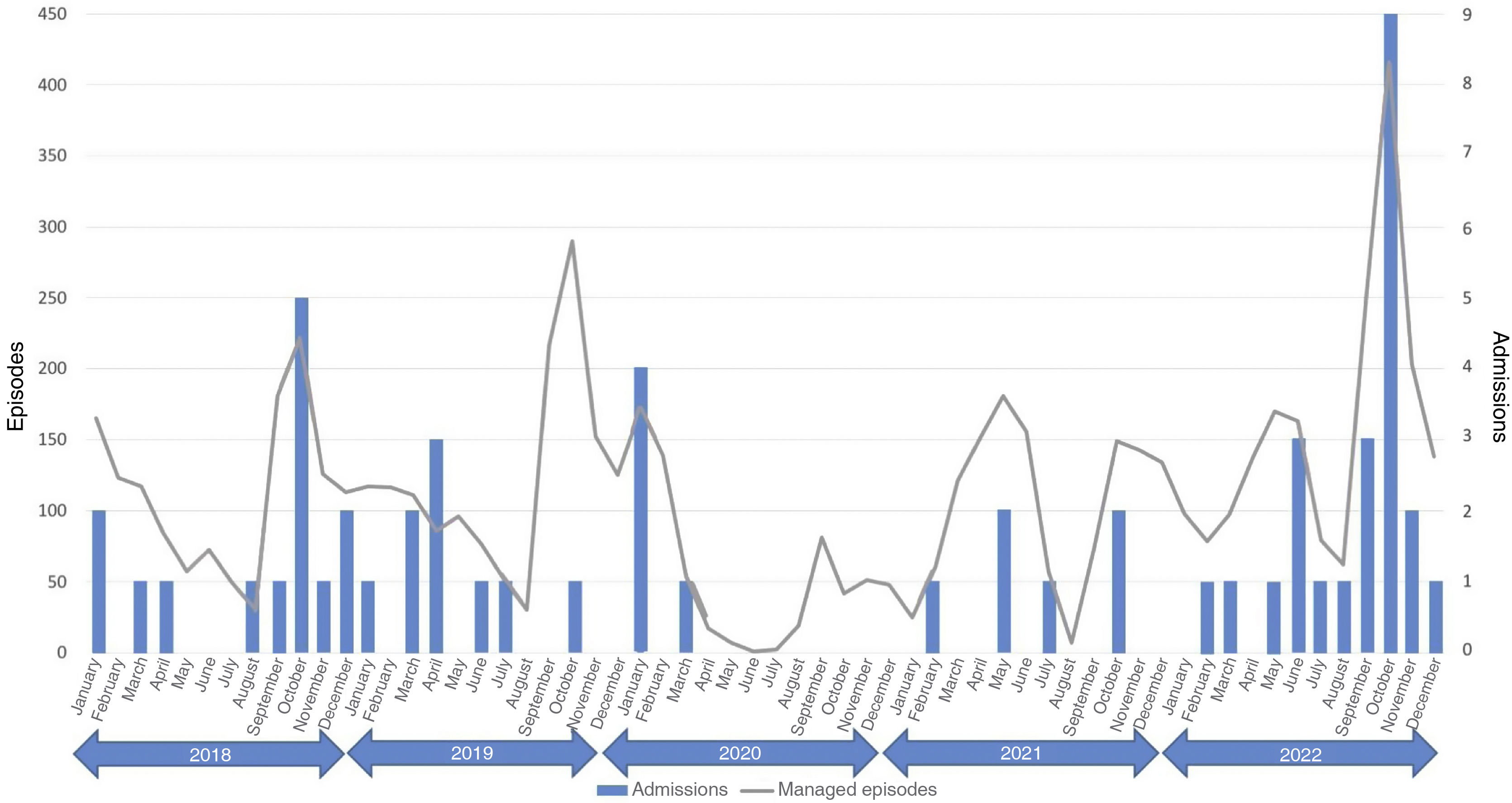
In the five years under study, there were 3 epidemic seasons (Fig. 1). Two took place before the COVID-19 pandemic (September–October 2018 and September–October 2019) and one after (September–October 2022). The number of managed AL episodes was greater in the 2022 season (2018: 404 episodes of AL [3.8% of total episodes of care]; 2019: 507 episodes [4.8% of total]; 2022: 669 episodes [5.1% of total]). In the analysis, we included 601 episodes (37.8% of total episodes of AL managed at the PED).
