Teachers may have an essential role in basic life support (BLS) training in schoolchildren. However, few data are available about their BLS learning abilities.
AimTo quantitatively assess the quality of BLS when performed by school teachers after a brief and simple training program.
Materials and methodsA quasi-experimental study with no control group and involving primary and secondary education teachers from four privately managed and public funded schools was conducted in three stages: (1) a knowledge test, (2) BLS training, and (3) performance test. Training included a 40-min lecture and 80-min hands-on session with the help of feedback on the quality of the chest compressions.
ResultsA total of 81 teachers were included, of which 60.5% were women. After training, the percentage of subjects able to perform the BLS sequence rose from 1.2 to 46% (p<0.001). Chest compression quality also improved significantly in terms of: correct hands position (97.6 vs 72.3%; p<0.001), mean depth (48.1 vs 38.8mm; p<0.001), percentage that reached recommended depth (46.5 vs 21.5%; p<0.001), percentage of adequate decompression (78.7 vs 61.2%; p<0.05), and percentage of compressions delivered at recommended rate (64.2 vs 26.9%; p<0.001).
ConclusionsAfter a brief and simple training program, teachers of privately managed public funded schools were able to perform the BLS sequence and to produce chest compressions with a quality similar to that obtained by staff with a duty to assist cardiac arrest victims. The ability of schoolteachers to deliver good-quality BLS is a pre-requisite to be engaged in BLS training for schoolchildren.
Los profesores pueden tener un papel esencial en la formación en reanimación cardiopulmonar básica (RCP-B) de los escolares. Sin embargo, se dispone de pocos datos acerca de la capacidad de aprendizaje de la RCP-B por estos profesionales.
ObjetivoEvaluar de forma cuantitativa la calidad de la RCP-B realizada por profesores de colegios, tras un programa formativo breve y sencillo.
Material y métodosSe realizó un estudio cuasiexperimental sin grupo control en el que participaron profesores de cuatro centros concertados de educación infantil, primaria y secundaria, en 3 fases: 1.a de evaluación de conocimientos, 2.a de formación en RCP-B y 3.a de evaluación de las competencias. La formación consistió en una sesión teórica de 40min y otra práctica de 80min, con ayuda de maniquís con sistema de retroalimentación de la calidad de las compresiones torácicas.
ResultadosSe incluyeron 81 profesores (60,5% mujeres). Tras la formación, el porcentaje de sujetos que realizaron bien la secuencia de RCP-B aumentó de 1,2% a 46% (p<0,001). La calidad de las compresiones torácicas también mejoró significativamente en cuanto a: posición correcta de las manos (97,6 vs 72,3%; p<0,001), profundidad media (48,1 vs 38,8mm; p<0,001), porcentaje que alcanzó la profundidad recomendada (46,5 vs 21,5%; p<0,001), porcentaje de descompresiones adecuadas (78,7 vs 61,2%; p<0,05), y porcentaje de compresiones realizadas al ritmo recomendado (64,2 vs 26,9%; p<0,001).
ConclusionesTras un programa sencillo y breve, los profesores de colegios concertados son capaces de realizar la secuencia de RCP-B y aplicar las compresiones torácicas con una calidad comparable a la de colectivos con el deber de asistir a una víctima de una parada cardíaca. La comprobación de la capacidad de estos profesionales para hacer una RCP-B de calidad es el primer requisito para que puedan implicarse en la enseñanza de la RCP-B a los escolares.
Performance of basic cardiopulmonary resuscitation (B-CPR) by witnesses of the event is the cornerstone of survival in out-of-hospital cardiac arrest. In spite of this, in developed countries, bystanders start CPR in fewer than 30% of witnessed cardiac arrests.1 For this reason, the American Heart Association (AHA)2 and the European Resuscitation Council (ERC)3 advocate for training the entire population in order to enable a quick and effective response to out-of-hospital cardiac arrest (CA) and improve its outcomes. It is estimated that early CPR performed by a bystander can double or triple the probability of survival in individuals that suffer a CA.4
At present, while there is widespread agreement regarding the need to teach B-CPR in schools5 and both the ERC and the AHA support its inclusion in the academic curriculum, several aspects are under debate regarding this approach (who should provide the training? to whom? how? when? etc.). Some countries, such as Norway,6 have been teaching CPR in schools for many years. Spain also joined this initiative with Royal Decree 126/2014, which included first-aid skills in the primary education curriculum,7 but in reality these skills are seldom taught,8,9 partly because there are no established programs to train teachers to this end.
Therefore, it is essential to include teachers in the BLS education chain, teaching them what they need to know and confirming that they can perform the BLS sequence correctly so that they can be appropriate models.
