The minimally invasive approach is seldom reported in paediatric cardiac surgery. Teams gathering experience are scarce, with programmes focused on simple cases. The experience is presented on a series of over 200 cases operated on in the past 15 years.
Material and methodsA sub-mammary approach programme was started in 2000, which was gradually extended to include more complex and younger patients. The axillary incision was adopted in 2009, following the same steps. In 2013, the mini-sternotomy incision was introduced, increasing our armamentarium. From July 2000 until December 2014, 203 patients were operated on. The sub-mammary approach was used in 102 cases, axillary in 50 patients, mini-sternotomy in 44, postero-lateral thoracotomy in 4 cases, and upper mini-sternotomy in 3.
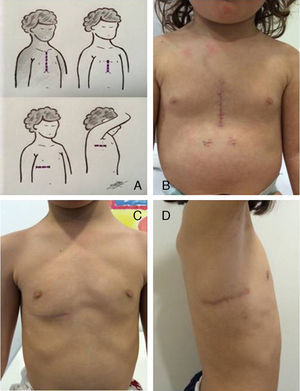
ResultsBy diagnosis, ostium secundum atrial septal defect was the most common (128), followed by sinus venosus (20), ventricular septal defect (20), ostium primum (16), and others (19). One patient was converted to sternotomy. No neurological events were detected. The mean age was 7.8/3.7 and 1.8 years, and the mean weight was 28.1/16.1 and 9.4kg, in the sub-mammary, axillary and mini-sternotomy approaches, respectively. The aesthetic results were excellent.
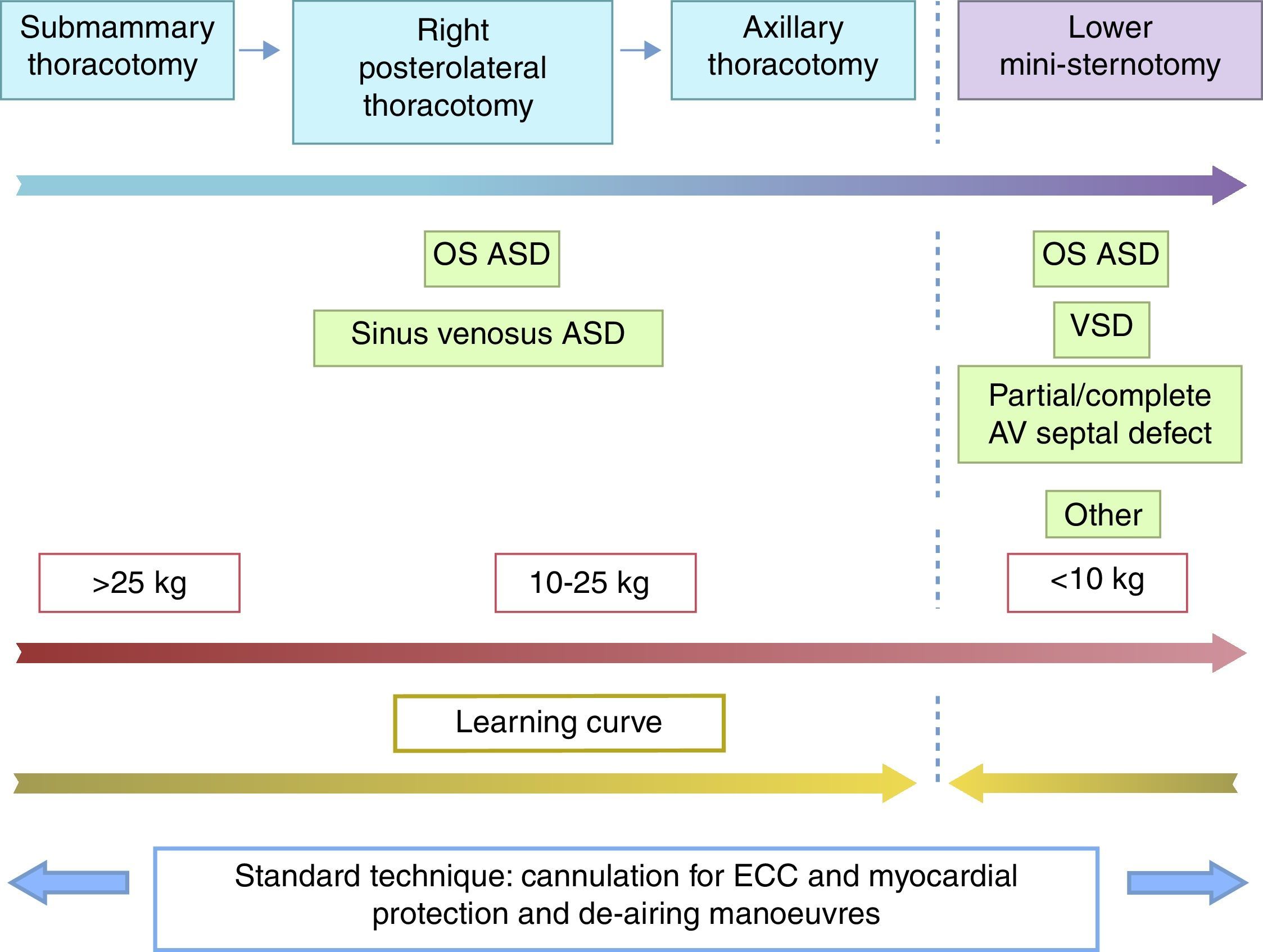
ConclusionsBased on our 15 years of experience, minimally invasive surgery is safe and yields excellent cosmetic results. The gradual introduction of alternative approaches (sub-mammary, axillary, mini-sternotomy) allowed us to set-up guidelines and learning curves. The wide range of incisions enables the most appropriate one to be selected depending on age/weight and cardiac condition.
