The Niño Jesús Hospital procedural sedation scale (Madrid) (NJHPSS) has not been validated.
Patients and methodsA prospective analytical study was conducted in 2 hospitals on patients ≥6 months undergoing invasive procedures using sedation-analgesia with propofol or midazolam and fentanyl. All were monitored using the bispectral index (BIS). Videos were made of each procedure, which were then edited and randomised. A total of 150 videos were rated by four observers using the NJHPSS, the University of Michigan sedation scale (UMSS), and the Ramsay Scale (RS). These observers were blinded to the BIS, and at the time of drug administration. To assess test-retest reliability, 50 of the initial 150 randomly selected videos were re-assessed.
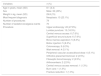
ResultsThe study included a total of 65 patients. Construct validity was demonstrated by changes in scores after administering sedatives (p<.0001). The NJHPSS had a very low correlation with the BIS (r=−0.166), and a moderate correlation with the UMSS (r=0.497) and the RS (r=0.405).The within-observer agreement was high (ρ=0.793). The NJHPSS gave a good interobserver reliability when compared with the UMSS (ICC=0.88) and the RS (ICC=0.86), and there was none with the BIS. Internal consistency was moderate (α=0.68). As regards the applicability, this scale has been used in two hospitals in several areas by four professionals of different categories.
ConclusionsThe NJHPSS is valid, reliable and applicable for sedation monitoring in invasive procedures under deep sedation-analgesia in paediatric patients. The NJHPSS has worse properties than the UMSS and the SR.
La escala de sedación para procedimientos del Hospital Niño Jesús (ESPHNJ) no ha sido validada.
Pacientes y métodosEstudio analítico prospectivo bihospitalario. Se reclutaron prospectivamente pacientes ≥ 6 meses sometidos a procedimientos invasivos bajo sedoanalgesia con propofol o midazolam y fentanilo. Todos fueron monitorizados con el índice biespectral (IB). Se realizaron videos de cada procedimiento, que fueron editados y aleatorizados. Ciento cincuenta videos fueron puntuados por cuatro observadores con la ESPHNJ, la escala de sedación de la Universidad de Michigan (ESUM) y la Escala de Ramsay (ER). Dichos observadores estaban cegados al IB y al momento de administración de fármacos. Para evaluar la fiabilidad test-retest, 50 videos de los 150 iniciales seleccionados aleatorizadamente fueron reevaluados.
ResultadosFueron incluidos 65 pacientes. La validez de constructo fue demostrada por los cambios en las puntuaciones tras administrar sedantes (p<0,0001). La ESPHNJ tuvo muy baja correlación con el IB (r=−0,166), y correlación moderada con la ESUM (r=0,497) y la ER (r=0,405). La concordancia intraobservadores fue alta (ρ=0,793). La ESPHNJ presentó una fiabilidad interobservador buena al comparar con la ESUM (CCI=0,88) y con la ER (CCI=0,86), y no hubo con el IB. La consistencia interna fue moderada (α=0,68). En relación a la aplicabilidad, nuestro trabajo se ha empleado en dos hospitales en varios ámbitos por cuatro profesionales de diferentes categorías.
ConclusionesLa ESPHNJ es válida, fiable y aplicable para la monitorización de la sedación en procedimientos invasivos bajo sedoanalgesia profunda en pediatría. La ESPHNJ presenta peores propiedades que la ESUM y que la ER.
Some sedation scales associate different levels of consciousness with behavioural responses to auditory or somatosensory stimuli.
For a sedation scale to be considered ideal, it must have the following characteristics1: easy to use, applicable to every possible clinical situation and age group, reliable, capable to discriminate between different levels of sedation (especially between moderate and deep sedation) and feasible (that is, must be based on few, simple and easy to measure parameters).
The most significant limitations of these scales are their subjectivity, that they are reliable only at minimal and moderate depths of sedation and the use stimuli to obtain a score.2 Stimuli can be disruptive during procedures and there may be variance between observers.
The Niño Jesús Hospital Procedural Sedation Scale (known as the ESPHNJ) was published by A. Valdivielso Serna in 19983 and uses 4 categories to classify the level of consciousness of patients during procedures: level 1 corresponds to an awake, alert and oriented, and level 4 to a patient that does not respond to physical stimuli, although possibly capable of perceiving pain if the stimulus is strong enough (Table 1).