Teaching CPR in schools is a strategy that allows access to nearly the entire future population, and it is perceived positively by educators,10,11 who feel capable of teaching children life support concepts and techniques if they have previously received adequate training.12 Training by teachers would facilitate the delivery of life support education13 and may be more efficient than education provided by other facilitators.14,15
The aim of our study was to make a quantitative assessment of the extent to which secondary teachers learned the BLS sequence and life support skills after a brief training program.
Materials and methodsIn the framework of the ANXOS project on teaching B-CPR to children and adolescents, we performed a quasi-experimental study without a control group in a convenient sample. The study was approved by the Ethics Committee of the School of Education and Sports Sciences of the University of Vigo. The sample included 81 teachers (49 female) of early childhood, primary and secondary education employed in four publicly-funded and privately-run schools in the Autonomous Community of Galicia who voluntarily chose to participate in the training. After explaining the objectives and procedures involved in the study, we obtained the authorization of the management of each school and the informed consent of the teachers that participated.
The study comprised three phases. In the initial phase, we collected the following data for each participant: sex, age, weight, height, body mass index, and educational stage and subject taught by the participant. This was followed by an assessment of baseline knowledge by means of an ad hoc questionnaire and of their basic life support (BLS) skills. Teachers were asked to fill out a questionnaire reporting whether they had received training in BLS in the past, which kind and their level of knowledge, then answer a total of 15 questions that addressed aspects related to the chain of survival. In addition to this assessment of their knowledge, participants underwent a B-CPR simulation test with a manikin. They had to simulate the steps that need to be taken in CPR, culminating with a performance of 2min of hands-only CPR (HO-CPR).
The second phase consisted of training the participants. The teachers attended a 2-h training on BLS. The training was divided into two parts: one theoretical and one practical. The theoretical part lasted 40min during which the instructors explained each step in the chain of survival. The practical part lasted 80min, during which the participants practiced the steps for CPR on a standard manikin with the support of the instructors. In addition, each participant performed 6min (in 2-min cycles) of HO-CPR on a manikin that generated visual feedback on the participant's execution. The instructor-to-participant ratio was 1:6 and the manikin-to-participant ratio was 1:3. The instructors that trained the teachers were BLS instructors accredited by the ERC.
In the third and last phase, participants were evaluated following the procedure of the first phase, 2h after completing the training phase. They filled out the initial questionnaire again and simulated the performance of CPR on a manikin, delivering 2min of HO-CPR.
When it came to simulation with manikins, we assessed the correct execution of the BLS sequence and the quality of HO-CPR. To assess the execution of the sequence, we recorded whether participants ensured the safety of every individual at the scene, checked the victim's response, opened the airway, checked for breathing, called emergency services, and started chest compressions. The time elapsed between the presentation of the case and initiation of compressions was also recorded. We assessed the quality of CPR by means of the manikins (Laerdal Resusci Anne manikin with wireless SkillReporter software for PC version 12.0.0.2), which provide real-time feedback set to the European guidelines of 2015 (depth of compression, 50–60mm; compression rate, 100–120 compressions/min). We established an arbitrary cut-off of 70%, which some experts have proposed as an adequate cut-off point for the assessment of CPR quality.16 This was also the manikin model used for practice with real-time feedback during the training phase.
Statistical analysisWe have expressed qualitative variables as absolute and relative frequencies. We summarized quantitative variables through measures of central tendency and dispersion (mean and standard deviation [SD]).
To analyze the association between categorical variables, we used the Pearson chi square test, while we used the McNemar test to compare pre- and post-testing proportions. We analyzed the quantitative variables associated with the quality of resuscitation by means of repeated-measures ANOVA. The analysis of variance included two factors: a between-subject factor (with vs without previous training) and a within-subject factor (pre- vs post-training).
We analyzed the data with the Statistical Package for the Social Sciences® (SPSS) version 20.0. A p-value <0.05 is defined statistically significant in any of the tests.
ResultsThe total number of teachers in the schools included in the study was 294. Of those, 87 (29.6%) participated in the study. We excluded 6 teachers due to incomplete data, resulting in a final sample of 81 teachers (60.5% females). Their mean age was 43.5 years (SD, 10.1), their mean weight was 73.5kg (SD, 15.3), their mean height was 167.9cm (SD, 8.1), and their mean BMI was 25.9kg/m2 (SD, 4.4).
The participants taught humanities (40.7%), sciences (22.0%), several subjects (27.1%), and physical education (17.2%). As for the educational stage, 46.2% were employed in primary education, 41% in compulsory secondary education (ESO), and 12.8% in early childhood education.