Los abordajes miniinvasivos en cirugía cardiaca infantil no son habituales. Pocos grupos presentan programas y experiencia, quedando limitados a cardiopatías simples. Presentamos una casuística recopilada a lo largo de 15 años y más de 200 pacientes.
Material y métodosEn el año 2000 comenzamos un programa de acceso submamario, ampliándolo progresivamente a casos complejos y edades menores. En 2009 incorporamos el abordaje axilar, con idénticas pautas. En 2013 iniciamos la cirugía por miniesternotomía inferior, ampliando la cartera de servicios. Entre julio del 2000 y diciembre del 2014 se intervino a 203 pacientes: 102 por vía submamaria, 50 por axilar, 44 por miniesternotomía inferior, 4 por toracotomía lateral-posterior y 3 por miniesternotomía superior.
ResultadosPor patologías, la más frecuente fue la comunicación interauricular ostium secundum (128), seguida del seno venoso (20), comunicación interventricular (20), ostium primum (16) y otras (19). Un caso fue reconvertido a esternotomía. No hubo eventos neurológicos. Las medias de edad fueron 7,8/3,7 y 1,8 años, con medias de peso de 28,1/16,1 y 9,4kg en los accesos submamario, axilar y miniesternotomía, respectivamente. Los resultados estéticos han sido excelentes.
ConclusionesTras 15 años de experiencia acumulada, la cirugía miniinvasiva es segura y eficaz, con resultados estéticos excelentes. La introducción gradual de diferentes accesos alternativos permite establecer pautas de aprendizaje. La versatilidad de accesos (submamario, axilar, miniesternotomía) facilita la selección de abordajes en función de cardiopatía y edad/peso.
Due to the boom in interventional cardiology and the proliferation of techniques such as laparoscopy or thoracoscopy in other surgical specialties, several teams have adopted approaches alternative to median sternotomy.1–7 The initial enthusiasm, fuelled by the technical advances of the past twenty-five years, stood against the reticence of those with a traditional approach. Doubts regarding the complexity and operative time of the technique, as well as its outcomes, prevented minimally invasive surgery from becoming widely used in congenital heart disease.
The most common surgical approaches used as alternatives to complete median sternotomy are: lower mini-sternotomy,8–11 right anterolateral thoracotomy (submammary incision),1,12–16 right posterolateral thoracotomy,18 and right axillary thoracotomy.19–23 Their advantages are mainly cosmetic, although other advantages have been described, such as lower use of blood products, lower rate of infection, and faster recovery. On the other hand, the most common drawbacks are the technical complexity and learning curve of these procedures, longer duration of extracorporeal circulation and aortic cross-clamping, and difficulty performing myocardial protection and de-airing manoeuvres.
In this article, we present our experience of fifteen years comprehending more than 200 cases. We describe the patient selection and exclusion criteria, and the manoeuvres used to address the drawbacks we have just mentioned. We give detailed information on the various approaches we have used and also on the criteria used for expanding the indications of these procedures to more complex cases and younger patients. Patient safety was the main consideration at all times.
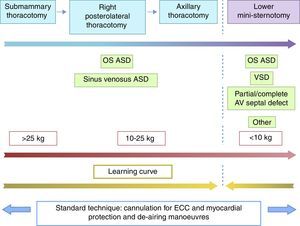
Materials and methodsIn year 2000, we launched a programme of minimally invasive paediatric heart surgery with submammary access. The first cases selected corresponded to female adolescents with developed breasts or a clearly defined inframammary fold with a diagnosis of ostium secundum (OS) atrial septal defect (ASD), having ruled out the presence of a left-sided superior vena cava (LSVC) and/or patent ductus arteriosus. A plastic surgeon assisted with accessing and closure of the thorax until we became familiar with the technique.16 In essence, the incision in the skin is made at the level of the submammary fold or sixth intercostal space, creating a pectoralis major myocutaneous flap24 to enter the thoracic cavity through the fourth intercostal space. Both cannulation and surgical repair are performed through this single access, with no auxiliary incisions. Later on, we expanded the indication to younger patients (male and female) and other diseases that could be approached through the right atrium, such as sinus venosus (SV) ASD or ostium primum (OP) ASD.
After operating on 71 cases through this technique, we incorporated the axillary approach in 2009. Several studies25,26 warned of potential deformities of the breast or dorsal region as a result of anterolateral thoracotomy, and the axillary incision gained advocatess.19–21 As a learning curve, we operated on several cases via posterolateral thoracotomy17,18 before “minimising” the incision towards the right axilla, sparing the latissimus dorsi and serratus.27 As was the case in the submammary approach, the entire procedure was performed through the axillary incision. Also consistent with the submammary approach, the initial indication for this approach was OS ASD, with the subsequent addition of SV ASD.
Exceptionally, we performed posterolateral thoracotomy in four patients (two bidirectional Glenn shunts and two scimitar syndromes) and upper mini-sternotomy in another three, all of them male (two aortic valve commissurotomies and one ascending aorta repair in a patient with Williams syndrome).