Levels of sedation and corresponding patient characteristics in the different scales used to assess procedural sedation in paediatric patients.
| Level | Characteristics |
|---|---|
| Hospital Niño Jesús Procedural Sedation Scale | |
| 1 | Awake, alert, oriented |
| 2 | Lethargic. Awake and oriented when spoken to |
| 3 | Asleep. Wakes up in confusion only with physical stimuli |
| 4 | Unresponsive to painless physical stimuli |
| Level 1–2: moderate sedation (without agitation) | |
| Level 3–4: deep sedation | |
| University of Michigan Sedation Scale | |
| 0 | Awake, alert |
| 1 | Minimally sedated: sleepy/tired, appropriate response to verbal conversation and/or sounds |
| 2 | Moderately sedated: somnolent/sleeping, easily aroused with light tactile stimulation or a simple verbal command |
| 3 | Deeply sedated: deep sleep, aroused only with significant physical stimulation. |
| 4 | Unarousable |
| Ramsay Scale | |
| 1 | Awake, anxious and agitated or both |
| 2 | Awake, cooperative, oriented and tranquil |
| 3 | Sleepy, responds only to commands |
| 4 | Asleep, brisk response to tactile stimulus or loud noise |
| 5 | Asleep, sluggish response to stimuli |
| 6 | Deeply asleep. Unresponsive to external stimuli, including painful stimuli |
This scale offers several advantages: it is simple, takes only a few seconds and is easy to reproduce, all of which makes it widely applicable. It has been widely used in Spain in children of varying ages to assess the depth of sedation in procedures performed outside the operation theatre and in the paediatric intensive care unit (PICU) setting.4–11 A study published in 2015 reviewed a series of 13737 cases of paediatric sedation and analgesia during painful procedures performed at the Hospital Universitario Niño Jesús (HUNJ).4 The main limitation of this scale is that it has not been validated.
The bispectral index (BIS) estimates the level of consciousness of a patient through a mathematical analysis of electroencephalographic frequency and amplitude data. It is validated for assessment of for children aged more than 1 year undergoing procedural sedation,2,12–16 and some authors have found it useful in children aged more than 6 months.12,17,18
The University of Michigan Sedation Scale (UMSS)19 was designed specifically to assess procedural sedation in paediatric patients and has been validated (Table 1).
The Ramsay Scale (RS)20 is the scale used most widely at the international level for assessment of procedural sedation. It has not been validated in the paediatric age group (Table 1).
The aim of our study was to assess the validity, reliability and feasibility of the ESPHNJ to assess sedation used for invasive procedures in paediatric patients through comparison with the BIS (a validated objective instrument), the UMSS (a validated subjective instrument) and the RS.
Patients and methodsWe conducted a prospective analytical study in 2 hospitals to validate the ESPHNJ.
SampleEnrollment by consecutive sampling of all children that met the inclusion criteria. Patients in the sample underwent invasive diagnostic or therapeutic procedures and received sedation or analgesia from paediatricians at the HUNJ (in the analgesia and sedation unit) and the Hospital General La Mancha Centro (HGMC) (in the special tests unit, the paediatric intensive care unit [PICU], the emergency department or the paediatric ward) between April 2016 and June 2017. The exclusion criteria were: age less than 6 months, use of general anaesthesia, administration of ketamine (as it decreases the level of consciousness without an associated decrease in the BIS readings), use of mechanical ventilation, administration by a route other than the intravenous route, severe compromise, moderate or severe cognitive impairment, or performance of a magnetic resonance scan (as BIS monitoring is not possible during this procedure).
Scales/measurement instrumentsWe used the ESPHNJ, the UMSS19 and the RS.20
We also use BIS monitoring. Values of 80–100 indicate absence of sedation or mild sedation, values of 60–80 moderate sedation, values of 40–60 deep sedation and values of less than 40 a deep hypnotic state.21
Study protocol and data collectionAll sedation and analgesia procedures followed the established protocol in each of the hospitals, which had similar protocols. Propofol and/or midazolam were used for sedation and fentanyl for analgesia.
Propofol and fentanyl protocol: propofol, 2mg/kg (up to a maximum of 100mg) over 3min, followed by 1mg/kg (maximum 50mg) over 3min, and 10mg/kg/h for maintenance. Fentanyl, 2μg/kg (maximum 100μg) over 3min, followed by 1μg/kg (maximum 50μg) over 3min. From this point, titration by 0.5μg/kg increments (maximum 25μg) until desired analgesia is achieved.