Of all participants, 28.4% reported having received some training on B-CPR in the past, face-to-face and with theoretical and practical components. All participants (with and without previous training) rated their own knowledge of B-CPR as low to very low.
Before training, only 1.2% were able to correctly perform the BLS sequence. After training, this percentage had risen to 46.2%.
As to their theoretical knowledge, the mean number of correct answers in the baseline questionnaire was 3.7 (SD, 2.8), which rose to 8 correct answers in the post-training test (SD, 1.9).
Fig. 1 shows how teachers improved significantly in every element of the sequence: ensuring rescuer, victim, and bystander safety (1.2% vs 53.8%; p<0.001); checking victim's responsiveness (29.6% vs 96.2%; p<0.001), opening airway with the head tilt and chin lift technique (24.7% vs 52.6%; p=0.021); looking, listening, and feeling for breathing (50.6% vs 96.0%; p<0.001), alerting emergency medical services (EMS) (50.6% vs 94.9%; p<0.001), and starting chest compressions (42.0% vs 98.7%; p<0.001).
Fig. 1 summarizes the data pertaining to the quality of chest compressions. When it came to the overall quality of compressions (QCPR), prior to training, only 18.5% of participants passed the 70% correct compressions threshold considered indicative of quality.16 After training, 63.2% delivered CPR that passed the 70% correct compression threshold (p<0.001), with the mean rising from 23.5±30.8 to 69.1±31.5% (p<0.001). Teachers improved significantly in the following variables: correct hand position (70.0±43.1 vs 97.6±12.2%; p<0.001); mean compression depth (38.1±2.5 vs 48.0±9.4mm; p<0.001), with increases in the percentage of correct compressions in terms of depth (19.4±30.8 vs 45.0± 37.3%; p<0.001) and of the teachers that achieved depths of 50–60mm (22.4 vs 42.1%; p=0.003); percentage of compressions with correct chest recoil (61.8±38.1% vs 78.7±30.0%; p=0.004), and percentage of compressions delivered at an adequate rate (26.8±35.5 vs 65.0±36.6%; p<0.001).
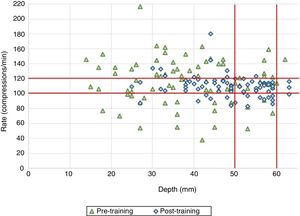
Compression rate also improved with training, as the percentage of teachers that achieved the recommended target of 100–120 compressions/min increased from 28.9 to 67.1% (p<0.001). Thus, as can be seen in Fig. 2, the percentage of teachers that achieved an adequate quality of compressions in terms of depth (50–60mm) and rate (100–120 compressions/min) increased after training (10.5 vs 28.9%; p=0.007).
We also compared the quality of CPR based on time (pre- vs post-training) and previous CPR training (with or without).
When we compared teachers with previous training and teachers without a baseline, we only found statistically significant differences in the overall quality of resuscitation and the mean compression depth. While previously trained teachers also performed better in the rest of the resuscitation variables, the differences were not statistically significant. Following the training that was the subject of this study, both groups of teachers improved significantly in every analyzed variable except the chest compression fraction and the mean compression rate. The group with previous training did not improve significantly in the percentage of compressions followed by correct chest recoil or in correct hand placement, although their performance did improve. Although the overall quality of CPR was higher in the group with previous training, the improvements observed in resuscitation variables led to the absence of statistically significant differences in any variable between groups after the training.
DiscussionOur study demonstrates that school teachers, most of them without previous training or minimal knowledge of life support, were able to perform the BLS sequence with a quality comparable to that observed in health professionals after a brief and simple training program.17–19 Considering that teachers are the individuals that have the pedagogical skills required to teach children effectively, we must guarantee that they have the necessary educational “foundation” to do so, and considering that the number of teachers that needs training is very high, it is important to develop and implement a standardized and brief training program for this collective.
Previous studies have investigated the role of teachers as CPR and first aid instructors and found not only that teachers are effective at teaching CPR12,13,20–22 and believe that children should be taught these skills,10 but also a good correlation between learning outcomes and the instructor's profession.23 Thus, our findings should serve as encouragement to implement similar training programs in other geographical areas with the ultimate goal of achieving the necessary critical mass of skilled teachers to turn universal school-based BLS education into a reality in Spain.
To guarantee adequate teaching of BLS, teachers must know the BLS sequence and be able to demonstrate high-quality CPR. Key points must be emphasized during the training process, such as knowledge of the emergency services number, how to identify CA, and how to determine when and how to contact emergency services, as the latest guidelines of the ERC24 recommend that emergency dispatch centers assist CPR by phone, providing rescuers with information and guidance on how to deliver BLS.