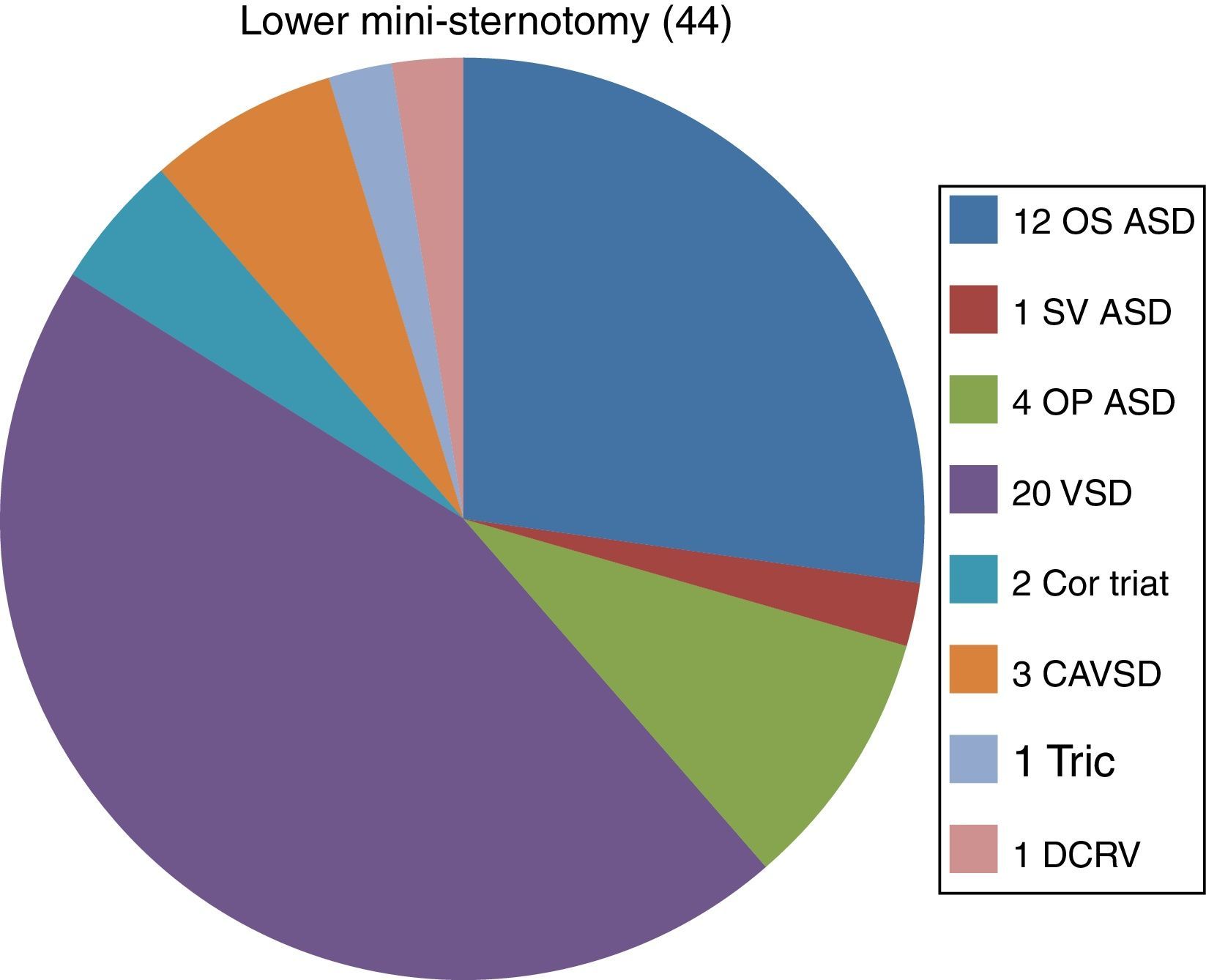
Lower mini-sternotomy is the approach last adopted by our team in 2013. An incision is made below the intermammary line, and the sternum is partially divided. We use a conventional sternal retractor and a cranial retractor system mounted on the horizontal rail of the anaesthesiologist.8–11 This incision is intended for closure of ventricular septal defects (VSDs), which are repaired in the early months of life and cannot be approached effectively through submammary or axillary incisions. As we had done before, the first patients operated on via this approach corresponded to simpler cases (OS ASD) as a learning curve prior to the inclusion of more complex indications (VSD, OP ASD, complete atrioventricular septal defect [CAVSD], etc.).