Midazolam and fentanyl protocol: midazolam 0.2mg/kg over 3min (maximum 10mg), followed by 0.1mg/kg (maximum 5mg) over 3min. From this point, titration by 0.05mg/kg increments (maximum 2.5mg) to maintain deep sedation. Fentanyl same as previous protocol.
The physicians that managed the patients were blinded to the BIS values.
All patients were monitored with BIS (BIS VISTA®; Aspect Medical Systems, Norwood, United States) through 10min after the procedure ended. The principal investigator recorded the BIS values displayed in the BIS view monitor.
We recorded video for all procedures. We edited out segments with insufficient BIS quality (signal quality index [SQI] <50 and/or electromyography [EMG] value >50), after which there were 1188min of video recording left. We split video recordings in 30-s segments (so that observers would be blind to the moment when sedatives and analgesics were delivered). Subsequently, we coded the segments and selected 150 of them at random.
Four observers evaluated the level of sedation using the three scales. These observers did not receive specific training on the scales, instead applying them based on their own experience. The observers were 1 paediatrician, 1 PICU nurse, 1 anaesthesiologist and 1 surgical nurse with experience in paediatric sedation and analgesia. All were blinded to the timing of drug delivery and to the BIS values. Each observer scored all 150 videos using the UMSS. After this, the paediatrician and the PICU nurse (group 1A) scored a random selection of 75 of the 150 videos (video set 1) with the RSS, independently and blinded to each other. The anaesthesiologist and the surgical nurse (group 1B) scored the remaining 75 videos (video set 2) with the RSS, independently and blinded. Later on, group 1B scored the videos they had not seen (video set 1) with the ESPHNJ, and group 1A did the same with video group 2 (Fig. 1).
To assess the test-retest reliability and intraobserver agreement, 50 videos from sets 1 and 2 selected at random were scored again by the same observers with the ESPHNJ and the RS. Lastly, we assessed interobserver variation by comparing the different members of group 1.
To correlate the value recorded per minute of BIS monitoring with a 30-s fragment extracted from each minute of recording, we used the BIS value recorded during that minute, as has been done in most previous studies.12,13,22–27
Since the scoring scheme differed between the UMSS (5 categories), the ESPHNJ (4 categories) and the RS (6 categories), we performed z transformations of the scores obtained with these instruments.
Data analysisWe calculated the required sample size for an expected correlation coefficient of 0.6, a power of 90% and a 95% level of confidence, which was of 25 patients. The final sample included 65 patients enrolled by consecutive sampling.
We have summarised quantitative data as mean and standard deviation (SD) or median and interquartile range (IQR) depending on the distribution of the variable. We summarised qualitative data as absolute and relative frequencies.
In the assessment of the construct validity of the ESPHNJ, we used the Wilcoxon signed-rank test to describe changes in scores over time following sedative administration.
To assess criterion validity, we analysed the correlation between ESPHNJ scores and BIS values, UMSS scores and RS scores by calculating the Spearman or the Pearson correlation coefficient as applicable based on the distribution of the variable. We used the guidelines proposed by Cohen to assess the obtained correlation values,28 considering coefficients of 0.6 or greater indicative of an adequate correlation.
We assessed interobserver agreement by means of the intraclass correlation coefficient (ICC), consider values of the ICC of 0.75 or greater indicative of good reliability. We also assessed this aspect with Kendall's τ. In addition, we assessed the internal consistency of the scale using Cronbach's α, defining adequate consistency as a value greater than 0.7. We assessed test-retest reliability by means of the Spearman correlation coefficient.
To assess the precision of the BIS score in predicting the depth of sedation, we generated receiver operating characteristic (ROC) curves for the ESPHNJ score, dichotomising the BIS score for each of the levels of sedation.
All the statistical analyses were performed with the software SPSS® version 18. We defined statistical significance as a p-value of less than 0.05.
Ethical considerationsThe study was approved by the Research and Ethics Committee of the HGMC and adhered to the principles of the Declaration of Helsinki.
We obtained the informed consent of the parents or legal guardians of each participant.
ResultsThe sample included 65 patients with a mean age of 8.1 years (standard deviation [SD]: 4.4), 49% were male, all had an ASA (American Society of Anesthesiologists) physical status classification I or II.29 Thirty-seven (56%) underwent sedation/analgesia at the HUNJ (sedation and analgesia unit) and 28 (44%) at the HGMC (15 [23%] in the special tests unit, 7 [11%] in the PICU, 6 [9%] in the emergency department and 1 [1%] in the paediatrics ward). Table 2 summarises the characteristic of the patients included in the study.
