Vasa praevia is a rare condition in which the foetal blood vessels cross the foetal membranes of the lower segment of the uterus below the presenting part. It has a high foetal mortality due to foetal exsanguination resulting from foetal vessels tearing when the membranes rupture. Prenatal diagnosis can reduce or even prevent foetal mortality, but it requires a high level of suspicion. For this reason, pregnant women with risk factors of vasa praevia should be examined using transvaginal ultrasound in combination with colour Doppler, and if the diagnosis is made, elective delivery by caesarean and aggressive resuscitation of the new born is indicated.
La presencia de vasa previa es una afección poco frecuente en la que los vasos fetales atraviesan las membranas amnióticas por encima del cuello del útero y por debajo de la presentación foetal. Asocia una mortalidad elevada debida a la exanguinación foetal producida por el desgarro de los vasos fetales al romperse las membranas amnióticas. El diagnóstico prenatal puede disminuir significativamente la tasa de mortalidad, pero requiere un alto índice de sospecha. Por este motivo, aquellas mujeres embarazadas que presenten factores de riesgo de vasa previa deben ser exploradas con ecografía transvaginal y Doppler colour. Si se confirma el diagnóstico, está indicada la realización de una cesárea electiva y una enérgica reanimación del recién nacido. Presentamos el caso de un recién nacido que nace en parada cardiorrespiratoria que no revierte, pese a una enérgica reanimación, debido a la rotura de un vasa previa no diagnosticado.
Vasa praevia is said to occur when the foetal blood vessels traverse the membranes over the cervix, below the presenting part.1 There are two variants: type 1, which results from velamentous insertion of the umbilical cord, and type 2, which occurs when foetal vessels run between the lobes of a bilobed or succenturiate-lobed placenta.2 Its incidence is approximately 1 in every 2500 pregnancies.3 Spontaneous or artificial rupture of the membranes leads to a tearing of the foetal blood vessels, frequently giving rise to rapid foetal exsanguination3 and high perinatal mortality.3–5
Case historyA healthy expectant mother, aged 28, attended the accident and emergency department in week 38 of pregnancy with premature rupture of membranes. The pregnancy had been controlled, with negative blood tests, except for rubella, to which she was immune. In the ultrasound scan performed in week 20 an anomaly compatible with club foot was diagnosed in the right foot. The next ultrasound scan, performed in week 36, did not find any other different anomalies.
Examination of the patient on arrival at the hospital detected the presence of vaginal blood clots. The foetal heart rate in the cardiotocographic recording and the ultrasound examination was 90 beats per minute. A Caesarean section was immediately performed for suspected placental abruption. The infant, a boy, was born floppy and markedly pale, with no respiratory effort and no heartbeat. Orotracheal intubation and intermittent positive pressure ventilation were performed. Since no response was detected, cardiac massage was initiated and a first dose of adrenaline was immediately administered. It was repeated a further five times. After 20min, in view of the lack of response, resuscitation manoeuvres were discontinued. The pH of the umbilical artery was 6.88.
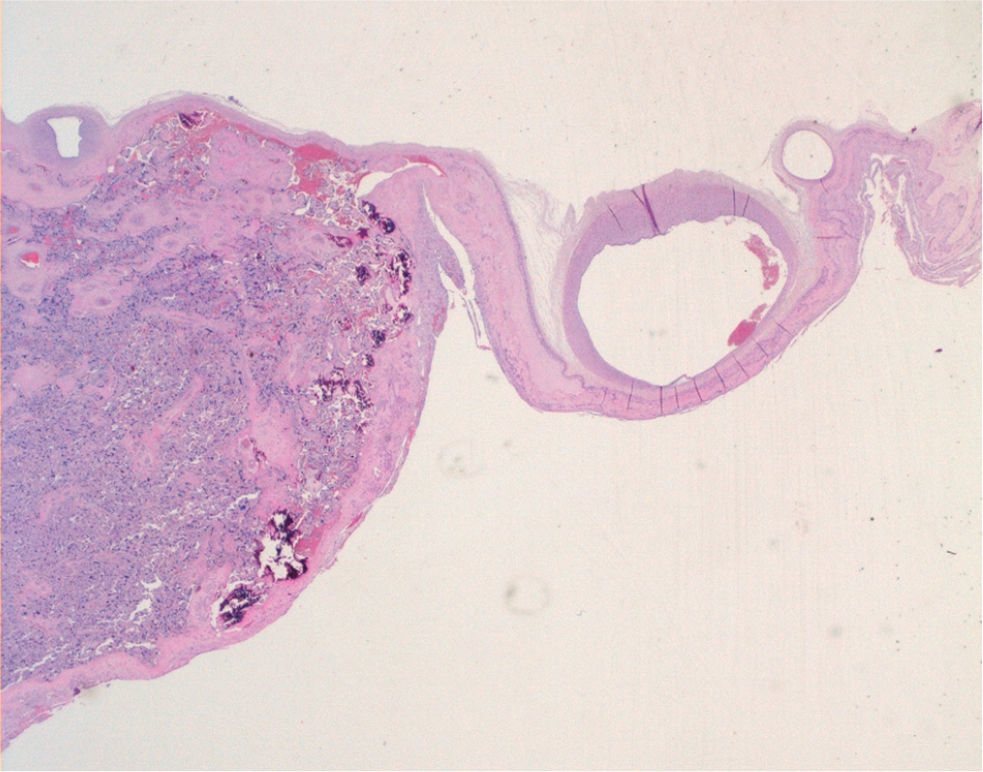
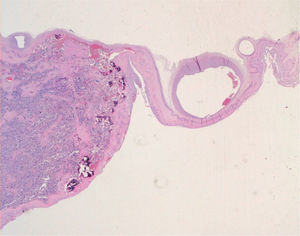
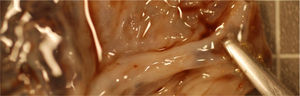
An anatomical and pathological examination of the foetus, placenta and adnexa was carried out. The conclusion was that it was a male foetus, weighing 2270g, with a right club foot. In the placenta a recent haemorrhage was observed in the chorioamniotic membranes, with no signs of inflammation. The histological section of the vascular structures showed that it was a case of velamentous insertion of the umbilical cord (Figs. 1 and 2).
