The aim of this study was to assess the usefulness of bedside ultrasound compared to capnography and X-ray for endotracheal intubation in children and newborns.
Materials and methodsHemodynamically stable children intubated in pedriatric and neonatal intensive care unit were included. Endotracheal tube insertion was checked after every intubation attempt by tracheal ultrasound and capnography simultaneously. The endotracheal tube insertion depth was then checked by assessment of lung sliding by thoracic ultrasound. Thereafter, Chest X-ray was performed and interpreted as usual. Time to perform each technique was recorded.
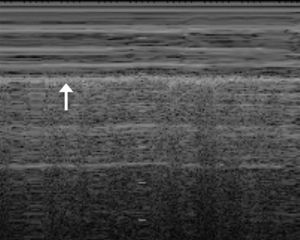
ResultsThe study included 31 intubations in 26 patients (15 in PICU and 16 in NICU). There were no statistically significant differences between tracheal ultrasound and capnography or between thoracic ultrasound and X-ray in identifying the correct endotracheal intubation and assessment of endotracheal tube insertion depth, respectively. Sensibility and specificity of ultrasound compared to capnography were 92% and 100%, and 100% and 75% compared to X-ray. Ultrasound was significantly slower compared to capnography [12 (4–16) vs 6 (3–12)s; P<.001] and significantly quicker compared to X-ray [0.22 (0.17–0.40) vs. 20 (17–25)min, P<.001].
ConclusionsUltrasound appears to be as effective as capnography, although slower, for identifying endotracheal intubation. Ultrasound may be useful in clinical situations, such as cardiopulmonary resuscitation where capnography is less reliable. Ultrasound is as effective as, and quicker than X-ray for assessment of endotracheal tube insertion depth, and it may contribute to decrease the routine use of X-ray after tracheal intubation.
Evaluar la utilidad de la ecografía frente a la capnografía y la radiografía en la intubación traqueal (IT) en niños y neonatos.
Material y métodosSe incluyó a pacientes hemodinámicamente estables intubados en la UCIP y UCIN. Se verificó la posición del tubo endotraqueal (TET) tras cada intubación mediante ecografía traqueal y capnografía. Posteriormente, se comprobó la profundidad del TET por ecografía mediante la visualización de la punta del mismo y el deslizamiento pleural y, posteriormente, con radiografía de tórax. Se cronometraron los tiempos de realización de las técnicas.
ResultadosSe incluyó a 31 intubaciones en 26 pacientes (15 en UCIP y 16 en UCIN). No hubo diferencias significativas entre la ecografía y la capnografía ni entre la ecografía y la radiografía en la detección de la IT ni en la comprobación de la profundidad del TET. La sensibilidad y la especificidad de la ecografía comparada con la capnografía y la radiografía fueron del 92 y el 100%, y del 100 y el 75%, respectivamente. La ecografía fue significativamente más lenta que la capnografía (12 [4–16] vs. 6 [3–12] s; p<0,001) y más rápida que la radiografía (0,22 [0,17–0,40] vs. 20 [17–25] min; p<0,001).
ConclusionesLa ecografía parece tan efectiva como la capnografía, aunque más lenta en la comprobación de la IT. Podría ser de utilidad en situaciones donde la capnografía no sea fiable. La ecografía es tan efectiva y más rápida que la radiografía en la evaluación de la profundidad del TET, por lo que podría disminuir la utilización rutinaria de la radiografía.
Endotracheal intubation (EI) is an essential technique in airway management. However, it can be associated to potentially serious complications, such as unrecognised oesophageal intubation (OI) or one-lung intubation. Consequently, it is important to verify the correct placement and depth of insertion of the endotracheal tube (ETT) after each intubation.1–3 Direct laryngoscopy allows the direct verification of the EI, but it requires proficiency by the operator and the interruption of resuscitation manoeuvres in patients with cardiac arrest.4,5 There are alternative methods such as auscultation, capnography, observation of chest movements, observation of condensation in the ETT, and raising the heart rate in neonates.6 Although none of the existing methods have been proven to be fully reliable, capnography is the most widely used and recommended.7 Chest radiography is routinely performed in most units to check the correct placement of the tip of the ETT after intubation. There is still little experience in the use of ultrasound in paediatric intubation. Studies in adults seem to suggest that ultrasonography is as reliable and fast as conventional methods and could be advantageous in specific situations, such as cardiopulmonary arrest.3,8–10
The purpose of our study was to assess the feasibility and efficacy of ultrasonography in EI compared with the most widely used methods, such as capnography or chest radiography.