Characteristics of the patients and procedures included in the analysis.
| Variables | n (%) |
|---|---|
| Age in years, mean (SD) | 8.1 (4.4) |
| Sex | Male: 32 (49%) |
| Weight in kg, mean (SD) | 29.8 (15) |
| Most frequent diagnosis | Neoplasia: 15 (23.1%) |
| Number of procedures | 79 |
| Number of sedation/analgesia events | 70 |
| Procedure | Upper endoscopy: 22 (27.8%) |
| Lumbar puncture: 13 (16.5%) | |
| Central venous access: 6 (7.6%) | |
| Superficial wound suture: 6 (7.6%) | |
| Bone marrow aspiration: 5 (6.3%) | |
| Botox injection: 5 (6.3%) | |
| Colonoscopy: 5 (6.3%) | |
| Wart removal: 4 (5.1%) | |
| Peripheral vascular access/blood draw: 4 (5.1%) | |
| Orthotics placement/removal: 2 (2.5%) | |
| Fibreoptic bronchoscopy: 2 (2.5%) | |
| Arthrocentesis: 2 (2.5%) | |
| Central venous access removal: 1 (1.3%) | |
| Burn care: 1 (1.3%) | |
| Fracture reduction: 1 (1.3%) |
The 65 patients underwent a total of 79 procedures associated with 70 sedation/analgesia procedures. The most frequent sedative was propofol, used in 87% of the patients (mean dose, 4.2mg/kg; SD, 1.6), while midazolam was used in 13% (mean dose, 0.31mg/kg; SD, 0.18). Fentanyl was used in 85% of the patients (mean dose, 3.1μg/kg; SD, 0.95).
Table 3 presents the median BIS values and median scores obtained with the UMSS, the ESPHNJ and the RS for the 150min of recording included in the analysis.
Results obtained with the bispectral index, the University of Michigan Sedation Scale, the Niño Jesús Hospital Procedural Sedation Scale and the Ramsay Scale.
| Variable | Median (interquartile range) |
|---|---|
| Bispectral index | 63 (55–70) |
| University of Michigan Sedation Scale | 4 (3.25–4) |
| Paediatrician | 4 (4–4) |
| PICU nurse | 4 (3.5–4) |
| Anaesthetist | 4 (3–4) |
| Surgical nurse | 4 (3–4) |
| Niño Jesús Hospital Procedural Sedation Scale | 4 (4–4) |
| Paediatrician | 4 (4–4) |
| PICU nurse | 4 (4–4) |
| Anaesthetist | 4 (4–4) |
| Surgical nurse | 4 (4–4) |
| Ramsay Scale | 6 (5.5–6) |
| Paediatrician | 6 (6–6) |
| PICU nurse | 6 (6–6) |
| Anaesthetist | 6 (5–6) |
| Surgical nurse | 6 (5–6) |
PICU, paediatric intensive care unit.
When it came to the construct validity of the ESPHNJ, we found a significant increase in the sedation scores relative to baseline 5, 10 and 15min after administration of sedation/analgesia (p<.001). The level of sedation increased from a median of 1 (range, 1–1) at baseline to 3 (2.8–4) at 5min and 4 (4–4) at 10 and 15min. For the criterion validity, we found a negative correlation between the ESPHNJ and the BIS (r=−0.166), compared to a positive and stronger correlation between the BIS and the UMSS (r=0.497) and the BIS and the RS (r=0.405).
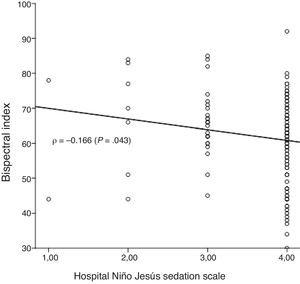
Fig. 2 presents the scatterplot for the ESPHNJ and BIS scores of the 150 paired measurements in the 65 patients. The ROC curves showed a low power of the BIS for prediction of sedation levels 2, 3 and 4 in the ESPHNJ. The sensitivity and specificity were 56% and 65%, respectively, for the prediction of level 4, and 40% and 94%, for the prediction of level 3 (Fig. 3).