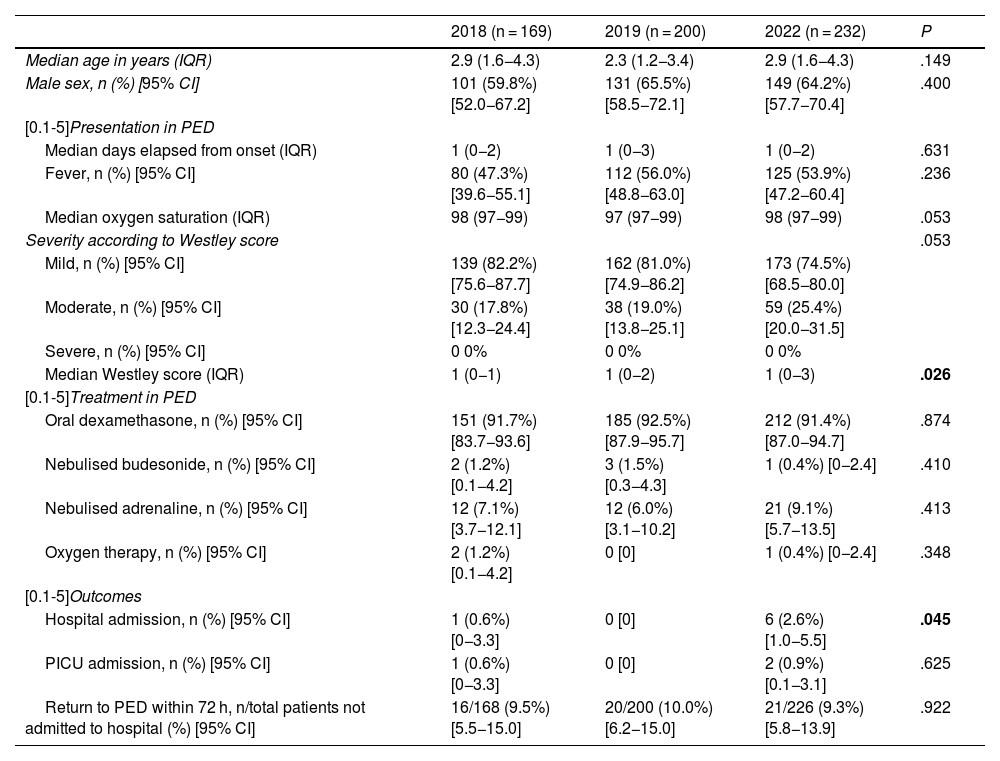
Table 1 presents the results of the comparison of the characteristics of the episodes of AL managed before and after the COVID-19 pandemic. The median Westley score was greater in the first AL epidemic season following the COVID-19 pandemic, as was the rate of hospital admission.
Comparison of demographic and clinical characteristics, treatment and outcomes of episodes of acute laryngitis managed at the PED in the period under study (2018-2022).
| 2018 (n = 169) | 2019 (n = 200) | 2022 (n = 232) | P | |
|---|---|---|---|---|
| Median age in years (IQR) | 2.9 (1.6−4.3) | 2.3 (1.2−3.4) | 2.9 (1.6−4.3) | .149 |
| Male sex, n (%) [95% CI] | 101 (59.8%) [52.0−67.2] | 131 (65.5%) [58.5−72.1] | 149 (64.2%) [57.7−70.4] | .400 |
| [0.1-5]Presentation in PED | ||||
| Median days elapsed from onset (IQR) | 1 (0−2) | 1 (0−3) | 1 (0−2) | .631 |
| Fever, n (%) [95% CI] | 80 (47.3%) [39.6−55.1] | 112 (56.0%) [48.8−63.0] | 125 (53.9%) [47.2−60.4] | .236 |
| Median oxygen saturation (IQR) | 98 (97−99) | 97 (97−99) | 98 (97−99) | .053 |
| Severity according to Westley score | .053 | |||
| Mild, n (%) [95% CI] | 139 (82.2%) [75.6−87.7] | 162 (81.0%) [74.9−86.2] | 173 (74.5%) [68.5−80.0] | |
| Moderate, n (%) [95% CI] | 30 (17.8%) [12.3−24.4] | 38 (19.0%) [13.8−25.1] | 59 (25.4%) [20.0−31.5] | |
| Severe, n (%) [95% CI] | 0 0% | 0 0% | 0 0% | |
| Median Westley score (IQR) | 1 (0−1) | 1 (0−2) | 1 (0−3) | .026 |
| [0.1-5]Treatment in PED | ||||
| Oral dexamethasone, n (%) [95% CI] | 151 (91.7%) [83.7−93.6] | 185 (92.5%) [87.9−95.7] | 212 (91.4%) [87.0−94.7] | .874 |
| Nebulised budesonide, n (%) [95% CI] | 2 (1.2%) [0.1−4.2] | 3 (1.5%) [0.3−4.3] | 1 (0.4%) [0−2.4] | .410 |
| Nebulised adrenaline, n (%) [95% CI] | 12 (7.1%) [3.7−12.1] | 12 (6.0%) [3.1−10.2] | 21 (9.1%) [5.7−13.5] | .413 |
| Oxygen therapy, n (%) [95% CI] | 2 (1.2%) [0.1−4.2] | 0 [0] | 1 (0.4%) [0−2.4] | .348 |
| [0.1-5]Outcomes | ||||
| Hospital admission, n (%) [95% CI] | 1 (0.6%) [0−3.3] | 0 [0] | 6 (2.6%) [1.0−5.5] | .045 |
| PICU admission, n (%) [95% CI] | 1 (0.6%) [0−3.3] | 0 [0] | 2 (0.9%) [0.1−3.1] | .625 |
| Return to PED within 72 h, n/total patients not admitted to hospital (%) [95% CI] | 16/168 (9.5%) [5.5−15.0] | 20/200 (10.0%) [6.2−15.0] | 21/226 (9.3%) [5.8−13.9] | .922 |
CI, confidence interval; IQR, interquartile range; PED, paediatric emergency department.
Figures presented in boldface correspond to statistically significant results.
When it came to the microbiological characteristics of the 12 patients admitted for AL in September–October 2022, none tested positive for SARS-CoV-2 with either the rapid antigen test or the polymerase chain reaction test. A respiratory virus panel test was carried out in 3 cases, with detection of parainfluenza virus type 1/rhinovirus coinfection in one patient, parainfluenza virus type 2/rhinovirus coinfection in another and infection by parainfluenza virus type 2 in the remaining patient.