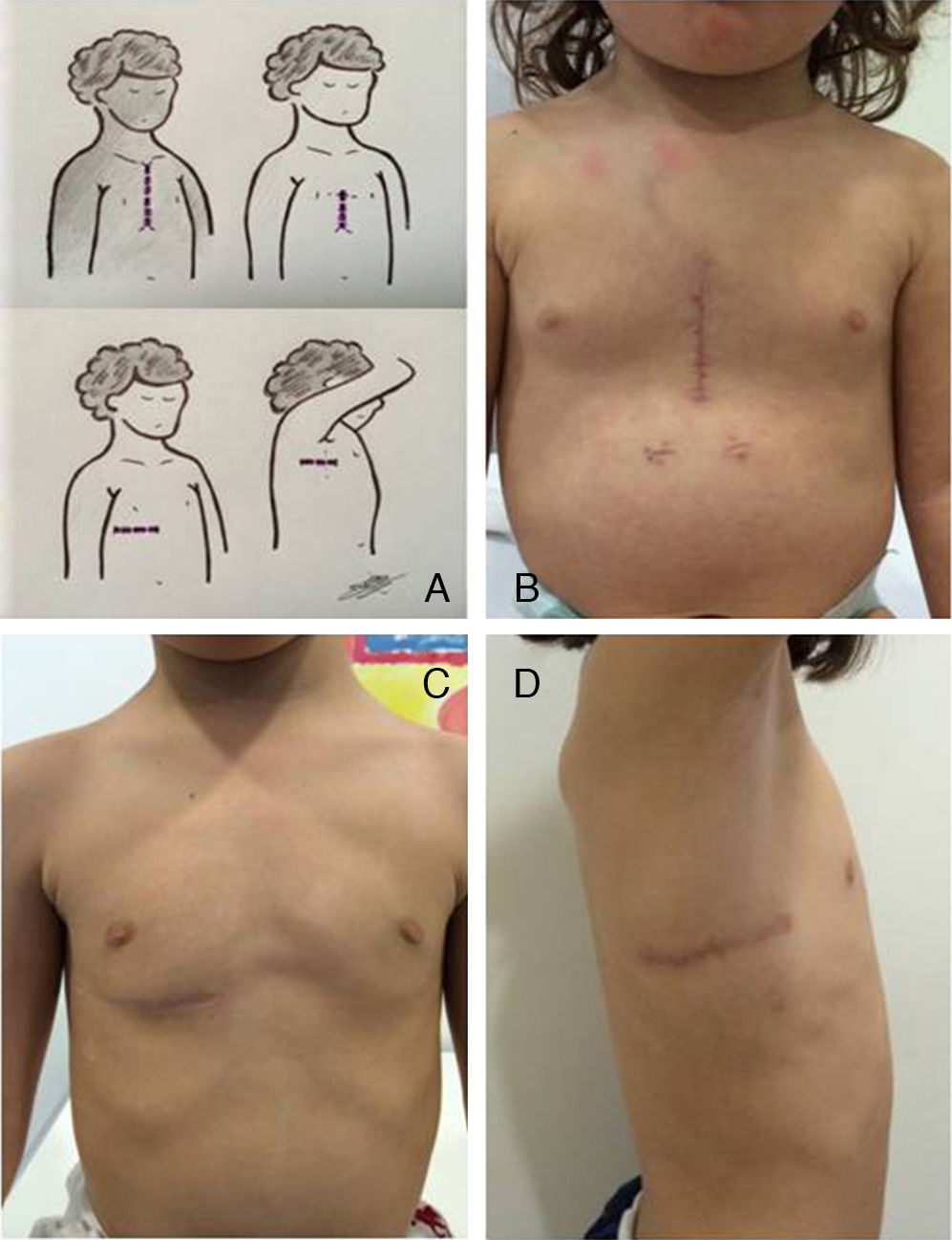
A principle that has remained consistent in our work has been to use the same technique and follow the same steps through an alternative incision (Fig. 1). Thus, cannulation manoeuvres (aorta and superior and inferior vena cava) to establish extracorporeal circulation (ECC), myocardial protection (aortic cross-clamping and infusion of cardioplegia through the aortic root), and surgical repair are all performed through a single alternative incision (submammary, axillary, mini-sternotomy). We do not use additional ports nor modify the myocardial protection strategy when we change the surgical incision.
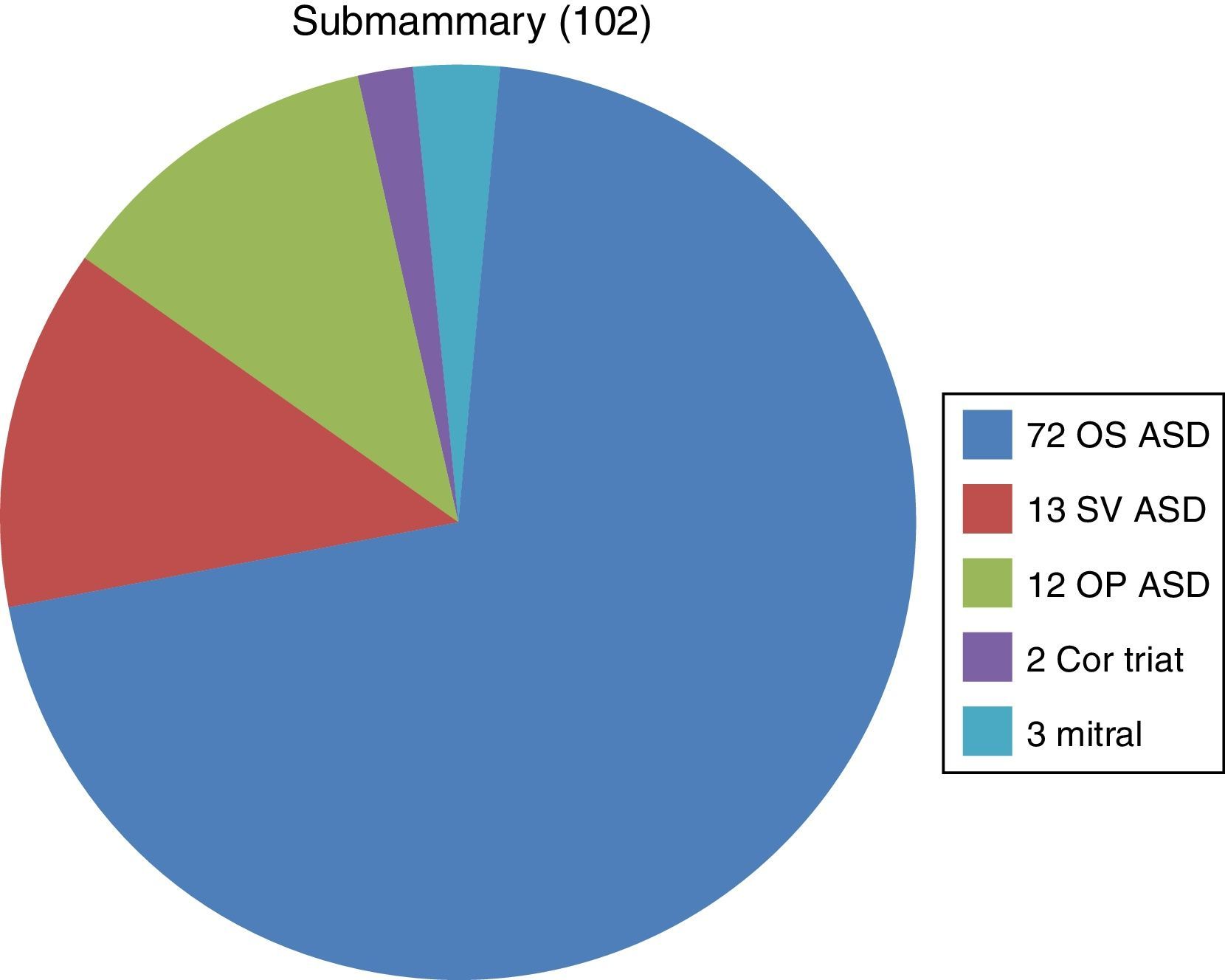
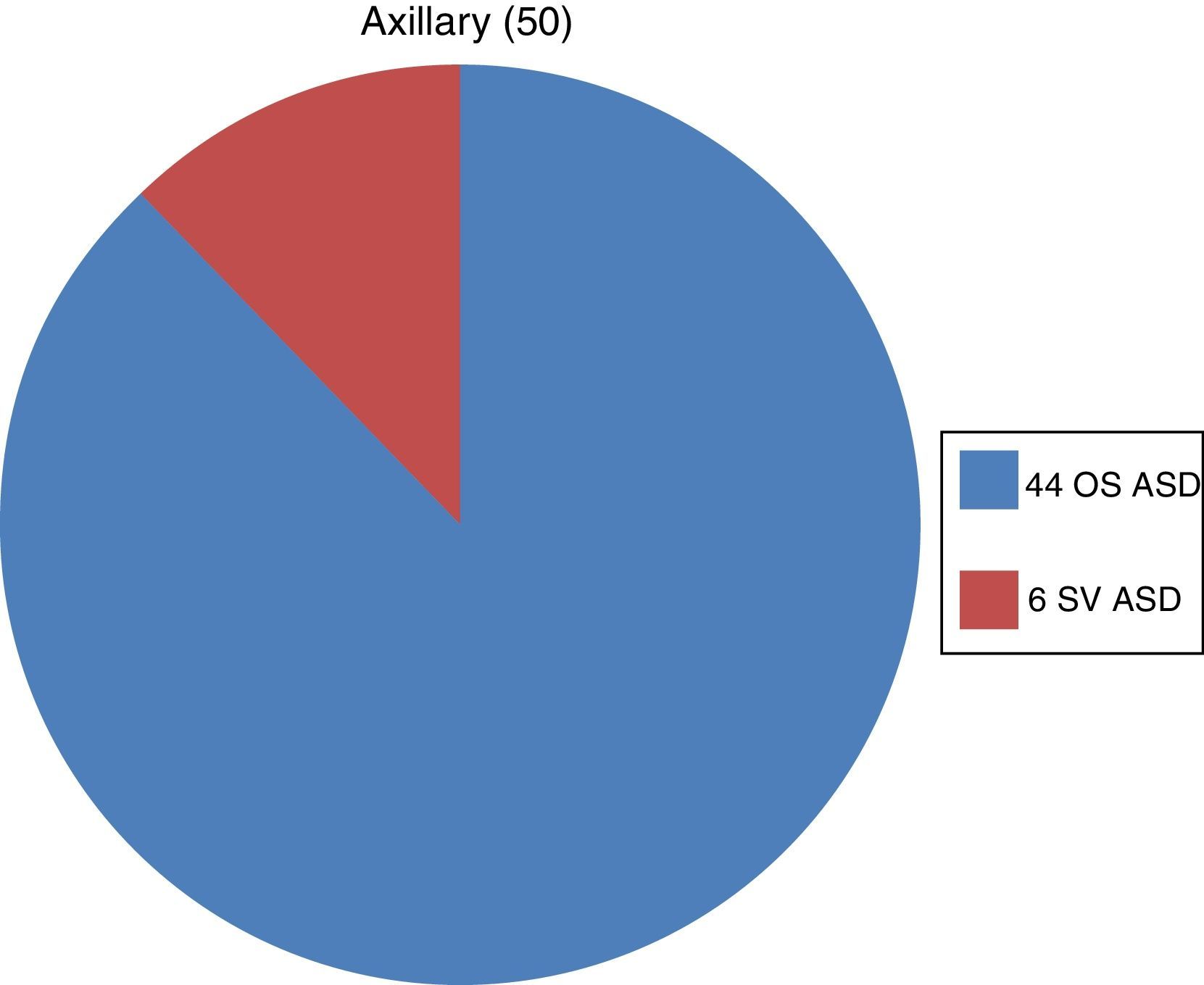
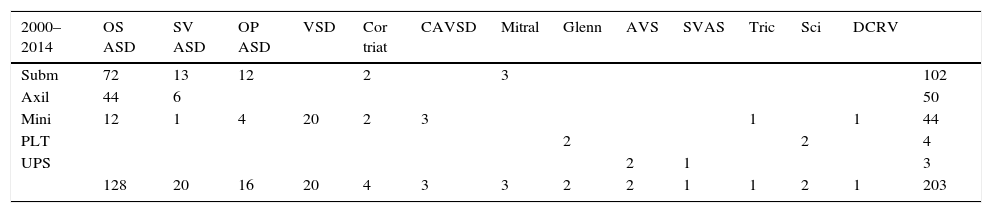
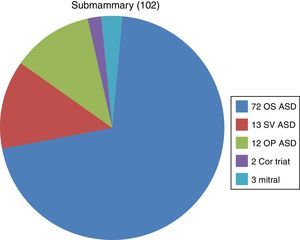
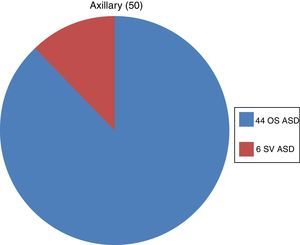
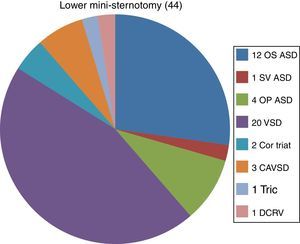
ResultsAs Table 1 shows, the most frequent surgical approach was the submammary incision (102), followed by axillary incision (50) and mini-sternotomy (44). We must keep in mind the gradual introduction of these approaches in years 2000, 2009 and 2013, respectively. Interventions involving posterolateral thoracotomy (4) and upper mini-sternotomy (3) were exceptional. The most frequently treated disease was ASD: OS ASD (128), followed