Materials and methodsStudy designWe conducted a diagnostic validation study between January 2011 and June 2013. The study included patients admitted to the paediatric and neonatal intensive care units who required intubation at a time when the researcher in charge of performing the ultrasound tests was available. None of the patients were undergoing cardiac arrest and all were haemodynamically stable. The protocol of the study was approved by the clinical research ethics committee of the hospital, and we obtained signed informed consent from the parents or legal guardians.
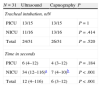
Ultrasound performance and interpretationUltrasound was performed with a portable device (Vivid i, General Electrics, Atlanta, United States) fitted with an 8Hz microconvex array transducer and a 12Hz linear array transducer, recommended for their capacity to generate detailed images of superficial structures. Because of its small size, the microconvex transducer was used in infants younger than 1 year, and the linear transducer was used in children older than 1 year. The transducer was placed superior to the suprasternal notch with the neck slightly extended for the tracheal ultrasound (Fig. 1), longitudinally along the mid-axillary line on either hemithorax for the chest ultrasound.
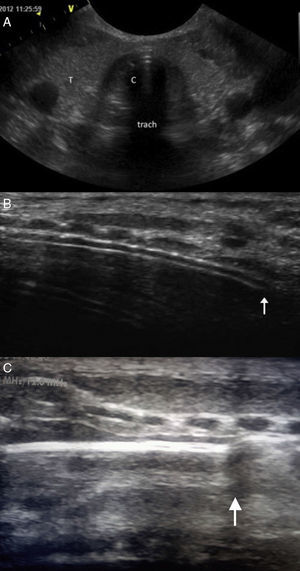
When the ETT is inside the trachea, the transverse ultrasound shows a double tract sign produced by the interface between the air and the ETT, giving rise to a “comet tail” artefact (Fig. 2A). The presence of this artefact has shown a sensitivity of 100% in several studies.11 In OI the comet tail is not seen, and at times the ETT can be visualised in the oesophagus in a paratracheal position, although this is not a constant finding. In the longitudinal view, EI generates an echogenic double tract sign along the trachea immediately posterior to the tracheal rings that is not seen in OI (Fig. 2B). If the ETT is in the extrathoracic trachea (superior malposition) the tip of the ETT is seen along with a posterior acoustic shadow that corresponds to the air in the trachea (Fig. 2C). The correct depth of insertion of the ETT is confirmed by 2-D mode chest ultrasound, which allows the assessment of lung sliding, understood as visualisation of the visceral pleura sliding against the parietal pleura in an expanded chest. The presence of bilateral, symmetrical sliding rules out one-lung intubation.12,13 In M-mode, normal lung sliding generates the so-called “seashore sign” (Fig. 3). The absence of the sliding lung sign is not specific of one-lung intubation, and it is important to be aware that it also appears in pneumothorax, large atelectases, and pulmonary consolidation with restricted movement on insufflation.12,14.
(A) Transverse plane: hyperechogenic shadowing or “comet tail” sign (C) visible in ET. (B) Longitudinal plane: double track echogenic line corresponding to the ETT (arrow) posterior to tracheal rings. (C) In cases of superior malposition, a posterior acoustic shadow corresponding to the air in the trachea can be visualised (arrow). T: thyroid; Trach: trachea.
The study protocol was divided into 2 phases: (1) intubation with simultaneous confirmation using capnography and tracheal ultrasound, and (2) Determination of ETT placement with chest ultrasound and chest X-ray. The attending physician performed the intubation. A paediatrician with 5 years’ experience in ultranonography performed all the ultrasounds, and a second researcher timed how long it took to perform each technique. The recorded times did not include the start-up time of the ultrasound machine nor the time spent in the set-up and calibration of the capnography device. The time spent in the radiograph spanned from the time it was requested to the time it was read in the computer terminals of the unit. The information obtained by ultrasound was not shared with the attending physician to avoid influencing his clinical perspective. Table 1 shows the chronological diagram of the study protocol.