Lastly, in the analysis of the interobserver agreement, we found a correlation coefficient of 0.428 for the agreement between the paediatrician and PICU nurse, and a coefficient of 0.388 for the agreement between the anaesthesiologist and the surgical nurse.
ReliabilityIn the analysis of the internal consistency of the ESPHNJ, we found a Cronbach α of 0.68 (95% CI, 0.488–0.796) and a high intraobserver reliability (ρ=0.793) (Table 4). We did not find interobserver agreement between the ESPHNJ and BIS. Table 5 presents the interobserver agreement between the ESPHNJ and the UMSS and the ESPHNJ and the RS in terms of the ICC and Kendall τ.
Agreement of the Niño Jesús Hospital Procedural Sedation Scale with the bispectral index, the University of Michigan Sedation Scale and the Ramsay Scale.
| ICC | 95% CI | p | Kendall τ | p | |
|---|---|---|---|---|---|
| ESPHNJ-BIS | 0.205 | (−0.098 to 0.424) | .082 | 0.106 | .092 |
| ESPHNJ-UMSS | 0.880 | (0.834–0.913) | <.001 | 0.408 | <.001 |
| ESPHNJ-RS | 0.864 | (0.812–0.901) | <.001 | 0.322 | <.001 |
BIS, bispectral index; CI, confidence interval; ESPHNJ, Niño Jesús Hospital procedural Sedation Scale; ICC, intraclass correlation coefficient; RS, Ramsay Scale; UMSS, University of Michigan Sedation Scale.
The scale was used in 2 hospitals in various settings and was used by 4 professionals in different professional categories.
DiscussionAlthough the ESPHNJ is the scale used most widely in Spain to assess the level of sedation in procedures performed in paediatric patients, we are not aware of any studies performed to assess the validity and the reliability of the ESPHNJ compared to other clinical scales.
Our results show that the ESPHNJ is a valid, reliable and applicable instrument for assessing the level of sedation during invasive procedures with deep sedation/analgesia in paediatric clinical practice.
Level of sedation in the sample and bispectral index valuesThe BIS monitoring values were indicative of moderate, near-deep sedation. This is probably attributable to the sedation protocol applied. One of the key aspects in the use of BIS is the range of values in which the patient should be kept during performance of invasive procedures outside the operating room. Most studies in paediatric patients have identified a value of 70 as indicative of an appropriate level of sedation in patients undergoing invasive procedures with sedation/analgesia.16,30 Agrawal et al.13 recommended a BIS range of 60–90 for invasive and non-invasive procedures in the emergency care setting.
Several studies have suggested that administration of opioids alters the responsiveness of patients to stimuli without altering BIS values.31–33 In the largest paediatric study that compared the UMSS and the BIS, Malviya et al. found a poor correlation between the two when patients received opioid drugs, with high BIS values in patients under moderate or deep sedation.24 The use of fentanyl may have played a role in the weak correlation found between the ESPHNJ, the RS and the UMSS with the BIS in our study, as the mean dose delivered to our patients was higher compared to other studies.
As concerns validity and reliability, the sedation levels used in our sample restrict the generalizability of our findings to patients under moderate to very deep sedation.
ValidityOur study demonstrated that the construct validity of the ESPHNJ is high for the detection of differences in the depth of sedation. This finding is strengthened by the fact that observers were blinded to the timing of administration of the sedative. When it came to the criterion validity, we found a very weak correlation between the ESPHNJ and the BIS, and a moderate correlation between the ESPHNJ and both the UMSS and the RS.
We found moderate interobserver agreement between the paediatrician and the PICU nurse and a low agreement between the anaesthesiologist and the surgical nurse. A possible explanation for the weaker correlation observed between the latter pair is that they may be less familiar with the ESPHNJ compared to the former pair at the HGMC.
In our analysis, we were unable to compare BIS values to discriminate between the different levels of sedation in the three scales and to establish cut-off values for levels sedation relevant to clinical practice, as most of the patients in our sample were under moderate to very deep sedation, which precluded comparisons of BIS values relative to lower levels of sedation.
One relevant finding of our study was that all the sedation scales exhibited a weak or very weak correlation with the objective gold standard for assessing the level of sedation, the BIS. The main reason for this may be the deep level of sedation and analgesia used in our patients, as it is known that clinical scales are more reliable and accurate for mild to moderate levels of sedation but become less precise at deep or very deep levels.