by SV ASD (20) and OP ASD (16). Also frequent was VSD, with 20 cases in total, which started to be operated on via mini-sternotomy in 2013. The remaining cases corresponded to: 4 cor triatriatum, 3 complete atrioventricular septal defect, 3 mitral insufficiency, 2 bidirectional Glenn shunt, 2 aortic valve stenosis, 1 supravalvular aortic stenosis, 1 tricuspid valve repair, 2 scimitar syndrome, and 1 double-chambered right ventricle.
Association between surgical incisions and cardiopathies.
| 2000–2014 | OS ASD | SV ASD | OP ASD | VSD | Cor triat | CAVSD | Mitral | Glenn | AVS | SVAS | Tric | Sci | DCRV | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Subm | 72 | 13 | 12 | 2 | 3 | 102 | ||||||||
| Axil | 44 | 6 | 50 | |||||||||||
| Mini | 12 | 1 | 4 | 20 | 2 | 3 | 1 | 1 | 44 | |||||
| PLT | 2 | 2 | 4 | |||||||||||
| UPS | 2 | 1 | 3 | |||||||||||
| 128 | 20 | 16 | 20 | 4 | 3 | 3 | 2 | 2 | 1 | 1 | 2 | 1 | 203 |
AVS, aortic valve stenosis; ASD, atrial septal defect; Axil, axillary thoracotomy; CAVSD, complete atrioventricular septal defect; Cor triat, cor triatriatum; DCRV: double-chambered right ventricle (mid-ventricular stenosis); Mini, lower mini-sternotomy; Mitral, mitral valve insufficiency; OP, ostium primum (partial atrioventricular septal defect); OS, ostium secundum; PLT, posterolateral