Chronology of the study protocol.
| 1st stage: determination of intubation | |
| Tracheal ultrasound | Capnography |
| Transverse planeLongitudinal planeTip of the ETT | Set up≥3 normal waveforms with plateaus |
| Securing ETT |
| 2nd stage: determination of ETT insertion depth |
| Chest radiography request |
| Chest ultrasoundSliding lung signSeashore sign |
| Chest radiography interpretation |
Capnography identification of EI was defined as the presence of 3 or more consecutive waveforms with a clearly identifiable plateau during ventilation with a bag-valve mask. Correct placement of the ETT was defined as radiography showing the distal end of the ETT at about 2cm above the carina. In radiography, superior malposition was defined as position of the ETT above the sternoclavicular articulation, and one-lung intubation as the ETT seen at the opening or inside the right mainstem bronchus.
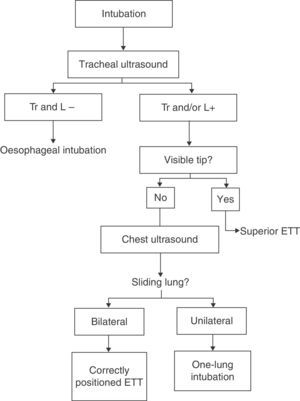
We considered that EI was identified by ultrasound when one of the characteristic ultrasound signs mentioned above was found in one of the examined planes. The insertion depth of the ETT was considered correct when the tip of the ETT was not seen in the extrathoracic trachea in the longitudinal view, and when a bilateral sliding lung was clearly identified in chest ultrasound. When the tip of the ETT was observed in the longitudinal ultrasound it was considered a sign of superior malposition, and if unilateral lung sliding on the right was observed, it was considered a sign of one-lung intubation. The algorithm proposed for the use of ultrasound in EI is shown in Fig. 4.
Statistical analysisQuantitative data are expressed as median and range, and qualitative data as relative frequencies (n/N). We compared the frequency of EIs determined by capnography with the frequency determined by ultrasound, and the number of correct placements determined by ultrasound with the number determined by radiography. We also compared the time it took to perform the different procedures. Comparisons were made for the results of the subsets of patients in the PICU and NICU. We used nonparametric tests (Wilcoxon matched pairs test, and Mann–Whitney U test for independent samples) and the chi-squared test. The statistical significance was set at P<.05.
ResultsThe sample included 31 intubations in 26 patients. Thirteen were neonates in the NICU with a median gestational age of 32 weeks (range, 24–40 weeks) and a median weight of 1438g (range, 530–3450g). There were 13 children in the PICU with a median age of 4 years (range, 3 months–14 years) and a median weight of 21kg (range, 4–58kg). Tables 2 and 3 summarise the results of the capnography vs ultrasonography and the radiography vs ultrasonography comparisons. We found no significant differences in the ability to detect EI between capnography and ultrasound in NICU or PICU patients; however, ultrasound was significantly slower, a difference that was not observed in the PICU patient subset. We found no significant differences between radiography and ultrasound either. The ETT was not visualised by means of ultrasound in 2 neonates with positive capnography. On the other hand, ultrasound did not detect 2 malpositions (ETT placed too high) that were detected in the radiograph. Using capnography as the standard criterion, ultrasonography showed a sensitivity of 92% and a specificity of 100% in detecting the presence of the ETT in the trachea. Ultrasonography also showed a sensitivity of 100% and a specificity of 75% compared to radiography in detecting the correct depth of insertion of the ETT. Ultrasonography was significantly faster than radiography in every comparison.
Comparison of ultrasound and capnography in identification of tracheal intubation.
Comparison of ultrasonography and radiography in confirmation of ETT position.
Ultrasonography has been used in airway management to investigate anatomy, estimate the size of the ETT, verify ETT placement, and detect one-lung intubation.5,15–20 We believe that one of the most interesting aspects of ultrasound is that, besides visualisation of the ETT, it allows evaluation of its insertion depth and ruling out incorrect placement.