Another explanation for the low correlation between the clinical scales and the BIS is that the BIS correlates to clinical scores of sedation very accurately and reliably, but it does not correlate to measures of analgesia and the response to painful stimuli.13 It is known that the BIS is a poor predictor of motor responses to painful stimuli and is not a good tool to guide adjustment of analgesia,30,34,35 presumably because movement and the response to painful stimuli mainly result from neural activity at the level of the spinal cord, and not at the level of the cortex, which is where it is measured by the BIS.
Due to the weak correlation between the ESPHNJ and BIS, the ROC curves demonstrated that the BIS score had poor discriminatory power in predicting sedation at levels 2, 3 and 4 of the ESPHNJ (Fig. 3).
ReliabilityWe found a good interobserver reliability of the ESPHNJ when compared to the UMSS and the RS, but not in comparison to the BIS. The intraobserver agreement was high. The internal consistency was moderate, which could be attributed in part to the reduce number of items of the ESPHNJ, given that the Cronbach α is known to be affected by the number of items under consideration.36 Compared to the UMSS and the RS, the ESPHNJ was less reliable.
ApplicabilityIn this study, the ESPHNJ was used in 2 different hospitals and 5 different care settings (sedation and analgesia unit, special tests unit, emergency department, PICU and inpatient ward), and was applied by 4 professionals in different professional categories (paediatrician, anaesthesiologist, PICU nurse and surgical nurse). Since this scale has been used in different studies with samples of different characteristics, in different clinical settings and by different types of health care professionals, we consider that is applicability has been proven.
The ESPHNJ is useful in clinical practice, as it is simple and the scores easy to calculate when frequent assessment of sedation is needed. Its greatest advantage is that it does not require the use of stimuli to determine the level of sedation, since it is based on the response to the stimuli involved in the procedure itself. While the guidelines of the ASA call for continuous monitoring of sedation throughout the procedure, assessment of sedation using external stimuli during a procedure is not practical, as noted by Hatch and Sury37 and Malvilla et al.19 While the procedure is underway, when sedation may be at its deepest, continuous pulse oximetry or vital sign monitoring, the ESPHNJ and other scales that do not require stimuli to assess the depth of sedation and capnography may facilitate safe monitoring.19
Limitations and strengthsThe main strength of the study is that we assessed the validity and reliability of the ESPHNJ by comparing it with the gold standards for subjective assessment (clinical scale) and objective assessment (BIS). Another strength is that the study was conducted in 2 hospitals and 5 different care settings and that the scales were applied by 4 professionals in different professional categories that were blinded to the timing of sedative administration. Also, we selected the 150min of video recordings at random out of the total 1188min available, which we believe provided a representative sample of sedation practices in the 2 participating hospitals.
The main limitation of our study is that the sedation levels used in our sample only allow generalisation of our findings to patients subjected to moderate to deep sedation. Thus, further studies in patients subjected to lower levels of sedation are necessary. Still, it is also true that in general the level of sedation required for invasive procedures in paediatric patient ranges from moderate to very deep, depending on the procedure. Another limitation is that the observers did not receive specific training on the use of the 3 scales, which may have had an impact on interobserver agreement.
ConclusionsThe results of our study demonstrate that the ESPHNJ is a valid, reliable and applicable instrument for monitoring sedation during invasive procedures with deep sedation and analgesia in paediatric patients based on the comparison to other sedation scales. The ESPHNJ performed less well compared to the UMSS and the RSS.
Conflicts of interestThe authors have no conflicts of interest to declare.
AcknowledgmentsThe authors thank Dr. Ramón Garrido Palomo, Dr. Pilar Saavedra Hernández, Ms. Miguela García-Cervigón Jaime and Ms. Belén Moreno Gutiérrez for being the observers who have scored the scales.
Please cite this article as: Lozano-Díaz D, Valdivielso Serna A, Garrido Palomo R, Arias-Arias Á, Tárraga López PJ, Martínez Gutiérrez A. Validez y fiabilidad de la escala de sedación para procedimientos del Hospital Niño Jesús bajo sedoanalgesia profunda. An Pediatr (Barc). 2021;94:36–45.
Previous presentation: This study was presented as an oral communication with the title “Validación de la escala de sedación para procedimientos del Hospital Niño Jesús en pediatría” at the XXXIV Congress of the Sociedad Española de Cuidados Intensivos Pediátricos; May 24, 2019; San Sebastian, Spain.