DiscussionFew obstetric tragedies are as unexpected as vasa praevia rupture. Its incidence is 1 in every 2500 pregnancies,3 though this is probably an underestimate, as it is a problem that tends to go undiagnosed.6
In the period before the widespread use of ultrasound, diagnosis could be made during vaginal examination with a speculum or by direct palpation of the vessels during delivery. Foetal mortality ranged between 58% and 73%.7 It currently stands at around 33%; there are very few obstetric conditions with so high a rate of foetal mortality that do not entail any risk for the mother.6 When the membranes are ruptured, tearing of the foetal vessels occurs and a small amount of vaginal bleeding appears, the significance of which is commonly underestimated.8
Various risk factors have been identified for the presence of vasa praevia, including in vitro fertilisation,9 bilobed or succenturiate-lobed placenta10 and multiple pregnancies.11 On the other hand, velamentous insertion of the cord is associated with an increase in the incidence of certain foetal anomalies, such as renal malformations, spina bifida, ventricular septal defect, single umbilical artery and an increase in obstetric complications, including miscarriage, prematurity and low birth weight.12 We have not found cases in the literature of vasa praevia associated with club foot, as occurred in our patient.
Dougall and Baird13 describe five modes of presentation: vessel rupture at amniotomy, vessel rupture before rupture of membranes, vessel rupture after rupture of membranes, vessel compression, and vessels palpable on vaginal examination.
The most frequent presentation is the first. Given that the blood volume of a term neonate is about 250mL, a haemorrhage of around 50–60mL (20–25% of the total) can lead to shock and death.6 Vaginal bleeding appearing at amniotomy should raise suspicions of the presence of vasa praevia.
Compression of foetal blood vessels by presentation is manifested as decelerations and bradycardia in the cardiotocographic recording13–15 and can lead to asphyxia and foetal death in 50–60% of cases.14,15 The aetiology of irregularities in foetal heart rate varies, but the presence of vasa praevia must be taken into account in differential diagnosis.15
The first diagnosis of vasa praevia using ultrasonography was made in 1987.16 In later years, improvements in the resolution of ultrasound images and the addition of Doppler colour made it easier to identify the point of insertion of the umbilical cord. Sepúlveda et al.17 report that they were able to identify the placental cord insertion site in 99% of cases and that the exploration was not particularly time-consuming. Other authors report a sensitivity of 62.5% in antenatal detection of velamentous insertion of the cord, with a positive predictive value of 100% and a negative predictive value of 99.6%.18
According to Lee et al., vasa praevia can be identified from the second trimester of pregnancy.19 Nevertheless, given that some cases of vasa praevia resolve themselves spontaneously at the end of the pregnancy, they consider it reasonable to confirm the diagnosis in the third trimester, when its detection has the greatest impact on treatment.
The treatment consists of performing a Caesarean section in week 35 of pregnancy or even earlier, if the lung maturity of the foetus has been documented. Immediate neonatal resuscitation must be aggressive and a rapid restitution of blood volume must be carried out. Some authors propose hospitalising the expectant mother in the 32nd week of pregnancy, administering corticosteroids to accelerate the lung maturation of the foetus and performing an urgent Caesarean section in the event of premature rupture of membranes before the 35th week. When an antenatal diagnosis is made, there are no associated malformations and an elective Caesarean is performed, the survival rate of newborns is close to 100%.20
Velamentous insertion of the umbilical cord is an obstetric complication that can have fatal consequences for the foetus. Its antenatal diagnosis is straightforward and enables effective preventive and therapeutic measures to be taken. We believe that this anomaly should be investigated by ultrasound in all pregnancies, or at least in those where risk factors for the condition exist.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pérez Rodríguez MJ, de Frutos Moneo E, Nieto Llanos S, Clemente Pollán J. Rotura de vasa previa en una inserción velamentosa de cordón umbilical. Importancia del diagnóstico prenatal. An Pediatr (Barc). 2014;81:393–395.