As for knowledge of the BLS sequence, in our study, teachers achieved a lower percentage of correct answers (61.5 vs 76.63%) in the knowledge assessment questionnaire20 and rated similarly in the performance of the BLS sequence except in ensuring the safety of the scene and opening the airway, where the percentages were higher.25 The methodology of these studies differed with ours, mainly in the duration of training, which poses barriers to comparing results.
In its 2015 guidelines,24 the ERC underscores the importance of delivering effective chest compressions, recommending a depth of approximately 5cm and no more than 6cm, a compression rate of 100–120 compressions/min with as few interruptions as possible, and allowing the chest to recoil completely after each compression. We ought to note that very few people, including health professionals, are able to exceed this rate even for short periods of time (<5min).17
When we compared the outcomes in compression quality with the outcomes of similar studies, we found that in our study, 67.1% of teachers achieved an adequate compression rate, a proportion that significantly exceeded the proportion reported by Lukas et al. (34.2%),20 with a mean rate of 91.8±5.0 compressions/min; 42.1% of teachers achieved an adequate mean depth, which was also higher compared to proportion that achieved it in the study by Lukas et al. (11.93%),20 while the remaining teachers had mean depths exceeding 6cm (3.9%) or below the recommended 5cm (53.9%) (Fig. 2). The depth achieved is associated with physical fitness or strength,26 and the mean depth can be improved through retraining. The outcomes in our study did not fall too short of the target, something that may be improved by increasing the duration of training. We also observed that the mean percentage of compressions with adequate chest recoil was lower than those reported in the reviewed literature (90.917 and 87.5%)18, although it was still acceptable.
When it came to the effect of previous training in teachers, we found that teachers with previous training delivered 25% more of correct compressions and compressions that were 7mm deeper on average compared to teachers with no previous training. After training, the overall compression quality improved, with 63.2% achieving adequate quality of compressions overall (taking into consideration all CPR quality variables), while those that did not achieve quality compressions (36.8%) achieved significantly greater mean depths and significantly lower values in all other parameters under study.
Based on these outcomes, any teacher, even those that have never been exposed to life support in the past, would benefit of training of the sort proposed in this study and would be able to teach BLS to their students fairly easily.
The method we employed for training was practical simulation with feedback, similar to the approach used in studies of chest compression quality.17,25–28 The time devoted to practical training was of approximately 5min per participant, similar to the time invested in the study by González-Salvado et al.17 While this duration is brief, it sufficed to improve skills, which suggests that short CPR training programs may be useful and feasible, facilitating access to and increasing the motivation for BLS training, as already noted by Wang et al.29
We observed that retention of CPR skills is poor, as they may deteriorate in as short a time as 6 weeks,25–30 which makes retraining indispensable.31 For this reason, the teachers trained in this project will be offered the chance to receive refresher trainings before they start teaching CPR, supported by the storage of quantitative data of the Laerdal SkillReporter® feedback software, which allows comparison with previous performance for improvement through regular retraining.
There are some limitations to our study, such as the potential biases associated with the level of motivation of participants at the time of training, the physical fitness of teachers (as they taught different subjects), and the fact that all teachers were employed in publicly-funded private schools, as there is evidence that student retention varies between public and private schools.32 These aspects do not render our results invalid, but must be taken into account to avoid direct extrapolation to other teacher populations, such as teachers employed in public schools. Furthermore, since we used a novel evaluation tool calibrated according to the targets proposed in international guidelines from 2015, our results cannot be directly compared to those of previous studies that used different tools for measurement and applied different criteria to assess the quality of CPR.
In conclusion, the early, primary, and secondary education teachers in the participating schools had poor knowledge and skills to deliver adequate BLS, but following a brief and simple training they were able to perform the BLS sequence correctly and apply chest compressions of a quality comparable to that observed in other collectives with a “duty of care” toward CA victims.
Our results suggest that training teachers on BLS, which is essential for them to be able to train their students, is feasible with short material and time resources, which should encourage routine training of these professionals to achieve the goal of universal school-based BLS training.
Conflict of interestThe authors have no conflicts of interest to declare.
Please cite this article as: López MP, Martínez-Isasi S, Barcala-Furelos R, Fernández-Méndez F, Santamariña DV, Sánchez-Santos L, et al. Un primer paso en la enseñanza del soporte vital básico en las escuelas: la formación de los profesores. An Pediatr (Barc). 2018;89:265–271.