thoracotomy; Sci, scimitar syndrome; Subm, submammary; SV, sinus venosus (with partial anomalous pulmonary venous connection); SVAS, supravalvular aortic stenosis; Tric, tricuspid valve repair; UPS, upper partial sternotomy; VSD, ventricular septal defect.
The pie charts (Figs. 2–4) show the distribution of diseases for each surgical approach. The most frequent disease operated on via submammary and axillary approaches was OS ASD, while VSD was the most frequent operated on via mini-sternotomies. Only two forms of heart disease were operated on via the axillary approach (OS ASD, SV ASD) compared to five through the submammary approach (OS ASD, SV ASD, OP ASD, cor triatriatum and mitral insufficiency) and even eight different diagnoses through minimally invasive approaches, which are the most versatile.
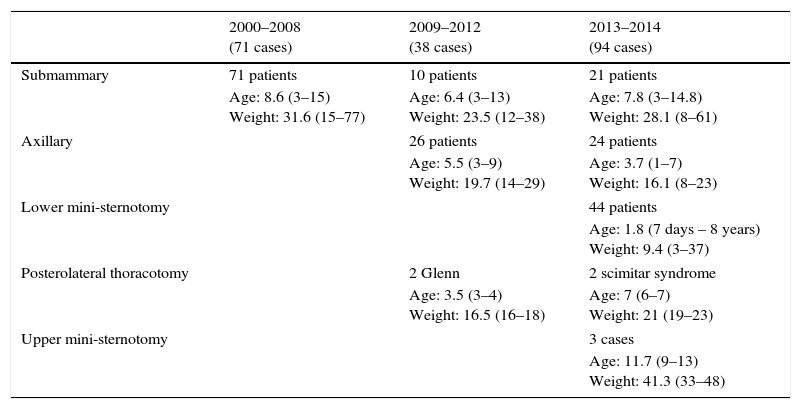
We also analysed our activity by time periods (Table 2), understood as the successive times alternative approaches were introduced: 71 surgical closures were performed through the submammary approach in the 2000–2008 period; 38 interventions (10 submammary, 26 axillary, 2 posterolateral thoracotomy) were performed in the 2009–2012 period; and 94 (21 submammary, 24 axillary, 44 lower mini-sternotomy, 3 upper mini-sternotomy, 2 lateral thoracotomy) in the 2013–2014 period.