The aim of our study was to compare the usefulness of ultrasonography to identify EI with other, more widely used methods, such as capnography and chest radiography. We found that ultrasonography is efficacious in the identification of EI, with high sensitivity and specificity compared to capnography. However, it is a considerably slower method. We must highlight that the difference in time was observed in the NICU group. This is probably due to the small size of neck structures in neonates, which makes it more difficult to implement the technique. In older children, ultrasonography was as quick as capnography. Since it is safe and fast, capnography is currently the most widely used method to confirm EI.7,11 However, it may not be reliable in patients with cardiopulmonary arrest due to an insufficient tidal volume. In this context, ultrasound can be advantageous in emergent intubations. Studies with large samples conducted by Sim et al.12 and Chou et al.9 have demonstrated that ultrasound performed better than capnography in patients with cardiopulmonary arrest. Furthermore, we found that ultrasound is as fast as capnography in older children, which suggests it may be useful under these circumstances, in which reliability and speed are crucial.
Other situations in which ultrasound can offer advantages over capnography are low tidal volume, for instance in premature neonates, or the presence of severe bronchospasm. In the absence of these special circumstances, if capnography is available, ultrasound should not be used or should be used only as an adjunct technique. We also observed that performing this technique in neonates presented more difficulty, which may be the reason why the ETT was not visualised in 2 neonates that had been intubated correctly (false negatives). Finally, superior malposition of the ETT was not detected in 2 neonates. These aspects need to be taken into account when considering the use of ultrasound in neonates, especially if the operator is inexperienced.
Ultrasound was as efficacious as chest radiography both in the PICU and the NICU, with high sensibility and moderate specificity. The false negatives in our study corresponded to nondetection of the superior malposition of the ETT in neonates using ultrasound. This may have been due to the small size of the neck, which makes it difficult to determine whether the tip of the ETT is or is not in the extrathoracic trachea. Ultrasound clearly required less time than radiography. This finding was also reported by Sim et al.12 in the adult population and by Kerrey et al.21 and Galicinao et al.5 in children. Another study on adults conducted by Pfeiffer et al.3,10 showed that ultrasound is as quick as auscultation and outperforms capnography combined with auscultation in determining the placement of the ETT. Another advantage of ultrasound compared to radiography is that in situations where the ETT may be displaced by patient handling, ultrasound can be used to verify its placement as many times as needed without associated exposure to radiation.
There is little experience in the use of ultrasound to confirm ETT placement in the paediatric age group. Kerrey et al.21 reported that ultrasound is equivalent to chest radiography in determining the position of the ETT within the airway. It is worth noting that the ultrasound technicians in this study were inexperienced. Previous research shows that ultrasound can be used reliably by prehospital care providers with little training.22 Later, a paediatric study by Galicinao et al.5 showed a 100% sensitivity and specificity of ultrasound when compared to clinical detection methods and chest radiography. This study also compared ultrasound with capnography and concluded that ultrasound should be considered an adjunct method that offers some advantages in specific situations. We believe that ultrasonography can be useful to verify ETT placement and rule out malposition in a timely manner after intubation, avoiding routine performance of chest radiography, especially in older children. Our results suggest that in neonates, if there are any signs of superior malposition (such as excessive leaks from the ventilator), ultrasound may not be sufficient, and a radiograph needs to be performed.
The main strengths of our study are its prospective nature, that a single operator performed all ultrasounds, and that it is the first study simultaneously comparing ultrasonography with other standard methods, like radiography and capnography, in children and neonates. The main limitation is the small number of patients included in the study, as well as their heterogeneity. Another limitation is that the study was performed in the controlled environment of the ICU, where the number of oesophageal intubations or incorrectly placed ETTs tends to be low. This may limit the generalisability of its results to other settings, such as prehospital or emergency care.
Future research should assess the role of ultrasonography in airway management, specifically in the context of cardiopulmonary arrest of haemodynamic instability. Ideally, it would entail multicentre studies in large-volume paediatric hospitals.
ConclusionsUltrasound is as efficacious as capnography in verifying ETT placement, although it may take more time, especially in neonates. Other disadvantages in neonates are that it may produce false negatives, and that it is difficult to identify superior malposition. Ultrasound is an efficacious and fast method for determining the depth of insertion of the ETT and ruling out one-lung intubation, so it could contribute to reduce the routine use of radiography.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Alonso Quintela P, Oulego Erroz I, Mora Matilla M, Rodríguez Blanco S, Mata Zubillaga D, Regueras Santos L. Utilidad de la ecografía comparada con la capnografía y la radiografía en la intubación traqueal. An Pediatr (Barc). 2014;81:283–288.