The strict hygiene and public health measures implemented to contain the COVID-19 pandemic have brought on changes in the presentation of some diseases. It has been hypothesised that these measures may have resulted in an “immunity debt” that in turn has allowed the development of more intense and severe respiratory infections, both viral and bacterial.3 In the past, the annual AL season typically occurred in the autumn months and was associated with human parainfluenza viruses. In our hospital, in the first AL season following the COVID-19 pandemic, the absolute frequency of episodes was greater compared to previous seasons and, for the first time since statistics started to be calculated, AL was one of the 10 most frequent diagnoses at the PED.
In the epidemic seasons under study, there was no documented case of severe AL, probably because we stratified patients based on the Westley score, an instrument that requires the presence of cyanosis or an altered level of consciousness in the examination to classify the episode as severe.4 However, the patients managed during the first AL season after the COVID-19 pandemic did have higher Westley scores. This was associated with an increased rate of admission, although the impact in the inpatient care setting was small, as most cases could be managed at the outpatient level.
Since in our PED microbiological testing is only performed in patients who require admission, we were unable to assess the impact of SARS-CoV-2 throughout the epidemic season. The omicron variant has been associated with an increase in the incidence of AL caused by SARS-CoV-2 compared to previous variants of the virus.5 Whether AL episodes caused by SARS-CoV-2 tend to be more severe compared to episodes of a different aetiology is still under debate.5,6 In our hospital, during the epidemic season that we analysed, none of the patients who required admission tested positive for SARS-CoV-2.
Despite the limitations intrinsic to a study with a retrospective design conducted in a single centre, it would be reasonable to conclude that the immunity debt incurred with the implementation of measures to contain the COVID-19 pandemic may have also affected the clinical presentation of AL cases, as has been observed in other respiratory infections. However, the impact on the health care system was limited, as most cases could be managed at the outpatient level.
FundingThis research did not receive any external funding.
Previous meeting: this study was presented as a poster at the XXVII Meeting of the Sociedad Española de Urgencias Pediátricas; May 18–20, 2023; Las Palmas de Gran Canaria, Spain.