Comparison of age (in years) and weight (in kg), expressed as mean and range, by surgical approach and time period.
| 2000–2008 (71 cases) | 2009–2012 (38 cases) | 2013–2014 (94 cases) | |
|---|---|---|---|
| Submammary | 71 patients | 10 patients | 21 patients |
| Age: 8.6 (3–15) Weight: 31.6 (15–77) | Age: 6.4 (3–13) Weight: 23.5 (12–38) | Age: 7.8 (3–14.8) Weight: 28.1 (8–61) | |
| Axillary | 26 patients | 24 patients | |
| Age: 5.5 (3–9) Weight: 19.7 (14–29) | Age: 3.7 (1–7) Weight: 16.1 (8–23) | ||
| Lower mini-sternotomy | 44 patients | ||
| Age: 1.8 (7 days – 8 years) Weight: 9.4 (3–37) | |||
| Posterolateral thoracotomy | 2 Glenn | 2 scimitar syndrome | |
| Age: 3.5 (3–4) Weight: 16.5 (16–18) | Age: 7 (6–7) Weight: 21 (19–23) | ||
| Upper mini-sternotomy | 3 cases | ||
| Age: 11.7 (9–13) Weight: 41.3 (33–48) | |||
Table 2 also shows the changes in the mean age (8.6, 6.4, 7.8years) and weight (31.6, 23.5, 28.1kg) of the patients that underwent surgery via a submammary approach in the three time periods. There were also changes in the axillary approach, with the mean age shifting from 5.5 to 3.7 years and the mean weight from 19.7 to 16.1kg. This can be interpreted as an increasingly early indication for surgical closure of OS ASD (and SV ASD, to a lesser degree). However, the most salient finding in this regard is the marked differences in the mean ages and weights for different approaches shown in the last column of Table 2. Patients operated on via the submammary approach were oldest (7.8 years; 28.1kg), those operated with the axillary approach were in the midrange (3.7 years; 16.1kg) and those operated by mini-sternotomy, including cases of VSD, were youngest (1.8 years, 9.4kg).
Our patients did not experience any neurologic events (which confirmed the safety of alternative approaches and the efficacy of myocardial protection and de-airing manoeuvres). The approach was converted to sternotomy in one patient (conversion rate<0.5%), after failing to close a VSD via a submammary incision. The patients and their families considered the cosmetic results to be excellent (Fig. 1).
DiscussionUnlike other surgical specialties, heart surgery has barely benefited from minimally invasive approaches. There are two main reasons for this: one is the difficulty of operating through small (or remote) incisions in an organ that is in motion and that requires extracorporeal circulation (ECC), and the other is the boom experienced by percutaneous procedures. The potential for treating a simple cardiopathy, such as ASD, without ECC or sternotomy is an incontestable justification. Therefore, as surgeons, we seek creative solutions that do not compromise patient safety, supported by fifty years’ experience in the particular case of surgical repair of ASD. In other words, we are knowledgeable of the long-term natural history of the disease (which is surgically repaired), and we also take into account cosmetic considerations without compromising the outcome.
As we mentioned in the introduction, the history of minimally invasive surgery started in the 1990s, mainly with the lower mini-sternotomy and lateral thoracotomy approaches. Most teams followed the same steps in the alternative approach, maintaining the manoeuvres for cannulation (for ECC) and protection by cardioplegia. Later on, some techniques started to be adjusted in order to minimise the size of surgical incisions. Thus, the practice of femoral (arterial or venous) cannulation and myocardial protection without cardioplegia (electrically induced fibrillation or beating heart) started to spread. The initial results showed longer operative times—total duration of the intervention, ECC, myocardial ischaemia (cross-clamping)—that reflected the learning curve.
Several factors and technical advances have fuelled the interest in minimally invasive surgery (beyond our “competition” with our colleagues specialised in haemodynamics):
- 1.
Intraoperative transesophageal echocardiography (TEE). It allows visualisation of myocardial function, intracardiac cannulae placement and manoeuvres for de-airing the left heart.
- 2.
Improvements in perfusion, including cannulae and assisted venous drainage systems (which allow the use of smaller-gauge catheters for the same body weight).
- 3.
Carbon dioxide insufflation of the operating field, which minimises the risk of air embolisation during de-airing manoeuvres.
These improvements increase patient safety, decreasing risks associated with myocardial protection and de-airing of the left heart (manoeuvres that are harder to perform via alternative incisions compared to complete median sternotomy).
Teams with extensive experience, especially in lateral thoracotomies, have experienced an evolution in their surgical strategy. In German teams, the submammary approach gave way to the axillary approach due to the suspected potential for future breast deformities.25 Subsequently, it has been demonstrated that the subpectoral approach24 (compared to the transpectoral approach) prevents these deformities. Similarly, they have replaced traditional myocardial protection (cross-clamping and cardioplegia) by electrically induced fibrillation20 (assisted by TEE). Vida et al. (Padua, Italy) have practised the full range of lateral approaches,5,26 along with technical advances. They started with extensive submammary and posterolateral incisions, applying a sex-differentiated protocol,28 and later on incorporated femoral cannulation (and at times cervical cannulation) monitored by near-infrared spectroscopy29 (NIRS) to gradually minimise the original incision.
This article summarises our cumulative experience of fifteen years. We have upheld two principles: patient safety, and performance of the same steps through a single alternative incision. We have advanced with caution, starting with simple cases and expanding indications after going through the learning curves and analysing the different phases of the perioperative period for each procedure.30 In two initial publications,16,22 we compared ECC and cross-clamping times compared to conventional sternotomy, demonstrating that they were not longer and thus confirming the safety of the procedure. A consistent principle of our evolving practice is that we do not modify our myocardial protection strategy (aortic cross-clamping with cardioplegia). We do not use additional ports nor change our myocardial protection technique when we change the surgical approach: “same tools, same steps, same risks, different approach.” It is our opinion that alternative techniques (such as induced fibrillation or beating heart) are not routinely used in simple cases operated via median sternotomy and are not justified on the sole basis of using a different thoracic access. Similarly, the help of one or more additional ports (thoracic, femoral, jugular, etc.) would turn this surgical modality into “pluri-minimally invasive,” and has not been used in our practice.
Our conversion rate has been very low. Only 1 of 203 cases (<0.5%) required conversion to a median sternotomy when it became clear that we could not guarantee the outcome of VSD repair via the submammary approach. Other aspects, such as the absence of neurologic events (which corroborated the safety of the alternative approaches and the efficacy of myocardial protection and de-airing manoeuvres) or the satisfaction of patients and parents, have been very positive.
The progressive incorporation of the axillary approach and mini-sternotomy to our everyday practice has allowed us to expand the services we offer. Nearly 20% of the surgeries with ECC that we perform are minimally invasive. In this regard, there has been a considerable increase in our professional activity since we started offering VSD closure through mini-sternotomy (with its corresponding learning curve through performance of procedures in simpler cases). Given its expanded indications for younger ages and a greater number of diseases, we expect an increase in the use of mini-sternotomy compared to the axillary and submammary approaches. The access via posterolateral thoracotomy used in four patients (two Glenn, two scimitar syndrome) can be very useful as a transitional step to the axillary approach. We consider the three cases of aortic valve or supravalvular aortic disease operated on via upper mini-sternotomy to be exceptional, as cosmetic outcomes with this approach are not noticeably improved.
The cases we have treated to date include heart diseases that can be approached through the right atrium (and occasionally the left, such as mitral valve disease and cor triatriatum) and cases of increasing complexity, ranging from OS ASD to CAVSD. Given the increasingly younger ages for which surgical repair of some cardiopathies is indicated, the versatility of different surgical approaches allows us to select the most appropriate for each case. The different incisions presented here are not mutually exclusive, and we can offer different options based on the type of heart disease or the weight of the patient. Thus, as can be seen in Table 2, we repaired a VSD in a child weighing less than 10kg via a mini-sternotomy, perform surgical closure of ostium secundum or sinus venosus ASDs in children weighing more than 16kg via axillary incision, and use the submammary approach in older female patients with developed breasts (Fig. 5). The differential sex-based approach28 is no longer upheld: both male and female paediatric patients can benefit from minimally invasive approaches today.
The quality standards applied to minimally invasive surgery must be the same as those applied to conventional surgery. Improved cosmetic outcomes are an added value to the already positive outcomes achieved by paediatric heart surgery in recent years. It is obvious that approaches alternative to sternotomy cannot be chosen while jeopardising the surgery. We must be critical of our own work: a poor outcome cannot be justified by cosmetic concerns. We must be aware of our own limitations, as was the case of our failed attempt of closing a VSD through a submammary incision.
From a training perspective, the learning curve is gradual and safe if cases are rigorously selected. We propose that cases traditionally approached via lateral thoracotomy be first approached via a submammary incision, then a posterolateral incision, and finally an axillary access. It is advisable that all members of the surgical team become familiar with minimally invasive techniques (Fig. 5) and master approaches alternative to median sternotomy.
Alternative, less invasive approaches can be carried out with robotic technology.30–33 The barriers to its implementation are the low availability of the equipment and its rare use in children that weigh less than 30kg.23 A possible transitional step would be video-assisted surgery,34,35 using thoracoscopy equipment (rigid endoscope, specialised retractors and forceps) to assist minimally invasive approaches.
ConclusionSurgical repair of specific congenital heart diseases by minimally invasive approaches in the paediatric age group has shown excellent results. It does not increase surgical risk, and is associated with decrease postoperative morbidity and better functional and cosmetic outcomes compared to conventional surgery. After a cumulative experience of 15 years and more than 200 surgeries, we can establish guidelines for training and learning curves for different surgical approaches. Given the progressive decrease in age at the time of surgical repair of certain cardiopathies, and taking advantage of the versatility of different minimally invasive incisions, we choose the most appropriate approach based on the age and disease of the patient.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Gil-Jaurena JM, González-López MT, Pérez-Caballero R, Pita A, Castillo R, Miró L. 15 años de cirugía cardiaca infantil miniinvasiva; evolución y tendencias. An Pediatr (Barc). 2016;84:304–310.